About dermatitis Symptoms Types of dermatitis Treatment of dermatitis
Many skin diseases present with similar symptoms, making diagnosis and choosing the right treatment difficult. In particular, such similar pathologies are dermatitis and eczema. Both of these diseases are characterized by moist rashes with itching, blisters and crusts, both develop due to the action of irritating factors. And yet these are two different nosologies. What is the difference between eczema and dermatitis? Why are these two conditions classified as two different diseases?
Types of atopic eczema
There are several types of eczema. They differ in clinical picture and factors involved in the development of the disease.
Atopic eczema may have:
- The true form is that contact with a substance that provokes an allergic reaction leads to the appearance of rashes on the hands (especially on the surface of the hands), face, and feet. The skin in the affected area becomes covered with small blisters containing serous contents. After some time, they burst, leaving a weeping and very painful surface.
- Microbial form - localized on the wound, burn surface, trophic ulcers affected by the inflammatory process or infected. Damaged skin becomes covered with crusts with a yellowish or greenish tint. When the crust is removed, red, moist, sometimes bleeding areas with clear boundaries are revealed. Foci of inflammation are located asymmetrically and can spread to the adjacent area.
- Seborrheic form - inflamed areas are localized in places with intense sebum secretion: on the scalp, in the ears, in the axillary area, on the back. Occurs with increased activity of a fungal infection in combination with disruption of the sebaceous glands. Nodular rashes covered with greasy crusts are observed on the skin. During an exacerbation, hyperemia and swelling in the affected area are sometimes noted; in the advanced stage, the formation of weeping erosions is possible.
- Professional uniform - occurs as a result of constant contact with harmful substances in the workplace, prolonged exposure to solar insolation or low temperatures. It manifests itself as itching, dry or serous rash, swelling in the affected area, and occasionally weeping erosions appear. If left untreated, lesions spread over the surface of the body.
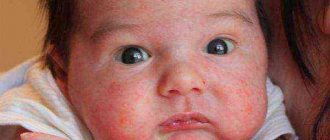
- Childhood form - occurs in infancy with improper treatment of atopic dermatitis. A small rash covers the forehead, cheeks, and skin folds; wet wounds form at the site of the rash. Subsequently, the inflammatory process covers the surface of the skin in the back, arms, buttocks, and feet.
general description
The disease atopic dermatitis is an inflammatory, chronic skin lesion that is clinically manifested by severe itching, dryness and irritation of the skin.
Atopic dermatitis causes significant discomfort to the patient and reduces the quality of life. Strong, constant scratching of itchy skin can lead to a secondary infection, which worsens the prognosis.
According to statistics, 12% of the population suffers from the disease. Despite the fact that medicine has advanced significantly in recent years, the treatment of atopic dermatitis is still a rather complex problem and requires clear and well-coordinated collaboration between the doctor and the patient.
Causes of atopic eczema
People who have a genetic predisposition to allergization of the body are characterized by an increased level of immunoglobulin E in the blood. In the normal state of the immune system, this protein takes part in neutralizing various types of infection. But if there is a failure in it, his behavior becomes aggressive.
Immunoglobulin E combines into a single complex with the allergen and affects healthy tissues of the body. With the development of eczema, this is manifested by the appearance of rashes on the skin and a number of accompanying symptoms.
Difference between eczema and atopic dermatitis
Atopic dermatitis and eczema have different causes. The similarity of these diseases is the damage to the skin by the inflammatory process. But with dermatitis it is caused by external irritants, and with eczema it is caused by the action of allergens.
An allergic reaction can be caused by:
- microorganisms (bacteria, viruses);
- constant friction of the surface against clothing or other objects;
- inflammatory processes in internal organs (rhinitis, tonsillitis, bronchitis, etc.);
- scratching the skin;
- inhalation of dust particles, plant pollen, pet hair;
- food products;
- medicines;
- cosmetics;
- insufficient compliance with hygiene rules;
- hormonal imbalance.
Atopic dermatitis often develops first, manifesting itself as acute inflammation of certain areas of the skin.
