The article selects effective and inexpensive ointments that can quickly get rid of streptoderma. You will learn what ointment to use and how to prepare it at home if the disease begins to spread over the skin. As a result, after reading the article you will be able to quickly cope with the disease.
Before starting treatment, you need to identify the disease. Which group does it belong to and how is it treated? Do not start treatment without making a correct diagnosis and prescribing an effective drug that is suitable for this disease.
Etiology and pathogenesis of streptoderma
Streptoderma is an infectious skin disease that is part of the group of pyodermatitis. The pathology occupies a leading place among all skin diseases in children, and is more common in women, people with thin skin and immunodeficiencies.
The main causative agent of the disease is β-hemolytic streptococcus of group A. It is part of the normal microflora of the skin and exhibits its pathogenic properties when the general resistance of the body decreases and autoinfection (self-infection).
Streptoderma can also be caused by streptococci common in the environment (exogenous infection). They, unlike other bacteria that cause infectious diseases, are unstable in the external environment.
Streptococci die when heated to more than 56° for 30 minutes, and when boiled - instantly. Bacteria can withstand drying well, but at the same time lose their pathogenic properties and quickly die under the influence of antiseptics and disinfectants. Group A streptococci are sensitive to penicillin antibacterial drugs and do not acquire resistance to them.
Streptococci mainly develop in the upper layer of the skin. The cytopathogenic effect of streptococci is characterized by the release of toxins: streptolysin, erythrogenin, leukocidin. Exotoxins destroy white blood cells and other blood cells and cause dilation of small blood vessels.
Damage to skin tissue by streptococci leads to nutritional and metabolic disorders. Inflammatory mediators are released, increasing vascular permeability and local microcirculation. This leads to the development of hyperemia (tissue fullness) and the leakage of the protein-containing part of the blood through the vascular wall (exudation) into the tissue.
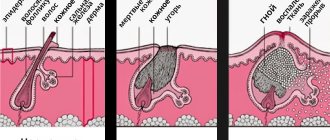
A reddened area with a bubble filled with exudate (phlytena) forms on the surface of the skin. During their life, streptococci secrete enzymes that promote the spread and penetration of infection into deeper tissues.
Classification
Streptoderma can be primary - damage to healthy skin, and secondary, occurring against the background of somatic pathologies. The modern classification of streptoderma allows you to track morbidity statistics and prescribe the correct treatment.
Division of pathology according to the form of clinical course:
- Acute streptoderma. Manifests itself with severe symptoms specific to streptococcal infection. With adequate and timely treatment, it almost always ends in recovery.
- Chronic streptoderma. The diagnosis is made after 2 months of constant progression of the pathology. Characterized by periods of relapses and remissions, erasure of the main signs.
According to the form of skin lesion:
- streptococcal impetigo;
- bullous impetigo;
- lichen;
- slit-like impetigo.
Skin lesions with streptoderma can be superficial (impetigo) and deep (ecthyma). There are localized (damage to certain areas) and diffuse (spread over large areas) forms of pathology. Often streptococcal infection is combined with staphylococcal infection.
Etiological factors
The development of ecthyma is facilitated by infection with pathogenic bacteria or insects. Primary infections are more often diagnosed in children, secondary infections occur with equal frequency in people of different ages who have a history of chronic diseases that can cause depletion of the body. These include tuberculosis, diabetes, HIV, and oncology.
Large, poorly healing ulcers may appear in those who develop local problems with blood flow and lymphatic circulation (thrombophlebitis). Another etiological factor is progressive itchy dermatoses. Their course is accompanied by severe itching, the patient tries to comb the affected areas of the body, injuries to the inflamed skin contribute to the addition of a secondary bacterial infection. Any wounds on the skin are an open gate for the penetration of staphylococci and streptococci. Infection with pathogenic microorganisms gives impetus to the development of all purulent-necrotic reactions.
The cause of the disease can be an insect bite or tick infection. Different pathogens provoke the development of different forms of infection.
