Acne can be a manifestation of internal diseases, hormonal imbalance, nutritional disorders and improper diet. Does staphylococcus cause acne on the face? In some cases, the cause of acne is pathogenic bacteria. Of particular danger is Staphylococcus aureus, which is difficult to treat and causes a lot of inconvenience to the patient.
After all, acne is primarily a cosmetic defect, which significantly reduces self-esteem, causing dissatisfaction with appearance, leading to isolation and the emergence of complexes.
What is staphylococcus and where does it live?
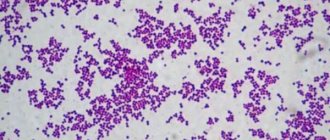
Staphylococcus is a bacterium that lives in colonies that visually resemble a bunch of grapes. There are about two dozen different strains of these microorganisms, but only a few species are dangerous to humans. The leader among them is Staphylococcus aureus, so named due to its pigment and related to opportunistic bacteria. It can live inside human organs and on the surface of the skin for years without causing harm. Colonies of this bacterium prefer to live in the mouth, nose, and other mucous membranes and are part of the natural microflora of the skin, but under normal circumstances they do not cause diseases.
Changes in environmental conditions provoke the active proliferation of staphylococci, which becomes the cause of staphylococcal infection. This concept does not denote a specific pathology, but is a general term. Living in various organs, this bacterium causes many diseases, and having the ability to travel with lymph and blood throughout the body, it can affect all systems.
How does staphylococcus act on organs:
- Causes dysbiosis in the intestines.
- On the skin - pyoderma (purulent rashes, boils, necrolysis).
- Blood poisoning - sepsis.
- In the nasopharynx it provokes sore throat and tonsillitis.
- In the lungs it causes pneumonia.
- A bone marrow disease caused by staphylococcus is called osteomyelitis.
Staphylococcus aureus can affect almost every organ and system of the human body. If you find purulent rashes on the skin, do not self-medicate, but visit a doctor to prevent the spread of infection. In a weakened body, staphylococcus can cause death without proper treatment.
What to do if acne is caused by staphylococcus – Beautician online
Probably everyone has heard that there is such an infection as staphylococcus. Unfortunately, it still often thrives in maternity hospitals, children's hospitals and medical institutions.
And it causes various diseases, some of which require serious treatment. But not many people know that staphylococcus can cause acne to appear constantly on the face without other symptoms usually accompanying it.
How this happens and what to do about it - let's figure it out.
Staphylococcus aureus is considered one of the most common and dangerous. It is named so because under a microscope its clusters resemble golden yellow grapes. But there are other varieties of these gram-positive bacteria:
- Epidermal - found on human mucous membranes, is opportunistic.
- Saprophytic - usually infects the genitourinary system and provokes urethritis, cystitis, etc.
- Hemolytic – when released into the blood, it causes sepsis, endocarditis, and damage to the urethra.
Doctors called the form of Staphylococcus aureus, which cannot be treated with traditional antibiotics, methicillin-resistant. This is the most dangerous type of bacteria, resistant to broad-spectrum drugs.
Main symptom
The main symptom to suspect staphylococcus is acne. Moreover, they can take a variety of forms:
- fluid-filled blisters;
- large red spots (erysipelas);
- boils and carbuncles;
- phlegmons, pustules, abscesses, etc.
It can be very difficult for a non-specialist, and sometimes even an experienced doctor, to recognize staphylococcus at first glance at the skin. However, its characteristic manifestations still exist.
https://www.youtube.com/watch?v=ARu6i7bxOWY
Most often the disease develops as follows:
- first, a red dense tubercle forms, painful when touched;
- it has a cone-shaped shape, at the top of which a white rod gradually forms;
- after ripening, whitish-yellow or green pus comes out of it;
- the skin is affected to a great depth, which causes quite severe pain;
- Intense redness and swelling develop around the pimple.
The most unpleasant thing is that closely spaced acne can merge with each other, forming entire purulent conglomerates. After them, scars often remain, especially if you squeeze out immature pimples with your hands.
Features of the disease
The most pathogenic Staphylococcus aureus has its own characteristics in different groups of people, which are important to know about. Although in general the treatment regimen looks approximately the same, doctors must take into account the points listed below.
In adults
Most often, staphylococcus begins to manifest itself when the immune system is weakened or exacerbation of existing chronic diseases. Women typically experience an increase in acne due to staphylococcus before menstruation. During this period, the face can literally become covered with them, and from days 5-7 of the cycle the number of rashes decreases.