This disease usually affects children; when it appears in infants, it is called diathesis. Then they become covered with bubbles, peeling occurs with the formation of crusts. These symptoms indicate the development of chronic atopic eczema.
An additional difference between these diseases is that with dermatitis there are no blisters or weeping erosions. Recovery occurs immediately after contact with the allergen is eliminated. Dermatitis from eczema also differs in the nature of the rashes - they are located evenly over the entire affected area, the focus of inflammation has clear boundaries, standing out against the background of healthy skin.
Lifestyle and Home Remedies
To help reduce itching and soothe inflamed skin, try these self-care measures:
- Moisturize your skin at least twice a day. Find a product or combination of products that works for you. You can try oil baths, creams, ointments or sprays. For a child, a twice-daily regimen might be an ointment before bed and a cream before school. Ointments are more fatty, and less when applied.
- Apply anti-itch cream to the affected area. Over-the-counter hydrocortisone cream containing at least 1 percent hydrocortisone may temporarily relieve itching. Apply it no more than twice daily to the affected area after moisturizing. Using a moisturizer first helps the medicated cream penetrate the skin better. Once your reaction improves, you can use this type of cream less frequently to prevent flare-ups.
- Take oral allergy or anti-itch medications. Options include over-the-counter medications (antihistamines) such as cetirizine (Zyrtec) or fexofenadine (Allegra). Additionally, diphenhydramine (Benadryl, others) may be helpful if the itching is severe. But it makes you drowsy, so it's better for sleep.
- Don't scratch. Instead of scratching the itch, try pressing on the skin. Cover the itchy area if you can't help but scratch it. For children, it may help to trim their nails and wear socks at night.
- Apply bandages. Covering the affected area with bandages helps protect the skin and prevent scratching.
- Take a warm bath. Sprinkle your bath water with baking soda, raw oatmeal, or colloidal oatmeal, a finely ground oatmeal prepared for bath use (Aveeno, others). Soak for 10-15 minutes, then wipe. Apply moisturizer while skin is still damp.
- Choose a mild soap without dyes or perfumes. Use soap that is super rich and non-alkaline. Be sure to rinse the soap completely.
- Use a humidifier. Hot, dry indoor air can dry out sensitive skin and worsen itching and flaking. A portable home humidifier or one attached to your furnace adds moisture to the air inside your home.
- Wear cool, smooth, textured clothing. Reduce irritation by avoiding clothing that is rough, tight or scratchy. Also, wear appropriate clothing in hot weather or during exercise to prevent excessive sweating.
- Satisfy stress and anxiety. Stress and other emotional disorders can make atopic dermatitis worse. Acknowledging those who are trying to improve their emotional health can help.
How does neurodermatitis differ from eczema and dermatitis?
Just like atopic eczema, dermatitis and neurodermatitis are inflammatory skin lesions. The difference between these pathologies is that not only an allergic, but also a neurogenic component is involved in their development. Neurodermatitis is accompanied by vegetative-vascular dystonia and occurs with periods of remissions and exacerbations. Characteristic of this disease is unbearable itching, which intensifies at night, causing insomnia, irritability and increased nervous excitability.
Let's take a closer look at how atopic eczema differs from neurodermatitis:
| Characteristics of differences | Atopic eczema | Neurodermatitis |
| Shade of rashes | Reddish | White |
| Nervous system | Violations are mild | There are disorders, increased nervous excitability |
| Form of rash | Bubbles, small nodules, punctate erosions | Nodules predominate, their fusion is possible |
| Seasonality of exacerbations | Celebrated mainly in winter and spring | Occurs more often in late autumn and winter |
| Prevalence of lesions | Distribution of foci of inflammation in different parts of the body | Selected areas of skin |
| Effect on body weight | Does not affect | In severe cases of the disease, weight loss is possible |
Video about dermatitis
Eczema is a chronic skin disease that occurs with periods of exacerbations and remissions. It is based on inflammation, which goes through several stages: hyperemia (redness), formation of nodules (papular), vesicles (vesicular), after opening the vesicles, weeping occurs, crusts form and the final stage is peeling. The clinical picture of eczema and atopic dermatitis has many similarities. This is severe itching, due to which a person scratches the skin, rash, and sensitization of the body. Let's try to figure out the difference between eczema and atopic dermatitis.
