Inverted papillomavirus belongs to the group of benign tumors of epithelial origin. It develops most often on the lateral wall of the nasal cavity. The endoscopic method is currently considered the most effective way to remove inverted papilloma of the nose and paranasal sinuses.
It owes its name to a histological image that shows an inversion of the epithelial plane.
Inverted papilloma of the nasal cavity and paranasal sinuses
Do you have difficulty breathing through your nose through one nostril? Or maybe you feel some kind of growth in your nose? You might think it's a harmless wart, but it's not that simple! This can be a very insidious disease - inverted nasal papilloma, which is important to recognize in time!
The tumor has local aggressiveness, which is manifested by locally destructive growth (signs of infiltrating growth without metastases). Histologically, it is characterized by invagination (penetration) of the integumentary epithelium into the underlying stroma. Macroscopically, it has the appearance of a dense polyp with a rough red surface, sometimes papillomatous, lobulated or verrucous.
It spreads and destroys both soft tissue and bone walls, growing into the paranasal sinuses and beyond. Most often, inverted papilloma affects the lateral wall of the nasal cavity in the area of the middle turbinate with nearby sinuses (maxillary and ethmoidal labyrinth cells), less commonly the sphenoid and frontal sinuses. Inverted papilloma is characterized by a high degree of malignancy (malignancy) - 5%.
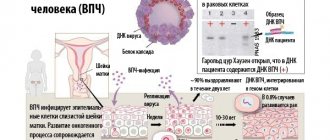
The etiology of inverted papilloma remains unknown to date. Among the causes of its occurrence are allergies, chronic sinusitis and viral infections.
• difficulty or absence of nasal breathing on one side (the earliest symptom);
• presence of discharge from the nasal cavity;
• periodic bleeding from one half of the nasal cavity;
• pain in the face on the affected side;
• feeling of a foreign body in the nasal cavity;
• change in the shape of the external nose as a result of tumor growth.
Diagnosis of inverted papillomas is carried out on the basis of:
Surgical treatment is indicated for all patients with inverted papilloma.
Recurrence rate of inverted papilloma depending on the surgical technique:
• surgery using external approaches (lateral rhinotomy with medial maxillectomy and/or “en-bloc” resection of the lateral wall of the nasal cavity, surgery according to Caldwell-Luc, Murr and Denker) – 12-19%.
Rhinotomy according to Moore's method for tumors of the nasal cavity.
The skin incision begins at the medial end of the eyebrow, continues down along the nasobuccal groove and ends around the nasal wing. To provide wider access, in some cases it is advisable to continue the incision to the midline, cross the upper lip and, by making an incision along the transitional fold of the upper lip, separate the soft tissue of the cheek from the facial surface of the upper jaw. Using hooks, pulling the soft tissues of the cheek separated from the bone in one direction, and the wing of the nose and the tissues of the side wall of the nose in the other, opens access to the corresponding half of the nasal cavity and the maxillary sinus. Then, using a chisel and bone forceps, the frontal process of the upper jaw and the nasal bone are resected. If there is a process in the maxillary sinus, its medial and facial walls are also resected. Thus, a wide path opens to the nasal cavity and maxillary sinus, which also provides the possibility of intervention on the ethmoidal labyrinth and even on the main sinus.
If necessary, increasing the soft tissue incision upward along the line of the superciliary arch, access to the frontal sinus and orbit is opened. The tumor, along with the affected parts of the facial skeleton, is removed electrosurgically. At the end of the surgical intervention, the surgical wound is tamponed, the end of the tampon is brought out through the nostril, and sutures are placed on the skin incision. The tampon is usually removed 4-5 days after surgery. Further treatment is reduced to daily rinsing of the nasal cavity and maxillary sinus with solutions of hydrogen peroxide, rivanol or antibiotics. This kind of washing has to be done for a long time, since as a result of electrocoagulation, slow rejection of necrotic bone occurs, which is accompanied by the release of inflammatory exudate with an unpleasant odor. The cosmetic result of rhinotomy using the Murr method is quite satisfactory. After healing, an inconspicuous pale scar and slight retraction of tissue in the area of the nasolabial fold remain.