Causes of spots on the face
A sick person with any form of streptococcal infection becomes a distributor of bacteria into the environment. It is possible to isolate the pathogen from the bacteria carrier. Streptococci enter the body of a healthy person through airborne droplets, household contact, or food routes.
Human skin and mucous membranes have local protective functions; in addition, healthy immunity promptly suppresses the development of all pathogens. Therefore, for the replication of streptococci and the onset of pathology, certain conditions are required.
Factors:
- skin damage (burn, scratch, bite, scratching);
- hormonal disorders (hypo-hyperfunction of the thyroid gland);
- changes in composition and increased production of sebum;
- disruption of the lipid layer of the skin (change in pH level from 6 to 7.5);
- immunodeficiencies, immunosuppression;
- chronic inflammatory pathologies (secondary infection);
- poor hygiene (neglect or infatuation with antibacterial detergents).
These factors can be caused by poor nutrition, hypovitaminosis, prolonged stress, chronic diseases and syndromes, poor environmental conditions and contact with chemicals.
The irrational use of antibiotics always causes the suppression of “beneficial” microflora, which often gives rise to the manifestation of the pathogenic properties of streptococci.
How to treat with folk remedies
To speed up recovery, auxiliary therapy with folk remedies is allowed in case of illness.
Recommendations for treating streptoderma in adults at home are as follows:
- dressings are used dipped in herbal decoctions that have drying properties and are not allergens: chamomile and oak bark;
- since during illness you cannot take a shower or bath, it is recommended to wipe healthy skin with napkins soaked in chamomile decoction;
- overheating of the skin and increased sweating should be avoided;
- following a diet that excludes sweet, fatty, and spicy foods from the diet;
- clothing should be made from breathable, natural materials.
Any treatment, even the most proven methods, must be accompanied by permission and supervision of a doctor. Otherwise, complications may arise that are difficult to correct.
Symptoms
After the pathogen enters the skin, the incubation period begins, which lasts 7-10 days. After this, hyperemia of the affected areas appears. Outwardly, this manifests itself as rounded pink spots with irregular outlines. After a few days, bubbles form on the surface of the elements, gradually filling with exudate.
With superficial skin lesions (impetigo), the blisters quickly open and form a crust. It gradually disappears, leaving behind hypopigmentation. As the skin renews itself, cosmetic defects completely disappear. These elements are called conflicts; their sizes can range from a few millimeters to 5 cm.
With deep damage (ecthyma), the germ layer of the skin is affected. This form of pathology is characterized by purulent-blood content of conflicts. After the crusts fall off, ulcerative elements form, leaving scars on the skin.
Skin damage is accompanied by:
- dryness and itching;
- swelling and pain;
- an increase in local temperature;
- peeling of necrotic tissues.
Mostly conflicts appear in the area of the nose, chin, cheeks and corners of the mouth.
In the atypical course of streptoderma (lichen), round pink elements, covered with transparent scales, form on the skin. Slit-like impetigo (jam) mainly affects the corners of the mouth. Characterized by the formation of cracks after opening conflicts. Since this area is constantly mobile and wetted by saliva, the pathology is difficult to treat. Cases of chronic disease are not uncommon.
Symptoms of intoxication may accompany the diffuse form of streptoderma. They are manifested by low-grade fever (up to 38.1°C), general malaise, nausea and headaches. In this case, an increase in regional lymph nodes is noted.
With any streptococcal infection, there is a risk of the pathogen spreading throughout the body, including to the internal organs. This leads to the formation of serious pathological processes, so you should not self-medicate. When you identify the first signs, you need to contact a dermatologist, undergo a full examination and receive adequate therapy.
What is ecthyma
Ecthyma is a pustule that occurs in the deep layer of the dermis. The location of the infiltrate is often the lower legs. The disease mainly affects people with weakened bodies. The pathology is caused by an infection that occurs as a result of serious illnesses: tuberculosis, syphilis, diabetes and other diseases. Ecthyma looks like an ulcer, from which pus can be released. After healing, a scar remains at the site of the pustule.