Treatment of eczema and dermatitis
Since these diseases are allergic in nature, it is necessary to completely eliminate the possibility of contact with the types of allergens that cause them. A sick person should balance his emotional state and avoid stressful situations. People with a predisposition to allergies are advised to exclude from their wardrobe clothes made from synthetic fabrics and wool. To wash things, it is better to use soap rather than powder containing a large amount of chemically active substances.
The best way to prevent the occurrence of diathesis in children is breastfeeding. Mother's milk contains substances that protect the baby's body from infectious diseases, allergens and other unfavorable factors. Dermatitis in a child can occur due to contact with the latex from which nipples are made, as well as some materials used to make toys. Very often, eczema is caused by eating foods that cause food allergies. They can be identified by gradual introduction into the diet against the background of a hypoallergenic diet.
Conservative therapy
For eczema and dermatitis, treatment with medications is based on relieving inflammation and restoring the functions of the skin. To eliminate the increased sensitivity of the body, calcium chloride or sodium thiosulfate is prescribed. Antihistamines Zyrtec and Suprastin help prevent the release of histamine, which is involved in the occurrence of rashes and itching. The use of sedatives based on valerian, lemon balm, and motherwort (Novopassit, valerian extract) will help relieve nervous tension and improve sleep.
For atopic eczema, treatment of the skin in areas of inflammation is carried out with topical hormonal ointments (Advantan, Hydrocortisone). They should be prescribed by a doctor. If the surface becomes infected, an ointment with antimicrobial activity (Fusiderm, Oxycort) is applied to the skin. Drying of the affected areas is provided by lotions with Furacillin or a solution of Boric acid. Infants are recommended to treat lesions with Fucarcin.
Use of herbal remedies
Traditional medicine and herbal medicine recommend treating eczema and dermatitis with lotions made from infusions of leaves of stinging nettle, mallow, elderberry, arnica, hops, bearberry, and clover. They relieve inflammation, suppress pathogenic microflora, and have a wound-healing effect. To wash the surface of the lesions, a decoction of bear's ear leaves is used, and an infusion of cucumber and laurel leaves is added to the bathing water. You can reduce the burning sensation by moistening the wounds with onion juice or applying a piece of ice to them.
Fireweed oil, obtained from primrose flowers, effectively eliminates the symptoms of eczema. Lubricating the affected areas with this remedy restores the structure of the skin and relieves itching. The course of treatment is 3–4 months. You can also add a couple of spoons of oatmeal to your bath. Water procedures should not be taken for long to avoid softening of the skin. Then it is advisable to lubricate the areas of inflammation with a cream containing calendula extract or vitamin E.
Alternative therapy methods
For atopic eczema, homeopathy, acupuncture, oligotherapy, heliotherapy, reflexology, and yoga help improve the condition of the body. The selection of homeopathic remedies and their dosages should be carried out by a specialist. Acupuncture restores proper circulation of vital energy in the body affected by the disease, improves the condition of the immune system, and relieves allergic manifestations.
Heliotherapy uses solar treatments to treat various diseases. Scientists have noticed a beneficial effect of sun radiation on lesions, but it should be moderate; the best time for walking in the fresh air or visiting the beach is before 11.00 and after 15.00. The therapeutic effect of oligotherapy is based on saturating the body with microelements, the deficiency of which is usually found in atopic dermatitis and eczema. These substances are very important for maintaining healthy skin.
Reflexology uses massaging, pressure and rubbing of the reflex zones located on the hands and feet. The procedure has a positive effect on the nerve endings located in these parts of the body, triggering the body’s self-healing processes.
The surface of the palms and feet is interconnected with other organs and systems, so treatment sessions help normalize blood circulation, improve the immune system, improve mood and well-being. Yoga helps the body relax as much as possible and relieve the negative effects of stress. Controlling your breathing during exercise allows you to saturate all the cells of the body with oxygen and improve the functioning of vital organs.