Provoking factors that can act as a trigger and cause the appearance of staphylococcal acne on the skin are also:
- severe hypothermia, colds, ARVI;
- skin trauma, including during shaving;
- autoimmune and oncological diseases, HIV;
- severe hormonal imbalance;
- increased sweating and oily skin;
- abuse or use of someone else's decorative cosmetics;
- failure to comply with basic rules of personal hygiene.
Most often, acne caused by staphylococcus appears on the face. But often the hairy part of the chest, the area around the nipples, armpits, back, and delicate intimate area are affected.
In infants
For them, Staphylococcus aureus is especially dangerous, since newborns do not yet have a strong immune system. They may not have the characteristic small purulent staphylococcal acne, but one of its other forms will appear:
- Richter's disease. The infection affects large areas of the epidermis with its subsequent detachment. Moreover, this form of the disease is caused by a certain type of toxin - exfoliatin, which the baby is not yet able to cope with on his own.
- Pemphigus of newborns. Externally it has some similarities with chickenpox. It is also characterized by the formation of many fluid-filled bubbles. But when they burst, inflamed purulent wounds form in their place. With this form, the risk of sepsis is very high.
Moreover, a baby can become infected with the bacteria in the womb, but more often this happens during childbirth due to the negligence of staff or failure to maintain sterility in a medical institution and especially in the delivery room.
In men
Sycosis – this type of disease most often occurs in men. It has a clearly defined localization - around the mouth, on the chin and in the cheek area - exactly where stubble is usually shaved. Sometimes the infection spreads to the scalp.
Purulent inflammation affects the hair follicles. This can lead to their death and the development of alopecia. Unfortunately, in this case one begins to suspect the presence of staphylococcus quite late, when the disease is already rapidly progressing. At this stage, it is difficult to treat and often relapses.
What is the danger
Opportunistic forms of Staphylococcus aureus can be present on the human body and mucous membranes almost constantly. But a strong immune system prevents them from actively reproducing and causing significant harm to the body. Bacteria cause toxins, but the body eliminates them naturally.
As soon as the immune system weakens for any reason, colonies of bacteria begin to grow rapidly, sometimes affecting quite large areas. If left untreated, they can cause the following serious problems:
- Food poisoning - when a large number of bacteria enter the intestines.
- Bacterial pneumonia, if the mucous membranes of the mouth, larynx and bronchi are affected.
- Bronchitis is when bacteria nest in the nasopharynx or oral cavity.
- Endocarditis is inflammation of the heart sac when staphylococcus enters the blood.
- Meningitis is an inflammation of the mucous membranes of the brain and also occurs from infected blood.
- Osteomyelitis is a purulent-necrotic process in cartilage and bone tissue.
But the worst thing is if staphylococcus provokes sepsis - a general blood infection. In this case, in the absence of qualified medical care, the patient dies literally within a few days.
What to do
If you suspect that acne and other skin problems on the face are caused by staphylococcus, go to the doctor. Do not self-medicate under any circumstances, and even more so, do not take antibiotics without a prescription. If you choose the wrong drug, you will only create an even more favorable environment for the pathogenic bacteria and weaken the immune system.
We take tests
After the initial examination, the doctor will definitely send you to a clinical laboratory for a bacterial culture. A sterile stick is used to take a scraping from the skin or mucous membrane and place it in a sterile environment. This analysis takes several days, during which only external measures can be taken to prevent the spread of the disease and severe deterioration of the skin condition.
Please note that the sample is tested not only for the presence and type of staphylococcus. The laboratory will also determine which group of antibiotics he reacts to most positively. And only after this the doctor will select a medicinal drug individually for you. Usually this is a combination of products for internal and external use, which I will deliberately not list.
Remove acne
Until the immune system is strengthened and the colony of bacteria is significantly reduced, it will not be possible to completely remove rashes caused by staphylococcus. But temporary measures can be taken.
Alas, most effective salon treatments for acne and acne are contraindicated in this case. As well as the usual folk remedies: peelings and many masks.