Inverted transitional cell papilloma must be differentiated from antral choanal polyp, squamous cell carcinoma, and adenocarcinoma.
Therefore, you should immediately contact an ENT doctor if the above symptoms occur, and also take seriously the choice of method for removing inverted nasal papilloma to reduce the possibility of relapses.
Signs of pathology
Papilloma in the nose is determined by signs characteristic of skin pathology. The following symptoms indicate the presence of a growth in the olfactory organ:
- Congestion of one nasal passage. It occurs due to the fact that too large a papilloma blocks the lumen through which air passes during inhalation. This symptom indicates the development of pathologies of all types;
- Unnatural discharge from one nostril. This symptom is explained by a failure of the mucus distribution process and increased secretion of the glands;
- Nosebleeds. They must be one-sided. Blood comes from the nostril in which the growth is located;
Surgery for inverted papilloma of the nasal cavity
Neoplasms are best removed by surgery
. Drug treatment very often does not produce results, causing frequent relapses: degeneration of formations into malignant tumors, difficulty breathing.
Elimination of neoplasms is carried out using surgical intervention. Modern medicine identifies several methods for removing formations. The doctor chooses one or another method of removal, taking into account the location and extent of the tumor.
The following methods of surgical treatment are distinguished:
- Open surgery. In medicine it is called Denker's operation. The surgeon uses a scalpel to open the nasal cavity, removing the growth along with the affected tissue. After that it is stitched up. The post-operative recovery period is painful and takes several weeks. It is used for a large number of neoplasms.
- Endoscopic removal. An endoscope is inserted, which allows visual monitoring of the operation. Together with the endoscope, an instrument is inserted that cuts and cauterizes the papilloma. Today this method is the most popular and effective. During the operation, the patient receives minimal damage, which significantly speeds up recovery.
- Removal using laser. Most often used to remove growths that are not deep in the nasal cavity. The recovery period is very short, since the wound is immediately cauterized. Do not use in case of large numbers of formations.
- Removal using a loop. A loop, similar to a string, is put on the growth, cutting it off just under the stem. After this, the cut site is cauterized with a laser beam or diathermocoagulation.
- To remove tumors in children, the doctor chooses a more gentle method, taking into account the age and individual characteristics of the patient.
- Surgical removal is necessarily supplemented by taking antiviral drugs that should destroy HPV.
Therapeutic measures
It is strictly forbidden to remove papillomas yourself. Only a specialist can prescribe appropriate treatment based on the results of a diagnostic examination.
Conservative therapy
Most often, patients are recommended to use keratolytic agents. This could be Lapis, Solcoseryl ointment or Salipod patch. Necrotizing drugs are also prescribed, for example, Condilin or Vartek.
To eliminate the inflammatory process, oxolinic ointment, which has an antiviral effect, is recommended.
In addition, the doctor prescribes immunomodulators. Conservative treatment should last until the characteristic signs of the pathology completely disappear.
Surgical intervention
Surgical removal is indicated when medications do not give a positive result. One of the following methods may be used.
Laser
It is considered one of the most effective and painless techniques. A distinctive feature is that after laser treatment there are no marks left on the skin.
Cryodestruction
The wart is treated with nitrogen, which has a destructive effect on it. The method allows you to remove papillomas from inside the nose and from its surface.
Radio knife
After removal in this way, relapses, as a rule, do not occur.
Electrocoagulation
The neoplasm is affected by electrofrequency pulses. The procedure is prescribed in the presence of even fairly large growths.
Scalpel
This method is currently used in rare cases. The main disadvantage is the scars after surgery.
Drug treatment of inverted nasal papillomas
In the first stages of the disease, treatment can be carried out using topical medications. Such drugs have a destructive effect that causes the death of neoplasm cells.
