Every person has moles on their skin. The medical name for these dark spots is nevi. They can be congenital or acquired at a certain stage of life.
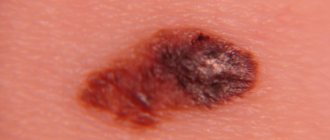
Dysplastic nevus is a pigmented skin neoplasm that has a tendency to malignancy. Clinically it looks like a mole of varying sizes with bizarre borders, heterogeneously colored in brown and black tones.
Dysplastic nevus - what is it?
Like most moles in humans, a dysplastic (atypical) nevus is a pigmented nevus consisting of nevus cells. These cells are very similar to melanocytes. They also secrete the brown pigment “melanin”, but they differ in a number of characteristics that are not of fundamental importance to us.
It is important to note that dysplastic nevus is a histological diagnosis. This means that not all moles that look dysplastic in appearance will actually turn out to be dysplastic after removal and examination.
What does it look like
Externally, the tumor is very similar to an ordinary mole, but due to the fact that melanin is distributed unevenly, the nevus can be colored in different shades of brown - from light to darker tones.
In the central part, the formation has the darkest shade. These are melanoform nevi of the scalp and neck, manifested as single or multiple formations.
The diameter of the formations can reach 10 mm or even more, which distinguishes dysplastic nevi from other skin neoplasms. A complex melanocytic nevus has a heterogeneous surface - it is smooth at the edges, and, on the contrary, bumpy in the center. The central part of the nodule is slightly elevated above the surface of the skin.
How to distinguish a regular mole from a dysplastic nevus?
Atypical nevi have a number of characteristic features that can occur either individually or in combination with each other.
| Round, symmetrical shape | Uneven edge and/or asymmetrical shape |
| Completely flat or completely raised above the skin | One part can be raised, the other flat (fried egg) |
| Uniform color or shades of brown | Black, red, brown at the same time |
| Size less than 6mm | Size over 6mm |
| Localization on any part of the body | Rarely located on the face |
Diagnostics, difference from other formations
The resulting cutaneous element, one or several, must be shown to a dermatologist. Only a specialist can determine the degree of risk of malignant transformation of the nevus, the need for further observation or removal.
To diagnose Clark's nevus, an experienced specialist only needs to conduct a visual examination of the formation.
To exclude malignancy, the patient is prescribed the following diagnostic tests:
- Dermatoscopy. The procedure involves a thorough examination of the elements using a dermatoscope, which magnifies the image. The purpose of the examination is to detect the slightest changes in the mole. The examination is carried out quickly, painlessly and is highly informative for the patient’s initial and repeated visits. Dermatoscopy does not provide a 100% chance of confirming the diagnosis, but it can tell the specialist which examinations in the future will be the most rational. Recently, digital dermatoscopes have been used.
- Echography. It is used infrequently: with large cutaneous elements to exclude malignant growth of a nevus into all layers of the skin or during preoperative preparation to determine the boundaries of a large mole.
- Indication by phosphorus isotope. A highly informative method for diagnosing oncological degeneration of a tumor. Melanoma actively accumulates radioactive phosphorus, since active cell division processes occur in the tumor, in which this element participates. During malignant transformation, the scanner detects intense accumulation of the isotope in the area of formation.
- Local thermometry. The technique involves measuring the temperature on the surface of the skin using a special apparatus. As the formation grows, active metabolism occurs, accompanied by a slight increase in temperature in this area. During the examination, temperature data obtained from measurements on the surface of the nevus and clean skin are compared. A benign formation will show a difference within 1 °C; with malignant neoplasia, the difference will be higher - up to 2.5 °C. This technique is often used in the follow-up of patients with dysplastic nevi.
- Biopsy. The most reliable method for diagnosing signs of cancer transformation. A biopsy is the removal of a piece of tissue from a nevus and subsequent microscopic analysis of the sample. A characteristic histological sign of Clark's nevus is atypical proliferation of melanocytes, that is, its chaotic growths in the dermis and epidermis. Two types of examination are used: puncture biopsy, when a sample is obtained with a needle after preliminary anesthesia (the method has limited information content, since cells are taken pointwise and in small quantities);
- a total excisional biopsy, when the entire nevus removed during the operation is examined; if histological signs of oncology are detected, the patient is prescribed chemotherapy.