The concepts of “dermatitis” and “eczema” in the history of dermatovenerology have undergone dynamic development due to the expansion of our knowledge in related branches of medicine (for example, allergology). However, to date there is no unambiguous understanding of the differences between these diseases, since there is no clear definition and classification of them. Despite the rapid development of allergology, outdated concepts continue to dominate in dermatovenerology.
Some authors identify the content of the terms “eczema”, “atopic dermatitis”, “allergic eczema”, “disseminated neurodermatitis”, “prurigo” and the terms “lichenification”, “eczematoid dermatitis”, “food” and “infantile eczema”, etc. .
Due to the transition of healthcare to insurance medicine, terminological confusion does not allow assessing the quality of medical care and, therefore, needs serious correction.
A.I. Pospelov gives the following definition of eczema: “Eczema is an inflammatory skin disease, in most cases not contagious and usually occurring chronically, less often acutely.” In a later work, A.I. Pospelov, calling eczema “weeping lichen,” gives the following definition: “Eczema currently means superficial inflammation of the skin, accompanied by redness, swelling, fever, the appearance of scattered nodules and blisters, weeping or peeling , a feeling of tension, burning and significant itching." The author further divides eczema into acute and chronic. Describing the course of eczema, he writes: “If you cause artificial inflammation on a person’s skin by lubricating the skin, for example, with turpentine or another substance, subjecting it to friction or elevated temperature, then a few hours after this, at the site of irritation, the skin will turn red and swell (edema) , its local temperature will rise and the affected area will “burn” or itch - this will be eczema erythematozum.” In our opinion, the described clinical picture corresponds to simple contact dermatitis, but not eczema, which indicates the existence of discrepancies even among such a famous dermatologist as A.I. Pospelov.
According to the definition of V. Duperrat (1959): “Eczema is the most common skin reaction to extremely small external or internal influences (which are not all known yet), a reaction that during its development represents, first of all, a complex of dermal-epidermal lesions, among which spongiosis with vesiculation predominates.”
Even in modern clinical recommendations for dermatovenereology, the division of eczema into acute and chronic dominates: “Eczema (from the Greek Ekzeo - I’m boiling) is an acute, less often chronic, recurrent allergic disease, characterized by the appearance of a polymorphic rash, severe itching and an acute inflammatory reaction caused by serous inflammation of the skin.” .
Dr. Max Joseph, citing the experiments of Hebra, who, by rubbing croton oil into a healthy area of the skin, received “... a number of clinical phenomena that in many respects were similar to the phenomena observed in acute eczema. This proved that irritation acting on the skin can cause various clinical forms of the disease." He also divides eczema into acute and chronic and gives six stages of development of acute eczema: erythematous, papular, vesicular, oozing, impetiginous and squamous." Thus, the polymorphism of rashes is considered as pathognomonic signs of acute eczema, while chronic eczema is recognized not by the duration of the process, but by the changes that remain as a result of the development of the disease: “In chronic eczema, persistent changes in the skin, dense impregnation, cracks and etc.” .
G.I. Meshchersky attributed eczema to a skin syndrome, “... which at the height of development is characterized by edematous erythema with tiny, poppy seed-like, transparent blisters filled with a pale yellow sticky liquid, superficial, i.e. located directly under the stratum corneum."
A.I. Kartamyshev understood eczema as: “Itchy, often located in symmetrical areas, superficial inflammation of the skin, which is characterized by the appearance of nodules and blisters, often turning into erosions or crusts and healing with the formation of scales without leaving permanent changes in the skin. ...Eczema is characterized by polymorphism of the primary and secondary elements of the rash, a tendency to relapse, and a feeling of itching that always accompanies the disease.”
M.M. Zheltakov defined eczema as an allergic disease, which is characterized by a rash of blisters, weeping and a chronic relapsing course. Speaking about allergic dermatitis, M.M. Zheltakov cited the name “Eczematous dermatitis” as a synonym, thereby emphasizing the similarity of clinical manifestations.