Experts recommend the following topical medications:
- Vartek. The active substance of this medicine is podophyllotoxin. The drug causes the death of pathological tissues. The drug is prohibited for use by pregnant and lactating women, as well as children under 12 years of age.
- Solcoderm. This medicine is in the form of a solution. It consists of a combination of various acids and copper nitrate. The drug cauterizes, causing the death of pathological tissues, resulting in necrosis of the growth.
- Verrucacid. Consists of a combination of phenol and metacresol. Causes protein coagulation and gradual death of tumors.
- Cryopharma. This is a drug that can be used at home. It contains dimethyl ether, safe propellants and propane.
Important addition: What does a wart look like?
Medicines that melt the tissue of growths are successfully used:
- Kolomak. It contains a mixture of salicylic and lactic acids.
- Salipod is a special patch whose active ingredient is salicylic acid.
- Pencil for skin growths Lapis.
- Simultaneous use of two ointments: Oxolinic - actively fights viruses, Salicylic - destroys cells of formations.
Surgery
The method of surgical removal is selected individually, depending on the severity of the clinical case, the size of the formation, and the intensity of the symptomatic picture. Papilloma can be removed in the following ways:
- cryotherapy: cauterization method with liquid nitrogen;
- laser;
- cauterization method - electrocoagulation;
- endoscopic manipulation;
- radical surgery.
Cauterization with electrocoagulation, liquid nitrogen or laser removal is carried out using the same system - first a local anesthetic is administered, since a large number of nerve endings pass through the mucous membrane, then manipulation is carried out. The procedure itself is painless, but a person may experience a feeling of discomfort during it.
Upon completion of the operation, the mucous membranes on which the papilloma was located are treated with antiviral solutions. The removal method by cauterizing the growth helps when there is only one papilloma. For multiple formations, endoscopy or open surgery is performed.
Preference in the surgical treatment of formations in the nasal sinuses is given to a minimally invasive method - endoscopy. This technique does not carry the risk of injury to healthy soft tissues and blood vessels. The advantage of endoscopy is that no incisions are required to insert surgical instruments.
What space-occupying lesions can be confused with Schneiderian papilloma
Retention cyst
— Volumetric formation with no enhancement and smooth boundaries
Retronasal polyp
— Round polyp arising from the maxillary sinus, without significant contrast enhancement
Angiofibroma of the nasopharynx
— Young age of patients
-Forms in the nasopharynx and spreads into the pterygopalatine fossa
Malignant tumors (eg, squamous cell carcinoma)
— Direct signs of a malignant process
-Sometimes it is impossible to distinguish from papilloma
- Complete removal
- In addition to the classical approach - resection of the upper jaw - endoscopic techniques are increasingly used.
ENT. He to. Transitional cell papilloma.
Inverted transitional cell papilloma
(syn.: Schneider's papilloma, epithelial papilloma, papillary fibroepithelioma, papillary sinusitis, columnar cell papilloma, papilloma of the respiratory epithelium) is a rare, but characteristic benign tumor of the nasal cavity and its sinuses, accounting for about 0.5% of the findings of all nasal tumors. It is more common in men, mainly in the fifth or sixth decade of life. Usually unilateral, this tumor can be single or multiple. As a rule, it occurs on the lateral wall of the nasal cavity, as well as in the paranasal sinuses: the maxillary cavity, the ethmoidal labyrinth, and occasionally in the frontal and sphenoid sinuses. With combined lesions, the localization of the primary node is almost impossible to establish. From the nasal cavity, a tumor can grow into the paranasal sinus and vice versa. Patients usually complain of nasal congestion, discharge, nosebleeds, and pain in the facial nerve area. Sometimes bone tissue is destroyed in the area of tumor growth. The walls of the maxillary sinus are most often affected. But the tumor can grow in other directions, destroying the wall of the palate, the walls of the orbit, or the bones of the base of the skull. Tumor relapses can occur after 5-10 years. In approximately 5% of patients, inverted transitional cell papilloma can turn into cancer after a long-term benign course. Metastases are not observed.
