More than 60% of people on the planet are infected with the human papillomavirus. HPV 56 belongs to this family. The group of viruses is similar in symptoms and routes of infection, but differs only in oncogenic risk and cross-infection. The diagnosis of HPV of this type is scary for most people, and this is justified, since it provokes the development of neoplasia (cancer) in the cells of the reproductive organs, shortening life and its quality.
HPV type 56 is most often transmitted sexually and poses a significant threat to the human reproductive system.
Features of type 56 virus
Human papillomavirus (Human papillomavirus) is a heterogeneous group of viruses that affects the skin and mucous membranes, for example, the cervix, anal canal, and oral cavity. More than 600 types (strains) are known. HPV is the most common infection that is transmitted during sexual contact. It is so disseminated that all sexually active people can be carriers of it at any time in life. All strains can be divided into 3 groups:
- HPV with low oncogenic risk (HPV 3, 6, 11, 13, 32, 34, 40, 41, 42, 43, 44, 51, 61, 72, 73);
- HPV with average oncogenic risk (HPV 30, 35, 45, 52, 53, 56, 58);
- HPV with high oncogenic risk (HPV 16, 18, 31, 33, 39, 50, 59, 64, 68, 70);
Human papillomavirus: treatment and prevention
The most relevant method for preventing HPV today is vaccination. After three-time immunization with one of the three existing vaccines, antibodies (immune protection) to HPV16, HPV18, HPV6, HPV11 are detected in 99% of vaccinated people.
Preventive measures also include:
- Maintaining personal hygiene
- monogamous sexual relationships;
- using a condom for oral, vaginal, and anal intercourse.
HPV treatment is carried out strictly according to the doctor’s recommendation.
Therapy may include:
- immunocorrection
- cytotoxic drugs
- antiviral drugs
- special creams, gels;
- laser therapy;
- cryodestruction;
- electrocoagulation.
A gynecologist can determine the scope and tactics of treatment after examination and studying the results of the study. Even if there are no clinical signs of HPV, but only a positive laboratory test for oncogenic strains of HPV, it is necessary to carry out preventive treatment and regular examination by a doctor.
For more detailed consultation, please contact the specialists of the President-Med medical centers
ul
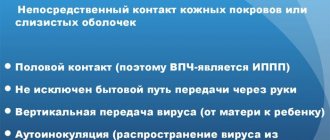
Transmission routes and risk factors
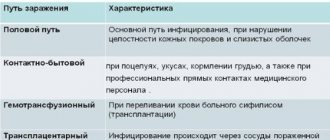
Human papillomavirus genotype 56 is a dangerous type of infection that, penetrating the body, can provoke skin rashes, as well as genital lesions. HPV penetrates from an infected person to a healthy person during unprotected sexual intercourse, through the oral cavity and open wounds on the skin.
Papilloma is a papillary growth on the skin, which, under the influence of negative factors of the external and internal environment, can degenerate into malignant neoplasms. The causative agent is the human papillomavirus. Some types affect only the skin, but most cause diseases of the genitals in men and women.
The entrance gates of papilloma are microtraumas and the mucous membrane. Frequent localizations for type 56 virus infections are the mucous membrane of the genital organs, uterus, perinatal area, vagina in women, urinary tract, urethra, glans penis in men.
The external part of the urethra in men is most often affected and accounts for 25% of all cases. Risk factors for activation of oncogenic type 56 infection are:
- decreased immune defense, metabolic disorders;
- genetic predisposition to cancer;
- exacerbation of chronic pathologies of the reproductive system and the whole body;
- thermal and chemical local irritants;
- unprotected sexual intercourse;
- visiting places with high humidity: baths, swimming pools, beaches.
Advice! When visiting public beaches and bathhouses, it is recommended to always wear slippers in order to protect yourself from accidental exposure to type 56 infection.
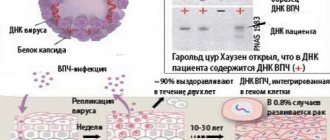
Penetrating into the human body, papilloma virus 56 or another type first passes along the nerve to the brain, where it awaits activation during a stress factor. When immune defenses decline, it travels down the nerve back to the site where direct contact with the mucous membrane or skin occurred.