O.L. Ivanov et al. distinguish “allergic dermatitis” and “toxidermia”, apparently implying “contact allergic dermatitis” by allergic dermatitis. They note that the clinical picture of allergic dermatitis is similar to the acute stage of eczema. It is also indicated here that the differential diagnosis of allergic dermatitis is carried out with eczema, which is characterized by polyvalent (rather than monovalent) sensitization and a chronic relapsing course, with toxicoderma, in which the allergen is introduced into the body. Describing the treatment of toxicoderma, the authors write: “With fixed toxicoderma, they are limited to the use of local anti-inflammatory and, if necessary, antiseptic agents...”. It is not clear what kind of fixed toxicoderma we are talking about; apparently, contact allergic dermatitis is again implied. At the same time, citing the formulation of eczema, the authors indicate: “Eczema is a common chronic recurrent skin disease of allergic origin, characterized by polyvalent sensitization and a polymorphic itchy rash (vesicles, erythema, papules).”
B.I. Karuna believes that eczema occurs acutely, subacutely and chronically, and divides eczema into true, or idiopathic, microbial, occupational, seborrheic, and childhood.
N.A. Torsuev et al. write: “Dermatitis is a common inflammatory reaction of normally responsive skin to external and internal harm. Eczema is a dermatitis in a predisposed subject; it is a special form of intolerance reaction. Thus, as H. Fuchs and L. Kumer correctly note, every eczema is dermatitis, but dermatitis is by no means eczema.” Further, the authors propose: “... the concept of allergic or eczematized dermatitis should be removed as completely unfounded and unnecessary and a strict distinction between the concepts of “dermatitis” and “eczema” should be adhered to (unfortunately, it is not specified which dermatitis we are talking about).
Literary references can be continued, but a brief excursion into the history of the issue allows us to conclude that scientists are divided into two groups: those who separate the concepts of allergic dermatitis and eczema and those who mix them up.
If we analyze the chronology of changes in ideas about dermatitis and eczema, the following pattern can be traced. At a time when there was no knowledge about allergic processes, the concept of “allergic dermatitis” naturally did not exist. With the development of allergology, a division of dermatitis into “simple contact” and “allergic” appeared. Despite the accumulated knowledge of the pathogenesis of allergic dermatoses and the inclusion of eczema in the group of these diseases, a clear separation of eczema from allergic dermatitis has not occurred.
In the protocols for the management of patients, eczema is interpreted as “a chronic recurrent acute inflammatory polyetiological disease with pronounced polymorphism of the elements of the rash,” and toxicdermia is “an acute inflammatory lesion of the skin and often mucous membranes, resulting from exposure to toxic, allergic, toxic-allergic agents introduced into the body ( inhalation, oral administration, parenteral administration). The clinical picture is distinguished by the polymorphism of the rashes (spots, papules, urticaria, vesicles, etc.).” As can be seen from the above definitions, the difference between the two diseases is only in the duration of their course, but there is no semantic meaning in the phrase “chronic recurrent acute inflammatory disease.” You can understand that eczema throughout the entire illness is an acute inflammatory dermatosis, but this is far from the case.
The definition of toxicerma also leaves much to be desired. In the standards for the provision of specialized medical care in the section: “Diseases of the skin and subcutaneous tissue” for nosologies, including allergic dermatoses, atopic dermatitis is presented; dermatitis, unspecified (true eczema); dermatitis caused by substances taken orally (toxidermia); hives. The standards do not provide a definition of nosological units, while true eczema is equated to “unspecified dermatitis.”
It seems to us necessary to improve the classification of dermatitis and eczema, because (as already indicated) insurance medicine is unthinkable without a basic focus on quality standards of medical care.
Taking into account the above literature review and modern ideas about the etiopathogenesis of allergic dermatoses, two solutions to this problem are possible. First, in the classification of dermatitis it is necessary to distinguish: simple (artificial) contact dermatitis, caused by unconditioned (obligate) irritants, and allergic dermatitis, caused by conditioned (facultative) irritants (allergens). In turn, allergic dermatitis is divided into contact allergic dermatitis, which occurs from direct contact of the skin with the allergen, and toxicoderma, which occurs when the allergen penetrates the bloodstream (through the gastrointestinal tract, respiratory tract and parenterally). With this division of dermatitis, eczema is presented as a chronic, recurrent allergic disease, arising as a result of polyvalent sensitization of the body and manifested by true polymorphic rashes (spots, papules, vesicles, pustules) with a tendency to vesiculation and weeping, with the subsequent development of false polymorphism (evolution of primary elements with the appearance crusts, scales, pigmentation, lichenification).