Macroscopically soft
, with folds, the tumor has a lobulated, papillary structure, a rough surface. The color of its fabric varies from pink to yellow-red. Inverted transitional cell papilloma recurs in 75% of cases if local excision is performed. For optimal treatment when the tumor is localized on the lateral wall of the nasal cavity, lateral rhinotomy and midline resection of the maxilla are recommended. If such a papilloma becomes malignant, its clinical course becomes more aggressive.
Under the microchip the surface of the tumor
uneven due to many deep cracks and folds. They are covered with a thick layer of epithelium, reminiscent of the lining of the urinary tract. Three zones can be distinguished in it. The relatively narrow basal zone consists of small and dark cells. Most of them have a slightly elongated shape and their long axis lies perpendicular to the poorly developed basement membrane. The underlying connective tissue protrudes into the epithelium in places, forming papillae rich in capillaries. The intermediate zone is represented by large light cells, forming many layers. Their nuclei are round or slightly irregular in shape, and the area of cytoplasm adjacent to the nucleus appears optically empty. The closer to the surface, the larger and lighter the epithelial cells and the better the intercellular boundaries are identified. Finally, the narrowest and not everywhere pronounced zone consists of flattened cells with oxyphilic cytoplasm and hyperchromic nuclei. In addition, the papilloma epithelium forms many outgrowths into the underlying connective tissue. The epithelial layers in some areas of the tumor are bordered by prismatic epithelium or have a lumen in the center, limited by prismatic cells secreting mucus. Microcysts containing small amounts of mucin or neutrophils may be scattered throughout the neoplastic epithelium. There are few mitotic figures, and they occur in the basal zone of the tumor epithelium. Nuclear polymorphism is observed in approximately 10% of cases. The fibrous stroma may be edematous, loose, rich in capillaries, and lightly infiltrated with lymphocytes and plasma cells. Sometimes lymphoid follicles are found. There are no normal glands in the stroma.
With malignancy,
First of all, hyperplasia of the basal cells occurs. They acquire an elongated shape, displace higher lying cells and intensively divide by mitosis. Then foci of dysplasia appear in the superficial zone. Stratification (layered epithelium), polymorphism and mitotic activity of epithelial cells increase. When the entire epithelial layer is replaced by polymorphic and atypical cells, we are talking about carcinoma in situ. The latter may have a spindle cell character or, with very pronounced polymorphism and the appearance of individual mononuclear giant cells, a bowenoid character. In all types of carcinoma in situ, the basement membrane is preserved throughout.
Inverted transitional cell papilloma
must be differentiated from antral choanal polyp squamous cell carcinoma and adenocarcinoma.
Traditional methods of treatment
Over the centuries, traditional medicine has learned to fight tumors. The following effective treatment methods can be identified:
- Fresh celandine juice is the most effective remedy that should be lubricated with the growth several times a day.
- Fresh forest mushrooms - they contain enzymes that destroy HPV.
- The grated lemon peel must be steeped in 30% vinegar for 7 days. A piece of cotton wool is soaked in the resulting infusion and placed in the nose overnight.
- Grate fresh horseradish on a fine grater and apply the resulting pulp to the growth using cotton wool overnight. After 7-8 sessions the formation disappears. It is worth noting that the procedure is accompanied by a burning sensation.
Important addition: Phosphogliv for psoriasis
Recent Entries
- HELMINTHOX for papillomas: a broad-spectrum anthelmintic!
- Nopapilom for papillomas and warts: will get rid of growths quickly, safely, delicately!
- Top 5 drugs for papillomas and warts: painless relief from all types of growths on the skin!
- Panavir is a remedy for papillomas: it affects not only the external signs of the disease, but also the cause itself!