First, the deep epithelial layer in women or men is affected, then the virus, after waiting a little, penetrates the surface and begins its active reproduction. The proliferation of human papilloma leads to damage to neighboring cells and control of their growth is lost. A feature of the type 56 virus is its rapid penetration into the DNA of women or men, and then its transformation begins.
ul
Symptoms of infection
Clinical manifestations of the human papillomavirus begin with the formation of a papillary formation, but they may not be visually detected if the internal genital organs in women or the urethra in men are affected. It is important that one person may simultaneously have several oncogenic viruses with a high and low risk of degeneration into a malignant process.
How to determine the presence of papilloma?
- Women develop genital warts on the genitals, some of which can only be observed during a gynecological examination, since they are located in the vagina
- The appearance of condyloma occurs in the third month of infection, thus it is possible to trace the pattern of the appearance of papilloma and the last unprotected sexual intercourse.
- Visually, condylomas have uneven edges and stand on a “pedicle”.
Advice! The most typical and dangerous manifestation of HPV is cervical neoplasia; it is diagnosed during an examination by a gynecologist, after which surgical treatment can be prescribed.
Diagnosis of the disease
To detect HPV in the body, you need to undergo a special test that can determine not only the virus, but also its type. Diagnostic signs of the disease:
- antibodies to infection are detected in the patient’s blood;
- externally visible warts, genital warts;
- cervical dysplasia diagnosed by cytological examination.
A special PCR analysis is used for diagnosis, but even the high sensitivity of such a test does not guarantee the detection of HPV due to its specific features:
- The asymptomatic course can last about five years.
- The infection is in a latent state, not spreading to the skin and mucous membrane.
- The extensive affected area does not allow specialists to select the area of skin for analysis where the largest amount of virus is concentrated.
Advice! Studies were conducted on women with the HPV virus, tests were prescribed every week for several months, but not every diagnosis had a positive result. In this regard, it is recommended to complete the study several times to ensure the reliability of the results.
ul
How is HPV treated?
Standard treatment for type 56 virus depends on the underlying disease and clinical manifestations. Treatment of a carrier of the virus is still impossible, since it is impossible to completely eliminate HPV from the brain and circulatory system without harm to health.
Such patients regularly visit a doctor to assess their general condition and monitor viral activity. When immunity decreases, the infection begins to manifest itself, then antiviral and restorative treatment is carried out.
When external signs of a disease caused by type 56 infection appear, constant monitoring of the patient and treatment of the resulting pathological processes are necessary.
The viral infection is eliminated by a radical method, surgical treatment of the mucous membranes and skin helps prevent the transition of the formation into malignant tissue growth. Modern methods of radical therapy include laser treatment, diathermocoagulation, and radio wave ablation.
Chemical treatment with local drugs is also used. For genital lesions in men, conservative treatment is first indicated, by freezing or chemical exposure.
Prevention methods
Primary prevention of HPV is vaccination. Today, two vaccine options are offered: Cervarix, Gardasil:
- Vaccination with Gardasil is effective for the prevention of high oncogenic risk infections: types 31, 56, 16. The effectiveness of such vaccination is more than 91%; it is effective for the prevention of erosive processes of the cervix in women, lesions of the anal canal and external genital organs.
- Vaccination with Cervarix is carried out to prevent damage to the virus types 18 and 16, which can cause uterine dysplasia in women and then cancer.
Secondary prevention after penetration of genotype 56 virus into the body can be distinguished:
- maintaining personal hygiene;
- protected sexual intercourse;
- use of individual hygiene items: towel, soap;
- taking vitamin complexes to increase general immunity.
Preventing the activation of the human papillomavirus is very important in case of a genetic predisposition to cancer, therefore women and men should visit a specialized doctor every six months, which will allow timely identification and maintenance treatment.
ul
Transmission routes and risk factors
HPV is spread in 33% of cases through sexual transmission - the main route. Since during sexual intercourse the integrity of the epithelium is disrupted, which allows human papillomavirus type 56 to penetrate and cause infection. There are also other ways of transmitting the virus:
- baby in labor;
- through touch - by contact (in public places through minor wounds, scratches on the skin).