All this will contribute to the spread of infection to new areas of the skin.
| Way | Description |
| Pimples can be burned | For this, essential oils, alcohol tinctures (calendula, St. John's wort, propolis) or ordinary brilliant green are used. |
| Clay applications | They can be done very carefully, only in places where acne accumulates. Cosmetic clay is an excellent adsorbent with powerful anti-inflammatory and antibacterial properties. |
| Zinc ointment | Has an excellent drying effect. It promotes rapid healing of wounds remaining after the pus is released. |
| "Bepanten" and other drugs with panthenol | Relieves swelling, redness and inflammation, stimulates tissue regeneration. |
| Cosmetics with triclosan | It also helps to quickly get rid of pathogenic microflora. But keep in mind that it cannot be used for a long time. |
All this is used only in parallel with medications prescribed by a doctor. Otherwise, you will only get a temporary effect, and not always.
We are introducing general strengthening measures
To strengthen the body's own defense, it is simultaneously recommended to take immunomodulators and complex multivitamin preparations. At the same time, you must adhere to the following rules:
- completely eliminate alcohol and, if possible, stop smoking;
- limit exposure to ultraviolet radiation to the affected areas of the skin as much as possible;
- do not visit the sauna, swimming pool, solarium during active treatment;
- do not swim in open water or too hot water;
- do not get too cold and try not to sweat too much;
- remove spicy, fatty and fried foods, coffee and chocolate from the diet;
- eat fresh vegetables and fruits every day;
- drink at least 2 liters of pure still water per day.
To avoid infecting your loved ones, use a separate bed, towel and other hygiene items. After washing, it is advisable to iron your child’s clothes with a very hot iron. This reduces the likelihood of re-infection.
Summing up
According to reviews from some of my clients who tried to independently treat acne from staphylococcus, often even the usually effective broad-spectrum antibiotics, for example, Amoxiclav, do not give the expected result. Meanwhile, the bacteria mutate and become even stronger, provoking a new batch of rashes. That is why it is so important to get rid of them only under the supervision of a specialist.
Source: https://ckcentre.ru/zdorove-kozhi/chto-delat-esli-pryshhi-ot-stafilokokka.html
Conditions for the occurrence of staphylococcal infection
The described microorganism is cunning and is able to remember and adapt to the action of antibiotics. That is why it is often called a disease of hospitals. He is a permanent resident of maternity hospitals, despite their sterility. Therefore, the first category of people who are carriers of Staphylococcus aureus are doctors. To prevent the spread of infection, medical workers undergo preventive examinations twice a year.
An increase in the activity of staphylococci provokes a decrease in the protective functions of the body. The reason for this is:
- A viral infection that suppresses the immune system (from the common cold to HIV).
- Pregnancy.
- Unhealthy diet, which contains chemically processed and genetically modified foods.
- Infancy, when the child’s own immunity is still practically absent.
- Frequent injections (taking insulin, hemodialysis, drug addiction).
Sources of infection:
- teeth affected by caries;
- inflammation in the nasopharynx (tonsils, adenoids);
- purulent processes in the ears;
- eye diseases (conjunctivitis, stye);
- purulent lesions of the epidermis (boils, acne, folliculitis).
The main reason that provokes the activation of staphylococcus is weakening of the immune system due to acute and chronic diseases, pregnancy and other reasons. A healthy, strong body is able to live with colonies of Staphylococcus aureus without harming itself.
What is the danger
Opportunistic forms of Staphylococcus aureus can be present on the human body and mucous membranes almost constantly. But a strong immune system prevents them from actively reproducing and causing significant harm to the body. Bacteria cause toxins, but the body eliminates them naturally.
READ ALSO: What to read in the evening for a young woman
As soon as the immune system weakens for any reason, colonies of bacteria begin to grow rapidly, sometimes affecting quite large areas. If left untreated, they can cause the following serious problems:
- Food poisoning - when a large number of bacteria enter the intestines.
- Bacterial pneumonia, if the mucous membranes of the mouth, larynx and bronchi are affected.
- Bronchitis is when bacteria nest in the nasopharynx or oral cavity.
- Endocarditis is inflammation of the heart sac when staphylococcus enters the blood.
- Meningitis is an inflammation of the mucous membranes of the brain and also occurs from infected blood.
- Osteomyelitis is a purulent-necrotic process in cartilage and bone tissue.
But the worst thing is if staphylococcus provokes sepsis - a general blood infection. In this case, in the absence of qualified medical care, the patient dies literally within a few days.
Who diagnoses the disease and what tests are taken
Depending on the area where the bacteria are localized, the following doctors can diagnose a staphylococcal infection:
- Dermatologist, if purulent red pimples and boils are found on the surface of the skin.
- Otolaryngologist for diseases of the nasopharynx and ears.