Ecthyma may occur near a cut or scrape
Types of pathology: vulgar, scabies, contagious, etc.
Ecthyma has the following classification:
- Vulgar (ordinary). Occurs due to bacteria entering the wound: streptococci or staphylococci. This can happen when you scratch an insect bite with dirty hands. It is a dense infiltrate that occurs as a result of infection entering the dermis.
- Contagious. With this form of the disease, pustules form on the mucous membrane of the mouth and lips. The causative agent is a viral infection.
- Syphilitic. The occurrence of ecthyma in this case is accompanied by manifestations of secondary syphilis. The pathology has a long and severe course.
- Scabies. A pustule forms on the genitals of individuals infected with a specific type of mite called scabies.
Diagnostics
Diagnosis of streptoderma includes a physical examination, medical history, and laboratory tests. During the examination, a dermatologist assesses the nature of the skin damage and the location of the elements. The patient’s presence of current chronic pathologies, the possibility of using antibacterial drugs, living conditions and household habits are clarified.
The main laboratory diagnostic method is macroscopic examination of scrapings from the surface of the skin and exudate. At the same time, a test is carried out to determine the sensitivity of bacteria to antibacterial drugs.
For specific indications you may need:
- general blood analysis;
- bacteriological blood test;
- blood test for Wasserman reaction;
- general urine analysis;
- stool analysis for worm eggs.
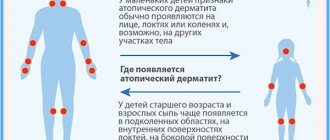
The pathology should be differentiated from atopic dermatitis, urticaria, pityriasis versicolor, other types of pyoderma, eczema and fungal infections. You may need to consult an immunologist and gastroenterologist.
Diagnostic tests
To determine the causative agent of this disease, a scraping is made from the ulcer or the contents of the pustule are taken for culture. When the infection is placed on soil favorable for its development, it begins to grow and multiply. The specialist very quickly identifies the cause and determines the sensitivity of the infectious agent to a certain type of antibiotic for further effective treatment. Microscopic examination allows differential diagnosis of this disease from impetigo, which has similar symptoms. However, with ecthyma the infiltrate is deeper.
When diagnosing, they often resort to microscopic examination of the crust, which helps to differentiate the disease from trophic ulcers and impetigo.
Streptoderma treatment complex
Complete recovery from streptoderma is possible only with complex treatment. It consists of the gradual use of etiotropic, pathogenetic and symptomatic agents. Treatment tactics, including a combination of certain drugs, should be selected by a dermatologist.
Skin treatment and antiseptics
Before starting therapy, it is necessary to treat the affected areas of the skin. To do this, the phlyctenes are opened at the base with sterile needles, cleaned of necrotic tissue and washed with a 3% solution of hydrogen peroxide.
The lesions are treated with antiseptic agents:
- brilliant green 1%;
- potassium permanganate 0.1%;
- fucorcin;
- chlorhexidine alcohol 0.5%;
- nitrofural 1%;
- methylene blue 1%;
- salicylic alcohol 2%.
The drug is applied locally using a cotton swab. After complete drying (20 minutes), apply ointments or compresses. Antiseptic treatment is carried out 2-4 times a day during the entire course of treatment.
Local preparations and ointments
In cases where the lesions are single, the general condition and immunity are normal, treatment is carried out with external drugs. These are medicines with antibacterial active substances.
Preparations:
- Gentamicin;
- Triderm;
- Baneocin;
- Retapamulin;
- Bactroban.
The ointments are applied 2-3 times a day in a thin layer to the treated affected areas. The duration of treatment depends on the shape and extent of the lesion.
After the formation of crusts, agents with keratolytic, anti-inflammatory and antiseptic properties are used. Preparations: salicylic, syntomycin, zinc ointments.