The human papillomavirus is not transmitted aerogenously, that is, through the air and touching objects, for example, a door handle, a handshake.
People with weakened immune systems, uncontrolled sex life and poor hygiene are at risk of contracting HPV type 56.
Human papillomavirus exists in the body in a latent state. In 90% of cases, within 6-12 months the body copes with the infection on its own - self-healing. The onset of symptoms and transition to a chronic disease, with frequent exacerbations, occurs if the following risk factors are present:
- reduced immunity or immunosuppression;
- overwork, chronic stress;
- a large number of sexual partners;
- early onset of sexual activity;
- HIV infection;
- presence of other STDs;
- nutritional deficiency;
- drug use, smoking, psychoactive substances;
- genetic predisposition;
- pregnancy.
Why is DNA type 56 dangerous?
Oncogenic papillomas often lead to infection of the genitals, which become vulnerable to many diseases. The virus takes part in the formation of cervical cancer in women and gives impetus to the development of cervical neoplasia. HPV DNA of types 56 must be destroyed at an early stage of the disease.
The DNA of the virus genotype penetrates human DNA cells and causes them to change. This is a dangerous process that:
- expands the lesions;
- reduces immunity;
- increases the risk of rapid development of severe infections.
Once hpv 56 enters the body, it accompanies the development of malignant neoplasms. To prevent this from happening, you need to take preventive measures in advance. Many countries around the world now offer vaccinations to prevent HPV infection. The vaccine is 91% effective and covers 4 types of such viruses. The procedure is suitable for people of any age, but it is better to vaccinate before the age of twenty-one. Vaccinations are safe, are not accompanied by any negative consequences and can only cause mild swelling, a slight rise in temperature, and mild tingling in the muscles.
Maintaining good hygiene will help you avoid illness. You cannot use other people’s towels, soap, or allow sexual intercourse with different partners. In a bathhouse, sauna, shared shower, in a swimming pool, on a public beach, you must wear rubber slippers. Vitamin complexes that boost immunity and improve health help protect against HPV 56. People with a genetic predisposition should visit a doctor once every 6 months and undergo appropriate examination.
Risks for men and women
Type 56 belongs to the oncogenic risk group, affecting the human reproductive system, causing genital infection in women and men. Both sexes, regardless of sexual orientation, will be infected with at least one type of HPV virus during their lifetime. For men, HPV is not dangerous because it is not associated with health risks. Genital warts occur in men infected with the virus, but are extremely rare. In women, on the contrary, the frequency of occurrence is quite high - 80%. Also, type 56 virus in women leads to erosion and cervical dysplasia - pathological changes in the normal epithelium of the internal organ. The DNA of the virus, weakening the human immune system, activates the appearance of bacterial, fungal, and other viral infections.
Symptoms of human papillomavirus
External manifestations of HPV:
- Warts: squamous (juvenile), plantar, common (vulgar). Flat warts usually appear in children and adolescents. They are found both completely flat and with a slightly raised surface. Vulgar warts are quite rough; they most often appear on the fingers and elbows. Plantar warts are described as hard, granular growths on the feet.
- Genital warts are genital warts that resemble a small cockscomb or the head of a cauliflower. They can vary in size and color. In women, genital warts appear mainly in the area of the external genitalia, on the cervix, near the anus. In men - on the scrotum, penis, around the anus, in the groin.
ul
HPV symptoms
After an incubation period, which lasts on average from 15 days to several years, symptoms of infection appear in only 10% of cases. It is generally accepted that there are no symptoms of the disease. Despite the fact that the virus causes changes in skin cells and mucous membranes, they are insignificant and do not cause concern or complaints in the patient. Papillomavirus 56 causes noticeable changes in the presence of risk factors. Warts or genital warts, which can be found around the anus, on the penis, and scrotum in men. The same condylomas appear on the female genitals - on the labia majora and minora, on the clitoris, and also in the urethra. Their appearance may be accompanied by itching and burning.
HPV type 56 provokes the growth of intimate warts, and they are a source of physical discomfort.