- Ophthalmologist, when the infection manifests itself as eye disease.
- Gastroenterologist for complaints of problems with the digestive system.
- Gynecologist if rashes or other problems of the genitourinary tract are detected. This disease is especially dangerous for a pregnant woman.
- In infants and older children, the disease is diagnosed by a pediatrician.
It is impossible to determine the disease by eye. You will have to undergo tests that will reveal not the very presence of staphylococcus (it is constantly present in the body), but an excess of its number above the norm.
When inflamed purulent pimples form on the face and body, the contents of the abscess are donated for culture. In parallel, if symptoms of a staphylococcal infection appear on the skin of the face, it is recommended to visit a dentist and ENT doctor to exclude the presence of a source of infection in the organs for which they are responsible. To diagnose this disease, cultures are taken from the mucous membranes of the mouth, nose, and vagina. The activation of the proliferation of these microorganisms in the intestines is determined by stool culture. The results of laboratory tests are prepared for a week, after which the sensitivity of a particular species to antibiotics is determined and the vector of treatment is determined.
Staphylococcus manifests itself on individual organs and treatment is prescribed by the doctor responsible for them. Regardless of where the infection is localized, therapy is aimed at reducing the bacterial population throughout the body and increasing overall immunity.
Who is at risk of contracting staph?
Anyone can develop a staph infection, although some groups of people are at greater risk, including newborns, women who are breastfeeding, and people with chronic medical conditions such as diabetes, cancer, vascular disease, and lung disease. Injecting drug users who have skin injuries. or disorders, intravenous catheters, surgical incisions, and people with a weakened immune system caused either by disease or as a result of immunoconverting drugs all have an increased risk of developing staph infections.
Certain groups of people are at greater risk of staph infection, such as newborns, diabetics, injection drug users, and surgical incision patients.
What do acne caused by staphylococcus look like?
It is impossible to independently determine what caused the rashes on the body and face. The reason to visit a doctor is any acne that appears suddenly, in large quantities and cannot be treated at home for more than a week.
Staphylococcal acne is dangerous because it contains pathogens. These rashes look like inflamed red bumps with purulent contents. If inflammation occurs in the deep layers of the epidermis, then the pus may not be visible, but the affected area causes sharp pain when pressed. Multiple rashes are sometimes accompanied by fever, vomiting and diarrhea. This picture requires an urgent visit to the doctor!
Staphylococci have chosen the area of the cheeks and chin, but they can also spread without hesitation on other parts of the body - from the scalp to the buttocks and legs. These rashes cannot be ignored. Without treatment, staphylococcus becomes the cause of complex acne, carbuncles, and furunculosis. More often, such problems overtake men. Inflamed areas tend to unite, forming a continuous purulent surface, which, after healing, leaves scars and age spots. These consequences are difficult to correct even in beauty salons.
The skin manifestations of a staph infection look like inflamed, purulent red pimples that form in the sebaceous ducts around the hair follicle. This disease is called folliculitis and requires mandatory medical intervention.
Staphylococcal rash on the face
If rashes occur on the face, the cause of the disorder must be sought in the body. Often the appearance of acne is caused by the influence of pathogens. One of them is staphylococcus on the face.
It appears when the bacteria is activated. Microorganisms united under the concept of staphylococcus can be different.
Particularly dangerous is the golden appearance, which leads to acne.
What is an infection?
Staphylococcus is a bacterium that enters the body due to infection. Its structure resembles a bunch of grapes.
Humanity knows about twenty types of staphylococcal microorganisms. But the most dangerous are:
- golden;
- saprophytic;
- epidermal.
After entering the body, the bacterium can settle on various surfaces. The most common areas of localization are the skin, mucous membranes of the nasopharynx, mouth, and genitals. In a calm state, staphylococcus poses no danger. It is part of the body's microflora. Therefore, the bacterium is considered opportunistic.
If conditions are created that are conducive to the proliferation of infection, then the process of division begins. In this case, various diseases can be diagnosed.
When staphylococcus is activated, acne may appear on the skin. The lesion occurs with the epidermal or golden form of the microorganism. In case of influence of the latter, serious skin diseases (boils, carbuncles) are observed.
The structure of Staphylococcus aureus
What you can and cannot do about acne with a staph infection
What you shouldn't do with any pimples is squeeze them. For staphylococcal acne, this rule becomes stricter. By releasing pus containing pathogenic microflora, you risk accelerating the spread of infection. If pimples have chosen the area of the nasolabial triangle, do not remove them yourself. This is due to the proximity of the brain, into which bacteria can penetrate.