For slit-like impetigo, 2% silver nitrate is used. Cracks are lubricated 2-3 times a day.
Antihistamines
They are prescribed only for severe allergic reactions accompanied by unbearable itching. Third generation antihistamines are selected for treatment.
Medicines:
- Claritin;
- Levocabastine;
- Zyrtec;
- Telfast;
- Terfenadine.
Despite the fact that third-generation drugs have a small number of side effects, they must be selected by a doctor. This is in addition to possible cardiotoxic effects, the risk of which increases when combined with antibiotics.
Systemic antibiotic therapy
The decision on internal use of antibiotics is made in severe and diffuse forms of streptoderma, lack of therapeutic effect after a course of treatment with local drugs.
Indications for systemic treatment include the addition of regional complications: lymphadenitis, lymphangitis.
Penicillin drugs have good antistreptococcal activity. Therefore, they are the drugs of choice. If the patient has hypersensitivity to penicillins, drugs of other groups are prescribed.
Medicines:
- Clarithromycin;
- Erythromycin;
- Amoxicillin;
- Flemoxin solutab;
- Ciprofloxacin;
- Augmentin.
Medicines are used in the form of oral tablets, intramuscular or intravenous injections. The average course of treatment is from 5 to 14 days. Probiotics are prescribed during treatment.
Immunotherapy
Immunotherapy is prescribed for chronic streptoderma, which occurs with constant relapses at least once every 3 months. Indications for use are always proven cases of immunodeficiency.
Immunostimulating agents:
- thymus preparations: Taktivin, Timalin;
- γ-globulin preparations;
- synthetic chemicals: Isoprinosine, Levamisole, Diucifon;
- azoximer bromide: Polyoxidonium;
- stimulators of interferon production: meglumine acridone acetate, sodium oxodihydroacridinyl acetate.
For all chronic and sluggish forms of streptoderma, vitamin C and B vitamins are prescribed. To improve microcirculation, medications are used: Pentaxophylline, Xanthinol nicotinate.
Patients with any form of streptoderma are prescribed multivitamins for 1-2 months. Recommended complexes: Complivit, Vitrum, Multitabs.
Physiotherapy for streptoderma
After relief of acute manifestations of streptoderma, the patient is recommended to undergo a course of physiotherapy. Procedures can cure general and local immunity, regulate metabolism and microcirculation, and promote rapid restoration of the skin.
Methods:
- UV irradiation of the skin;
- UV irradiation of blood;
- laser therapy.
The radiation dose and duration of treatment are selected individually.
Folk remedies
For minor manifestations of streptoderma, traditional medicine can be used as an auxiliary treatment. Some herbal components may cause allergic reactions or do not combine well with pharmacological drugs. Therefore, before use, consultation with a dermatologist is required.
For treatment, plant components with antibacterial, anti-inflammatory, emollient and antiseptic properties are selected.
Oak bark
To prepare the decoction, crushed raw materials (1 tbsp) are poured with water (0.5 l) and boiled for 30 minutes. In the strained and cooled broth, moisten a gauze cloth and apply to the affected areas for 30 minutes 2 times a day.
Yarrow
Dry herb (1 tbsp) is poured with boiling water (250 ml) and steamed in a water bath for 30 minutes. The strained broth is used to treat conflicts 3 times a day.
Honey and pomegranate
To prepare the ointment, liquid honey and juice of unripe pomegranate berries are mixed in equal proportions and left for 3 hours. Apply the product to the affected areas 3-5 times a day.
Hairy hawkweed
The dried herb is ground to a powder. The product is used as a powder on wet surfaces 3-5 times a day.
Series
Dry raw materials (1 tbsp) are poured with water (200 ml) and kept in a water bath for 20 minutes. The strained broth is used as a lotion 3-5 times a day.
Calendula
Dried flowers of the plant (100 g) are poured with 96% medical alcohol, infused in a dark place for 7 days, shaking daily. The strained tincture is used to treat the entire surface of the facial skin 3 times a day.