Condylomas are formations that protrude above the surface of the skin or mucous membrane on a stalk. They have a variety of colors - from pale pink to dark brown. They tend to merge and grow rapidly. They are characterized by growth not only above the surface of the skin, but also grow inside, which makes it difficult to remove.
The US Center for Infectious Disease Control states that HPV infection causes cancer of the cervix and vagina in women and penile cancer in men. HPV type 56 also causes cancer of the anal canal and oropharynx. But dysplasia, and then cervical cancer, is still of particular importance.
What are the dangers during pregnancy?
During pregnancy, a woman's immunity decreases due to hormonal imbalance, which leads to the expectant mother's sensitivity to infections, especially HPV. A history of HPV does not affect a woman's fertility, but tell your doctor if you have an obvious infection during pregnancy. Pathological growths on the genitals cause certain problems during pregnancy.
- Due to an imbalance of hormones, warts in the urethra can increase in size and grow, making it difficult to urinate.
- In the vagina, warts reduce the elasticity of its wall and can also cause blockage of the lumen during childbirth. If the condylomas are not removed, a caesarean section will be required to deliver the baby. Infants whose mothers have the papilloma virus may develop warts in the throats called laryngeal papillomatosis. What causes wheezing and asphyxia (difficulty breathing) in children.
What are the consequences of HPV during pregnancy?
To date, there is no reliable evidence of a pronounced negative impact of infection on the course of pregnancy.
Pregnancy pathologies such as miscarriage, premature birth, etc., which are characteristic of other sexually transmitted infections, have not found unconditional confirmation of the connection with HPV.
However, if a woman’s primary infection occurs during pregnancy, there is a risk of developing various complications.
Anogenital warts in the mother caused by HPV types 6 and 11, localized in the area of the labia minora and the vestibule of the vagina, have some consequences for the fetus during pregnancy.
Such genital warts carry a small risk of infection of the fetus during childbirth, leading to the development of respiratory papillomatosis in the latter.
Respiratory, or otherwise laryngeal, papillomatosis (also called laryngeal papillomatosis) most often develops in children 2 to 3 years old.
As a result of infection from a sick mother during the latter’s pregnancy or immediately at birth.
The route of transmission during pregnancy through the placenta, during childbirth or immediately after it is not yet entirely clear.
The main symptoms of the disease are hoarseness, up to the complete disappearance of the voice, and difficulty swallowing.
As the disease progresses, shortness of breath and cough appear.
In severe situations, blockage of the upper respiratory tract and asphyxia are possible, especially in the case of formations with a long thin stalk.
During examination using a laryngoscope (sometimes a bronchoscope is also used), typical growths - condylomas - are found on the laryngeal mucosa.
This pathology has a rather aggressive course: after removal of the formations, relapses often occur, requiring repeated surgical interventions.
If pregnancy occurs due to infection with highly oncogenic papillomaviruses (especially HPV 16, 18), the woman must inform her obstetrician-gynecologist about the presence of infection.
The fact is that changes in a pregnant woman’s body can provoke more intense cell transformation.
Actually, such viruses do not affect the course of pregnancy itself or the child, but they pose a certain threat to the woman’s health.
In a situation where no infection was detected in the past, a cytological Papanicolaou smear (Pap test) is taken, among others, when registering.
If the analysis shows abnormalities, the doctor prescribes additional tests (for example, colposcopy).
Also, situations when pregnancy occurs in women with erosion require special attention.
PCR diagnostics are required to exclude infection with high-oncogenic risk HPV.
As a rule, in the routine practice of an obstetrician-gynecologist, such a combination as HPV and pregnancy is not specifically examined.
Tests for the virus are recommended only if pathological abnormalities are detected.
At the same time, there are research studies demonstrating the effect of the virus on pregnancy.
Thus, it has been shown that infection of women with HPV slightly reduces the likelihood of embryo implantation, and in men it reduces sperm motility.
And since in a married couple, as a rule, both partners are infected, the onset of pregnancy is associated with some difficulties.
As a result, when planning a pregnancy against the background of an infection caused by HPV, planning an IVF procedure, this factor should also be taken into account.
Diagnostics
Diagnosis of HPV type 56 involves laboratory testing of biomaterial.