Blood and urine tests are not used to diagnose atypical nevi, since there are no changes in indicators with such pathology. Clinical and biochemical studies of biological fluids can be carried out before surgical removal of the nevus to assess the functionality of the internal organs.
Differential diagnosis
First of all, a benign Clark nevus is differentiated from the following formations:
- melanoma, which is clinically indistinguishable from a nevus, so a histological examination is necessary;
- Dubreuil's melanosis (lentigo maligna) - a melanoma-dangerous nevus that forms mainly in older people and is a single element with uneven contours located on an open area of the body; the color of the formation can be different - from yellow-brown to black; can reach very large sizes - up to 20 cm;
- acquired nevomelanocytic nevus - a mole with a uniform color of different shades, usually of regular shape, clear boundaries, small in size (up to 6 mm);
- Spitz nevus (benign juvenile melanoma) - a fast-growing birthmark with a smooth (most often) surface, round and convex shape, different colors (pink, yellow, brown) and a fairly large size - up to 2 cm;
- seborrheic keratosis - multiple elements that appear in adults mainly on the back or chest, forearms; keratomas have a round shape, different colors, resemble warts, covered with a thin crust, prone to bleeding; the size of the elements is from 2 to 6 mm, may be accompanied by itching;
- solar lentigo - brownish spots on exposed skin that appear under the influence of ultraviolet radiation in people over 50 years of age (more often in men).
Since there is a high probability of Clark’s nevus acquiring malignant properties (especially in the familial, multiple type), you need to know the first signs of malignancy:
- an increase in the size of the nevus - proliferation of the peripheral borders;
- the appearance of a reddish border around the formation;
- thickening of healthy skin around the mole;
- the appearance of itching;
- color change - darkening;
- change in texture (compaction), the appearance of dryness, roughness, cracks on the surface of the nevus.
How to distinguish a dysplastic nevus from melanoma?
A theoretically prepared reader, after reading the table, will exclaim: “You have now listed almost all the symptoms of melanoma!!! How can you tell them apart???” Unfortunately, a person without experience in diagnosing skin cancer, as a rule, cannot do this.
If you find moles on your skin with signs of dysplastic nevi, you need to see an oncologist. This doctor will examine them and also tell you about the signs of nevi turning into melanoma and the principles of monitoring such formations.
Diagnosis
It is determined by a dermatologist according to dermatoscopy (examination through a magnifying glass). If necessary, additional examination: dermatobiopsy and histological examination.
Most often, a correct diagnosis can be made based on dermatoscopy data, especially if there is evidence of melanoma (malignant nevus).
Clark's nevus on dermatoscopy
On video: case from practice No. 3. Watch from 2 minutes and 34 seconds. A woman has signs of Clark's nevus turning into melanoma.
It should be differentiated: with borderline nevus, with fibroepithelial nevus, with basal cell carcinoma and melanoma.
Dysplastic nevus syndrome
Unfortunately, there is a syndrome that in Russian literature is often called nevus dysplastic syndrome (in foreign literature - FAMMM).
This disease has 2 diagnostic criteria
- the number of dysplastic nevi on the skin is more than 50
- melanoma in relatives
This disease may be associated with a mutation in the CDKN2A gene, which also increases the risk of developing pancreatic cancer
With this syndrome, the risk of developing melanoma, according to different authors, varies from 56 to 100%. The disease requires regular (once every few months) monitoring by an oncologist.
Treatment of pathology
Pigmented dysplastic nevus cannot be treated with medications or traditional medicine. Any such tumor must be surgically removed using a scalpel as a preventative measure. This applies to moles that are located in small numbers in areas where it is inconvenient to conduct frequent medical examinations.
If there are more than two dysplastic nevi on the patient’s body, it is not recommended to remove all of them to prevent the development of skin cancer. In this case, you should only regularly see a doctor at least once every six months, so that at the first signs of degeneration of the mole, you can immediately remove it without harm to the patient. If you begin to remove such tumors as a preventive measure, this will lead to a less than aesthetically pleasing appearance, especially in the face and open areas of the body, since the scalpel will leave scars.