Garlic
This is a herbal remedy for strengthening and stimulating the immune system. Garlic pulp (200 g) is poured with alcohol (200 ml) and left for 10 days. Shake the container with the product daily. Take 5 drops dissolved in 50 ml of milk 3 times a day. The course of treatment is at least 20 days.
Natural antibiotics
The following plants have a targeted bactericidal and bacteriostatic effect against streptococci: celandine, eucalyptus, cetraria, sage. Decoctions and infusions from plants are used to treat the skin or take them internally. Pine resin is used as a natural ointment.
All components of herbal remedies can be purchased at the pharmacy. In addition, manufacturers offer a variety of herbal preparations to strengthen the immune system, which will be useful for streptococcal infections.
Basic hygiene
With streptoderma, it is important to adhere to specific hygiene. During illness, avoid washing the skin with water in the affected areas and areas close to them.
The spread of infection throughout the body requires a complete refusal of water procedures. When conflicts are localized in areas with hair, the hair is cut off. Shaving is prohibited.
Water procedures are replaced by treating the skin with antiseptic solutions: 1% salicylic acid or 0.1% potassium permanganate. To prevent the spread of infection over large areas, the skin around the inflammation is sprayed with antibacterial agents in the form of sprays. Drugs: Terramycin, Forticlin, Monclavit-1.
All treatment procedures are carried out under sterile conditions, hands are kept clean, and contact of the facial skin with dirty objects is avoided. During illness, you need to avoid synthetic clothing that causes increased sweating.
From this video you can learn about some more methods of treating streptoderma.
Diet therapy
Therapeutic nutrition for streptodemia involves limiting fast carbohydrates and predominant proteins in the diet. It is important to include foods rich in vitamin C and B vitamins in your daily menu.
Exclude from the diet:
- baked goods made from white flour;
- potatoes, starch-containing products;
- sugar in any form;
- sweet carbonated drinks;
- sweet fruits, juices;
- refined products;
- spicy, fried, smoked, fatty foods;
- alcoholic drinks.
The following products will contribute to a quick recovery:
- any berries;
- lactic acid products;
- white cabbage, carrots, garlic, celery, sweet potato;
- parsley, spinach, ginger;
- lemon, coconut;
- whole grains: bread, wild rice, quinoa.
During illness, it is important to maintain metabolism, which is impossible without a drinking regimen. During illness, the following will be useful: herbal decoctions, berry fruit drinks, filtered water.
Hormonal ointments
Such remedies are used in cases of advanced disease. The ointment contains an antibiotic and a hormone; it can only be used for a few days, since its use disrupts the protective properties of the skin. For this reason, ointments are not used for extensive skin lesions. Without hormonal ointments, it is impossible to cope with streptoderma if it is accompanied by eczema, allergic and atopic dermatitis. Popular hormonal ointments for streptoderma:
- Akriderm. Fights allergies, relieves itching and inflammation, and also effectively fights allergic manifestations. It contains the hormone betamethasone. It is applied 2-6 times a day, the course of treatment is 4 weeks.
- Hyoxyzone. Contains the antibiotic oxytetracycline hydrochloride and the hormone hydrocortisone acetate. Thanks to this, it eliminates itching and inflammation. Apply a thin layer of 2-3 r. per day.
- Lorinden S. Contains the corticosteroid flumethasone and the antifungal clioquinol. The remedy is effective when streptoderma is complicated by a fungus.
- Triderm. This ointment contains a hormone, an antibiotic and an antifungal agent. As a result of its use, itching and swelling, as well as an allergic reaction, are relieved. Not for children and pregnant women.
Any of the described drugs against streptoderma should be prescribed by a doctor, taking into account the severity of the disease. In addition to these, the doctor may prescribe medications that accelerate wound healing.