With this approach, eczema can only be considered a disease that has a chronic course with frequent relapses and short remissions. When a characteristic pathological process occurs for the first time, it is impossible to predict how the disease will develop - whether it will become protracted, recurrent, or will never happen again. Consequently, the first episode of the disease and extremely rare relapses over a long period of time should be considered as manifestations of allergic dermatitis. A prolonged course of newly diagnosed dermatitis cannot be diagnosed as eczema. There are cases when allergic dermatitis lasts 3-4 months and never recurs.
Secondly, if allergic dermatitis is excluded from the classification of dermatitis, leaving only simple contact dermatitis, then the manifestations of allergic dermatitis (contact and toxicoderma) should be regarded as acute eczema. In this case, eczema should be interpreted as an allergic disease with mono- or polyvalent sensitization, manifested by true polymorphic rashes (spots, papules, vesicles, pustules) with a tendency to vesiculation and weeping, with the subsequent development of false polymorphism (evolution of primary elements with the appearance of crusts, scales , pigmentation, lichenification), characterized by acute and chronic course.
In the case of monovalent sensitization, eczema will be regarded as acute, since it (according to modern concepts) is nothing more than allergic dermatitis, which has a similar clinical picture. When polyvalent sensitization occurs, when any of the allergens (or the combined effects of allergens) can cause or aggravate the allergic process, it becomes protracted, recurrent in nature, and in this case we will talk about chronic eczema.
We deliberately included in the wording such features of eczema as vesiculation and weeping. This must be taken into account to differentiate eczema from neurodermatitis, because with eczema at the time of examination there may not be vesiculation and weeping, although anamnesis most often reveals this.
In conclusion, it should be noted once again that, despite the centuries-old history of dermatology, a clear understanding of dermatitis and eczema has not been formed and, given the relevance of this problem, we invite dermatologists to discuss it in order to develop a consensus on standardizing the concepts and criteria for assessing the quality of medical care for allergic dermatoses.
Bibliography
- Torsuev N.A. , Veynerov I.B. , Buharovich M.N., Goldstein L.M. Allergic itchy dermatoses. Kyiv, “Health”, 1973.
- Pospelov A.I. A short textbook of skin diseases. M, 1896: 130.
- Pospelov A.I. A guide to the study of skin diseases for doctors and students. M., 1905: 457.
- Duperrat B. Precis de Dermatologie. Paris: Masson, 1959: 1106
- Clinical recommendations. Dermatovenerology. edited by A.A. Kubanova. M.: DEX-Press, 2007: 205.
- Skin diseases. A guide for doctors and students, edited by T.P. Pavlov. St. Petersburg: publication of the journal “Practical Medicine”, 1900: 36-37.
- Meshchersky G.I. Textbook on skin and venereal diseases. Moscow-Leningrad, 1936: 135.
- Kartamyshev A.I. Skin and venereal diseases. Kyiv: State. Honey. from the Ukrainian SSR, 1952: 118.
- Zheltakov M.M. Skin and venereal diseases. M.: Medicine, 1964: 157.
- 10. Ivanov O.L. , Molochkov V.A. , Butov Yu.S. , Kryazheva S.S. and others (edited by O.L. Ivanov). Skin and venereal diseases. M.: “Shiko”, 2002: 170, 177
- 11. Karuna B.I. Eczema Kyiv: “Health”, 1989: 176
- 12. Allergic itchy dermatoses. N.A. Torsuev, I.B. Veynerov, M.N. Buharovich, L.M. Goldstein - Kyiv: “Health”, 1973: 23-24.
- 13. Methodological materials on the diagnosis and treatment of the most common sexually transmitted infections (STIs) and skin diseases. Patient management protocols. – M., 2001.
- 14. Collection of standards for specialized medical care. – M., 2008, – T. II, – P. 997-1039.