It should also be noted that no other hardware method of mole removal is suitable for getting rid of Clark’s nevus. Modern methods - cryodestruction, laser removal, radioknife and others - will not be able to provide such a high probability of preventing relapse and other possible complications. A reappearing tumor must be urgently surgically removed, which negatively affects the patient’s condition if the previous operation was performed recently. The risk of melanoma after a relapse increases significantly, so doctors do not even consider the option of removing a dysplastic nevus using hardware methods.
What to do if there are dysplastic nevi on the skin?
There is an opinion on the Internet that “all dysplastic nevi should be removed.” I consider this point of view incorrect for the following reasons:
- A very small percentage of nevi that look atypical upon examination turn out to be so upon histological examination.
- An even smaller proportion (0.0001%) of truly dysplastic nevi have a chance of becoming melanoma
- Skin melanoma can develop not from a nevus, but against the background of unchanged skin.
In this regard, for people who have dysplastic nevi, I usually recommend the following:
- Regular self-examination once a month with measurement of existing atypical nevi using a ruler. Optimally - with photographic recording of the result
- Examination by an oncologist once every 6 or 12 months. The frequency depends on the number of nevi.
- It makes sense to remove elements that are difficult to access for self-examination, as well as those that have changed in a short time
- Protect skin from the sun
Causes of Clark's nevus
Atypical moles are formed due to local movement of pigment cells under the influence of reasons that are not fully understood.
The pigment melanin, which is produced by melanocytes located in different layers of the dermis, determines the shade of the skin and is designed to protect it from the harmful effects of insolation (ultraviolet radiation).
In this case, the pigment is found in all skin structures in the same amount. But in people with a predisposition during fetal development or immediately after birth, melanocytes filled with melanin migrate to various areas of the skin.
Atypical familial birthmarks are formed - small formations that begin to gradually grow during puberty and become clearly visible.
Sporadic (single) nevi occur in a different scenario. Most researchers believe that ultraviolet radiation and the human papillomavirus play a certain role in the mutation and proliferation (accelerated cell division) of pigment cells.
The provocateur of the movement and point accumulation of melanocytes is always sharp hormonal changes - the onset of puberty, pregnancy, etc.
In contrast to the theory that it is insolation that is the main trigger for the development of a sporadic form of pathology, some doctors cite the fact: in many cases, atypical nevi appear in places where direct rays of the sun do not reach, for example, in the perineum, on the genitals or scalp under hair.
It is possible that a significant decrease in the body’s defenses plays some role in the formation of dysplastic nevi, since cases of numerous atypical moles have been reported in connection with skin blistering diseases and some other pathologies that cause immunosuppression (immune suppression).
The risk group for familial dysplastic nevus includes immediate relatives of carriers of atypical moles.
It has been proven that the predisposition to the appearance of formations is transmitted in an autosomal dominant manner. Whether a child will develop nevi or not largely depends on the characteristics of his body and the influence of external factors. The closer the relationship with carriers of the pathology, the higher the likelihood of developing multiple nevus syndrome.
The risk of malignancy of Clark's nevus exists due to the persistence of proliferative activity (readiness for increased division) of immature melanocytes in the epidermis and the presence of cell atypia of varying severity.
Briefly about the main thing:
A dysplastic nevus actually has a higher chance of developing into melanoma than a regular nevus. However, both of these figures, in my opinion, are in the realm of statistical errors. Typically, for dysplastic nevi, I recommend regular self-examination, examination by an oncologist, and removal of nevi that are difficult to observe.
Other articles:
- Large mole - should you worry?
- Which moles are SAFE?
- Find out your chance of getting melanoma!
- Can melanoma appear after mole removal?
Useful article? Repost on your social network!
Diagnostic features
At the slightest suspicion of the development of nevi, you should immediately contact a dermato-oncologist for a diagnostic examination. To make an accurate diagnosis, the patient may be prescribed the following procedures:
- dermatoscopy – visual examination of skin formations without surgical intervention;
- biopsy of the skin element - taking a biopath for laboratory analysis;
- cytological analysis of a dermatological formation, for which the doctor takes a scraping or smear from the surface of the nevus under study;
- immunohistochemistry is a microscopic examination of tissue that allows you to check the formation for malignancy, as well as determine the phenotype of the mole.