Complications of streptoderma
Dermatologists claim that the main cause of complications with facial streptoderma is self-medication. Most patients prefer to treat local manifestations of pathology on their own, turning to dermatologists only if the infection lasts for a long time and the infection spreads over large areas. This often becomes the cause of chronic pathology.
With long-term streptoderma, there is always a high risk of developing:
- microbial eczema;
- scarlet fever;
- the addition of a staphylococcal infection with damage to internal organs;
- septicemia (bacterial blood infection);
- poststreptococcal glomerulonephritis.
All complications of streptococcal infection pose a serious threat to human life, are difficult to treat and can leave irreversible consequences in the body.
Treatment tactics
Therapy for an infectious lesion is based on its cause and the severity of the inflammatory process. If syphilis is excluded, the underlying disease is eliminated with the help of antibacterial drugs. The patient is registered at the dispensary, all appointments are made on an individual basis. Single ulcers are treated on an outpatient basis; the presence of multiple lesions requires hospitalization of the patient.
If the cause of the disease is a streptococcal or staphylococcal infection, the patient is prescribed systemic antibacterial therapy, in parallel with this, the ulcer is treated, existing endocrine disorders are corrected, immunomodulators, vitamins, and general regenerative agents are used.
The pustules are opened using surgical instruments, and the surgeon removes pus and necrotic masses. Before surgery, oil compresses are used for two to three days. They help soften tight-fitting crusts. In the presence of large ulcerative craters, ointments containing proteolytic enzymes are used for these purposes. They contribute to the dissolution of necrotic masses and the launch of the processes of rejection of shriveled layers.
In the postoperative period, the doctor irrigates the cleaned area and rinses it using disinfectant solutions. The dressing is changed regularly twice a day, after applying antibacterial ointments to the wound. Also, ulcers are extinguished with agents that have astringent-coagulating properties. Silver nitrate, alcohol solutions and tannin are best suited for these purposes.
After the wound begins to heal, drugs are added that can stimulate tissue regeneration. The patient may be prescribed applications with propolis or sea buckthorn oil. Among pharmaceutical products, “” is often used. At this stage, physiotherapy is also indicated. Procedures are prescribed that stimulate wound cleansing, activate local immunity, and stimulate healing processes (laser therapy, ultraviolet irradiation, UHF).
Other types of ecthyma are treated taking into account the etiology of the disease. Therapy for the syphilitic form is based on stopping secondary syphilis. For this purpose, appropriate medical protocols are used. At the same time, local treatment of the wound is carried out, it helps to prevent the addition of a secondary infection and reduce the severity of existing manifestations. The patient is registered at the dispensary; observation of the patient with regular serological monitoring is considered mandatory. Due to the high contagiousness of the underlying disease, contact persons are identified.
Prescriptions for scabies ecthyma and pustular dermatitis are made taking into account the need to destroy the infectious agent. For these purposes, sulfur ointment, benzyl benzoate or spregal can be used during treatment of the ulcer. In this case, it is necessary to disinfect underwear and bed linen, as well as the lesion (in the case of pustular dermatitis).
Prevention
Since the routes of transmission and mechanisms of development of streptococcal skin infections are well known, the basis of prevention is based on the exclusion of predisposing factors.
A patient with an acute form of streptoderma should completely avoid close contact with healthy people and use individual household items.
Prevention rules:
- rational hygiene;
- timely treatment of skin injuries with antiseptic agents;
- exclusion of tactile contact with facial skin;
- balanced diet with daily intake of vitamins;
- regular courses of taking multivitamins;
- constant control over chronic pathologies of the body.
The human immune system has enormous capabilities, daily suppressing the proliferation of numerous bacteria and viruses. Therefore, every person should strengthen it and learn to prevent factors that suppress the body’s protective properties.
The prognosis of streptoderma depends on timely and adequate treatment. In these cases, it is favorable; the pathology in almost all cases ends with recovery. In everyday life, contact with various microorganisms cannot be avoided, and what it will be depends entirely on the person.