- Formu Clear patches for papillomas and warts: guaranteed to get rid of skin growths!
ATTENTION! Information about drugs and folk remedies is presented for informational purposes only. Under no circumstances should you use the medicine or give it to your loved ones without medical advice! Self-medication and uncontrolled use of drugs are dangerous for the development of complications and side effects! At the first sign of illness, you should consult a doctor
- Feedback
- Privacy Policy
2019 Papillomas and their treatment
- Papillomas
- Warts
- Removal
- Types and places of papillomas In intimate places
- In pregnant women
- In children
Types and symptoms of nasal papillomas
Neoplasms differ both in appearance and histological structure. Depending on their type, as well as on location, the clinical signs of the disease will be determined.
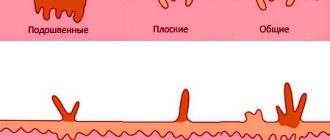
According to the degree of differentiation (degree of maturity) of cells, the following types of growth are distinguished:
- Expansive growth. Tumor cells are mature and tend to grow toward the cavity—outward. The appearance resembles a common wart. With expansive growth, already in the early stages there is a pronounced difficulty in breathing due to the filling of the nasal cavity with papillomatous masses.
- Invasive growth. The cells have an intermediate (transitional) degree of maturity; the neoplasm grows into the underlying cartilage and bone tissue of the walls of the nasal cavity, orbits, and skull. Inverted papilloma is manifested by pain in the nose and sinus area (forehead, upper jaw), frequent bleeding, and loss of smell.
- Appositional growth. The tumor grows into the submucous membrane. The tumor seems to spread along the nasal passages. Its cells are immature and can become malignant. Tumors with appositional growth manifest clinically at later stages and do not make themselves felt for a long time. In the early stages, you may experience nasal congestion and bleeding.
Viral tumors also differ in appearance:
- Cylindrical – elongated, oblong appearance.
- Inverting - tumors that grow into the walls of the nasal passages.
- Mushroom-shaped - intensively filling the free nasal space.
Inverted papilloma of the nasal cavity, which has invasive growth, deserves special attention. The tumor is benign in its histological structure, but clinically it has all the signs of malignancy. It destroys the walls of the nose, septum, eye sockets, paranasal sinuses, walls of the ethmoid labyrinth, and can grow into both cartilage and bone.
When papillomas form in the nose, people note the following symptoms:
- feeling of heaviness and foreign body;
- periodic bleeding;
- mucous, mucopurulent discharge from the nose;
- nasal voice;
- impaired perception of smells;
- headache.
- difficulty breathing and nasal congestion.
Diagnostics
To make an accurate diagnosis, it is necessary to undergo a comprehensive examination, during which it will be possible to determine the type of benign formations and the strain of the virus that provoked their development.
For an initial examination, you must contact an otolaryngologist. If there is a suspicion of the presence of growths inside the nasal cavity, the patient is prescribed additional research methods.
Biopsy
The technique involves examining tissue fragments taken from the sinuses to determine the formation of cancer cells. PCR is used to detect human papillomavirus.
MRI and CT
Prescribed if the previous diagnostic method confirmed that there are growths of the inverted type. The main feature of such papillomas is their growth into bone and cartilage tissue.
Rhinoscopy
During the procedure, a small tube with a built-in microscope is inserted into the nasal passages. This makes it possible to give an adequate assessment of the condition of the nasal mucosa and establish the formation of growths, as well as their size and other parameters.
Inverted papilloma of the nasal cavity
Tumors of the ethmoid sinuses
are accompanied by an outward displacement of the eye, and later exophthalmos occurs. Early eye movements are limited due to dysfunction of the internal rectus and superior oblique muscles. Obstruction of the lacrimal ducts leads to persistent lacrimation. Nasal breathing is impaired.