Monitoring the status of a dysplastic formation is an important process, since this formation is something between a benign tumor and melanoma. Timely diagnostics will allow us to determine the transformation process at the initial stage.
Possible complications
You need to be careful with moles. Even though they do not pose any danger to humans, when exposed to certain factors, dysplastic nevus can lead to serious complications. One of the most dangerous of them is the development of the process of malignancy (this may be indicated by a change in the color, size or structure of the formation).
If a nevus appears in a place of direct contact with clothing, then over time the formation may become damaged. In this case, an inflammatory process begins, which without timely medical care leads to more serious consequences.
Course and prognosis
Dysplastic melanocytic nevus may progress to melanoma
Dysplastic melanocytic nevus may be stable, progress to melanoma, or regress. The factors responsible for the progression of dysplastic melanocytic nevus to melanoma are unclear, but are likely genetic as well as environmental factors. The most significant study related to dysplastic melanocytic nevus developing into melanoma was a study of 14 families of melanoma-prone relatives. Over the course of 4 years, 128 melanomas were diagnosed in 69 members of these families.
People with a dysplastic melanocytic nevus with a family history of melanoma have a 56% chance of developing melanoma between the ages of 20 and 59 years, and a 100% chance of developing melanoma by age 76 years. In these individuals, even the presence of only a dysplastic melanocytic nevus is a reliable risk factor for the development of melanoma. Moreover, in patients with dysplastic melanocytic nevus who are difficult to tan and often receive sunburn, the risk of developing melanoma is higher. In contrast, the risk of melanoma in blood relatives who did not have dysplastic melanocytic nevus or melanoma. no higher than in the population. As for dysplastic melanocytic nevus without a family predisposition, it can be both a marker of the risk of developing melanoma and its potential precursor.
In general, people with dysplastic melanocytic nevus (regardless of a family history of melanoma or dysplastic melanocytic nevus) have a 7-70-fold increased risk of developing melanoma.
Their risk of developing this tumor during their lifetime is almost 18%. Moreover, the role of dysplastic melanocytic nevus as a precursor of melanoma is confirmed by the histological combination of dysplastic melanocytic nevus and melanoma in 10-70% of tumors. One study showed that the potential risk of melanoma in the presence of 1-5 dysplastic melanocytic nevi increased by 3.8 times, and in the presence of 6 or more dysplastic melanocytic nevi increased by 6.8 times.
The presence of any dysplastic melanocytic nevus in a patient with melanoma increases the risk of developing another melanoma by 6 times, and the presence of two or more dysplastic melanocytic nevi increases the risk of developing another melanoma by 9 times. Because, as discussed above, immunosuppression itself is an important risk factor for melanoma, patients with dysplastic melanocytic nevus and immunosuppression may have an even higher risk of developing melanoma. The connection between dysplastic melanocytic nevus and other malignant tumors has not been proven.
Location
The location of birthmarks occurs on areas of the body that are not exposed to daily sun exposure:
- genital skin;
- chest skin;
- back skin.
Many patients experience the formation of complex formations that have a number of characteristic features:
- the stain has 2 parts;
- in the center of the spot - a benign neoplasm;
- at the edges of the nevus there is a melanocytic component.
The number of melanocytes in the nevus varies, but there are few atypical cells.
The role of external influences and internal features of the development of the organism
The presence of sporadic cases makes us talk about these factors as the causes of the appearance of dysplastic nevi. Moreover, neither close nor distant relatives of the carrier of such nevi have signs of mole dysplasia. This means that not only the hereditary factor contributes to their development.
The maximum appearance of dysplastic nevi has been recorded during puberty and in a young growing body. This phenomenon can be explained by the influence of fluctuations in sex hormones on the degree of differentiation of skin melanocytes, which did not manifest themselves in the form of moles in earlier periods.
External factors in the form of excessive exposure to direct sunlight and artificial sources of ultraviolet rays are of secondary importance and are not capable of independently causing the appearance of dysplastic nevi.