Diagnosis of human papillomavirus begins with an external examination of the skin and mucous membranes to identify atypical neoplasms. During mandatory preventive examinations for women, a gynecologist undergoes a Papanicolaou smear during a colposcopic examination. In fact, 25% of atypical smears will detect the virus. Testing for human papillomavirus is a screening test for women aged 25 to 65 years. There is no reliable test for detecting HPV infection in men. But a group of people who are at high risk of developing anal cancer may be offered an anal smear test.
The PCR (polymerase chain reaction) method is not ineffective. It determines the presence of viral DNA in epithelial cells with 95% accuracy, thus it is possible to differentiate different types of HPV. HPV 51 is also associated with HPV type 56. There is another screening test - the Digene test, which is used to determine a high concentration of papillomavirus.
Why is human papillomavirus dangerous for women?
Ordinary warts look unsightly and can become inflamed when scratched, so they are removed (laser, cryodestruction, electrocoagulation).
High-risk oncogenic HPVs are the cause of cervical cancer. Numerous studies have been conducted and it has been proven that without HPV, cervical cancer does not exist, with the exception of metastases from other organs. Vaccines have been developed and are used to protect against the most oncogenic strains of HPV. Seventy percent of clinical HPV infections in healthy adults regress to a subclinical (asymptomatic) form within one year, and 90% within two years.
However, the virus persists in the body, and infected women are at high risk of precancerous lesions on the vulva and cervix, which can develop into invasive cancer. Progression from asymptomatic to clinical forms takes years, so women should be screened regularly to identify and treat precancerous lesions.
Recommended examinations for early detection of HPV and cancer:
- Examination and consultation with a gynecologist
- Colposcopy
- Human papillomavirus PCR smear
- Liquid oncocytology
- Pelvic ultrasound
ul
Treatment of infection
After confirmation of HPV type 56 by diagnostic procedures, therapy should begin, which is aimed only at the consequences of the virus. After all, there is no specific treatment that would eliminate the virus from the body. Treatment is divided into two groups:
- surgical;
- medicinal.
Surgical tactics are aimed at removing atypical tissues: the formation of condylomas, warts and other neoplasms in tissues and mucous membranes. If condylomas or other neoplasms are found, then well-known removal techniques are used:
- cryosurgery;
- laser therapy;
- chemodestruction with trichloroacetic acid;
- radio wave surgery;
- electrocoagulation;
- radical methods - amputation of the cervix.
Treatment of HPV type 56 is carried out with medication and surgery.
Using such surgical methods, the focus of the affected tissue is removed. Efficiency ranges from 65 to 45%. But, due to the fact that complete removal of the affected tissue cannot be controlled, the relapse rate is about 50% of cases. If after 3 treatments there is no noticeable improvement or if after 6 treatments the warts have not completely disappeared, another type of therapy is used.
It is better to treat HPV using a combination of medications and surgical techniques, then the effectiveness is up to 90%. Drug treatment includes the use of antiviral drugs (Interferon), and in the subsequent period, immunomodulators that will increase the resistance of the immune system to infections (Likopid, Immunomax and others).
Prevention methods
The main method of preventing STDs and the papillomavirus group is the use of protection during sexual intercourse. Another method of creating immunity against HPV is vaccination. Doctors recommend that children at 11 or 12 years old get vaccinated. It is possible for men under 21 to be vaccinated and women under 26 if they did not get vaccinated when they were younger. HPV vaccines are isolated from proteins called virus-like particles (VLPs) produced using recombinant technologies. They do not contain any live biological products or viral DNA, so they are safe and create a robust immune response. The HPV vaccine also has side effects, but they are quite minor. In addition, its effectiveness is much higher than the side effects. Side effects:
- pain;
- swelling at the injection site;
- redness;
- increased body temperature;
- headache;
- increased feeling of fatigue;
- tingling sensation in the muscles;
Vaccination is recommended for gay people and people with weakened immune systems (HIV-infected people, patients taking glucocorticosteroids). If infection and the manifestation of the above symptoms are detected, there are risk factors, then it is necessary to contact such specialists as a gynecologist, urologist, or dermatovenerologist. The effectiveness of immunotherapy and their recovery depend on the consciousness of patients.