Tumor growth
in the posterior ethmoid cells, its spread into the orbit is accompanied by a decrease in visual acuity and the appearance of a central scotoma in the field of view. As a rule, there are no changes in the fundus; exophthalmos does not exceed 4-5 mm. An increase in exophthalmos due to the continued growth of the tumor and a sharp outward displacement of the eye leads to a limitation of its mobility in all directions.
Changes may occur during this period
in the fundus, caused by impaired venous outflow. A tumor spreading at the apex of the orbit can spread to the superior orbital fissure, squeezing the nerve trunks, which is accompanied by a painful headache, shooting pain in the eye, and superior orbital fissure syndrome may develop.
Isolated malignant tumors of the main sinus are rare. Axial exophthalmos is preceded by headache and limitation of the functions of extraocular muscles. Along with exophthalmos, visual disturbances occur. In the fundus there is a congestive optic disc. The clinical picture of a malignant tumor of the main sinus is not much different from a primary malignant tumor in the orbit.
The most difficult differential diagnosis of nasopharyngeal tumors is
, which already at an early stage of development cause ophthalmological symptoms: dysfunction of extraocular muscles, mainly external, unilateral exophthalmos. In 2/3 of patients, ocular symptoms occur simultaneously with signs of damage to the trigeminal nerve.
Localization of the tumor process
between the apex of the pyramid and the superior orbital fissure leads to dysfunction of the external rectus muscle, and the symptom of damage to the abducens nerve is the most common sign of malignant tumors of the nasopharynx. Partial paresis of the oculomotor nerve contributes to the appearance of ptosis on the affected side. Treatment of such patients is carried out in specialized otorhinolaryngological departments.
Among secondary benign tumors
the orbits distinguish inverting papilloma, osteoma, osteoblastoma, ossifying fibroma and brown tumor. The pathogenesis and histogenesis of these tumors are different, but the clinical symptoms are similar.
Inverting papilloma
- benign epithelial tumor of the nasal cavity and paranasal sinuses has synonyms: squamous papilloma, hypertrophic papilloma, papillary sinusitis, epithelial papilloma, Schneiderian papilloma. We observed an inverting papilloma growing from the mucous membrane of the frontal sinus.
Having invasive growth
, inverting papilloma can transform into malignant carcinoma with the formation of metastases to regional lymph nodes. The patient dies as a result of tumor growth into the cranial cavity. Particularly dangerous in this regard is the localization of the tumor in the sinuses of the ethmoid bone and in the frontal sinus. The duration of the disease is calculated in years. The tumor often grows into the orbit, invading the orbital tissue. Clinical symptoms depend on the location of the tumor in the orbit, but almost always there is a displacement of the eye in the direction opposite to the tumor localization and exophthalmos.
Treatment of inverting papilloma
surgical. After local removal, the tumor recurs. The intervals between relapses decrease over time. We observed a patient who, after the first operation for inverting nasal papilloma, lived for 8 years, underwent another 5 operations (2 in the ethmoid sinuses, 3 in the frontal sinus and orbit), and died after 5 months. after exenteration of the orbit from the spread of the tumor into the cranial cavity. This observation illustrates the possibility of a poor prognosis in case of relapse of papilloma.
Important addition: How to eat ginger for psoriasis
The article was written based on materials from the sites: otpapillom.ru, www.riyad-ruf.ru, volynka.ru, lor-clinica.com, meduniver.com.
Signs of a benign tumor of the nasal cavity on CT and MRI images
Is MSCT of the nasal sinuses informative for inverted papilloma?
- Unilateral tumor with soft tissue density
- Affects the lateral wall of the nose
- Lobed surface
- After administration of contrast, tortuosity of the folds of the mucous membrane is revealed
- There may be calcifications inside the papilloma
- A slow-growing tumor that can cause bone erosion.
What MRI images of the paranasal sinuses will show for papilloma
- Low signal intensity on T1-weighted image and moderately increased signal intensity on T2-weighted image
- On a T2-weighted image, the signal structure is heterogeneous, which is more clearly visible after gadolinium administration (as on CT)
- Necrosis in the center of the papilloma or infiltration of surrounding structures are likely signs of malignant degeneration.
Specific signs
- The tumor at the level of the middle turbinate has soft tissue density
- Obstruction of the foramina leads to darkening of the frontal and maxillary sinuses and the anterior cells of the ethmoidal labyrinth
- Typical tortuosity of mucosal folds on CT or MRI after contrast/gadolinium injection.
Causes of papilloma on the inside of the cheek
The main reason for the occurrence of such a neoplasm here is the penetration of the papilloma virus into the body. If it gets on the mucous membranes of the oral cavity and does not encounter obstacles on its way, then sooner or later it provokes the appearance of a growth.
Here's what can trigger the process of papilloma formation on the cheek in the mouth:
- Kisses with infected people. HPV does not tolerate being outside the human body very well, but during such contacts it gets inside safely. This is especially true if there is a large accumulation of saliva and if there are traces of blood in the oral cavity, where the concentration of the virus is quite high.
- Oral sexual contact. First of all, those whose partners have papillomas on the phallus or on the female genital organs are susceptible to infection with HPV in this way. The virus is located inside these formations and when the oral mucosa comes into contact with the tissues in these places, it easily migrates. In the absence of proper treatment, the process of formation of papilloma on the cheek in the mouth begins.
- Low level of personal hygiene. This applies to those who ignore mouth rinses, which should be used to eliminate bacteria. This also applies to those who do not brush their teeth well enough. Using someone else's brushes that have traces of HPV on the surface can also lead to the appearance of a formation on the cheek. Since it is always contained in the saliva and blood of an infected person, the likelihood of papilloma formation on the inside of the cheek is very high.
- Sharing utensils with the patient. If cups, spoons, forks, knives, plates, pots and other similar household items are not washed well, then the papilloma virus may remain on them. That is why a healthy person who eats food with their help can easily become a carrier of HPV.
Using contaminated objects and kissing sick people does not necessarily cause papillomas to appear on the inside of the cheek. This occurs only if the level of immunity decreases and its response to viral attacks worsens. This, in turn, is caused by a lack of vitamins C, E, A, iron, zinc and a number of other useful substances.
The cause of deterioration of immunity and the formation of papilloma on the buccal mucosa can also be stress, chemotherapy and radiation therapy, long-term treatment with hormones, uncontrolled use of antibiotics, which worsens the intestinal microflora. Poor environment, lack of sleep, colitis, gastritis and other stomach diseases can also increase the likelihood of the formation of such a growth.
Causes
Papillomas are formed as a result of HPV infection. After infection, there is a high probability of a benign growth appearing.
On this topic
- ENT organs
Non-surgical methods for treating tonsil cysts
- Olga Vladimirovna Khazova
- December 3, 2021
The virus can enter the human body in several ways:
- airborne;
- contact;
- during labor from mother to child.
Once the virus has entered the body, it remains there for the rest of its life. Under the influence of provoking factors, the virus is activated, against the background of which pathological cells of the nasal tissues begin to grow.
The main provocateurs that can provoke the growth of tumors include:
- frequent colds;
- chronic respiratory pathologies
- deficiency ;
- staying in poorly ventilated areas with high air humidity for a long time;
- treatment with hormonal drugs;
- frequent stressful situations;
- excessive fatigue of the body;
- alcohol abuse and smoking;
- decreased immune system.
On this topic
- ENT organs
The best ways to remove a maxillary sinus cyst
- Olga Vladimirovna Khazova
- July 9, 2021
According to observations, experts have come to the conclusion that most often the virus is diagnosed in the winter-spring period, when human immunity decreases as a result of insufficient intake of vitamins and nutrients into the body.
In addition, according to otolaryngologists, if immunity to the virus has stabilized, the disease begins to regress three years after its first appearance. Based on this, we can conclude that the main cause of the disease is a weakened defense system of the human body.