It is recommended to postpone cosmetic procedures in the salon and at home until the resulting inflammations dry out and new ones stop appearing. Since any trauma to the rash with the release of its purulent contents leads to the spread of infection over the surface of the skin.
The prescribed treatment usually includes an integrated approach to reducing the number of pathogenic microorganisms. Special bacteriophages (bacteria-eating, literally) are taken orally to fight pathogens from the inside. Local therapy consists of treating the skin affected by rashes with ointments containing an antibiotic. The complexity of therapy is manifested in the fact that staphylococcus develops immunity to antibiotics. Therefore, it is not advisable to take one drug for more than seven days.
At the same time, procedures are carried out to strengthen the immune system:
- Restoration of intestinal microflora damaged by antibiotics, introduction of beneficial bacteria and correction of diet;
- Taking vitamin complexes that restore the normal functioning of organs and systems;
- Playing sports will be useful. If they are regular and do not bear a debilitating load on the body.
To relieve skin rashes caused by Staphylococcus aureus, in addition to lotions and ointments, it is permissible to use folk remedies:
- Aloe. Apply a piece of a leaf of this plant to the skin and fix it for an hour;
- Chamomile. Wipe the affected areas with a strong decoction three times a day;
- Garlic. After grinding, add water and let it brew. Wipe problem areas with the tincture using a cotton pad in the morning and before bed. Please note that prolonged contact of this vegetable with the skin will cause burns;
- Echinacea. Brew the roots of the plant together with burdock in the proportion of 2 tablespoons per 700 ml of boiling water. This decoction is taken orally in a glass three times a day.
If you suspect a staphylococcal infection on your face or body, consult your doctor for tests and medication. Pimples with purulent contents should not be squeezed out even during the treatment period. Avoid masks, peels and scrubs until complete recovery.
Summing up
According to reviews from some of my clients who tried to independently treat acne from staphylococcus, often even the usually effective broad-spectrum antibiotics, for example, Amoxiclav, do not give the expected result. Meanwhile, the bacteria mutate and become even stronger, provoking a new batch of rashes. That is why it is so important to get rid of them only under the supervision of a specialist.
If the antibiotic is chosen correctly and the patient follows all medical recommendations, significant improvements in skin condition become noticeable within a month. But it clears completely in 8-10 weeks. You may have had faster results. I would be grateful if you share the methods by which you managed to achieve them in the comments.
News MirTesen
Treatment
Treatment of diseases caused by Staphylococcus epidermidis or Staphylococcus aureus should be aimed at combating harmful microorganisms and increasing the body's protective functions. There are several groups of drugs that cope with dangerous rashes.
The patient requires antibiotic therapy. They can be local and systemic. If the inflammatory process is spread over large areas, then the use of systemic antibacterial drugs is required. The patient must undergo a sensitivity test, after which the doctor will select the medicine individually. Treatment is often carried out using:
They are able to stop the growth and reproduction of staphylococcus.
If the rash is localized, inflammation can be treated with local antibacterial drugs. These include ointments:
- Baneocin;
- Bactroban;
- Altargo;
- Methyluracil;
- Levomekol;
- Gentamicin.
Therapy is also carried out using staphylococcal bacteriophage. It is made with the addition of small particles of viruses that fight bacteria. They penetrate the microorganism and destroy it, and then die themselves.
The disease should be treated with the addition of staphylococcal toxoid. The drug helps rid the body of toxic substances produced by microorganisms. It is prescribed for extensive lesions and severe infection.
To strengthen the body's protective functions, you need to take multivitamins. They boost immunity and prevent infection from penetrating into the subcutaneous layers. Additionally, the use of adaptogens is indicated. These include ginseng tincture and Eleutherococcus.
In advanced forms of the disease, autohemotherapy may be required. The procedure involves taking the patient's venous blood and injecting it into the muscles.
During the treatment period, it is important to prevent the body from overheating. Baths and saunas are prohibited, as they increase the formation of pus and intensify the inflammatory process.
If staphylococcus becomes active and acne appears, you should definitely visit a doctor. Otherwise, microorganisms will affect different parts of the body. Due to the accumulation of pus, infection of the lymph, blood or bone tissue can occur. Therefore, therapy must be timely.
Facial skin lesions are inflammations due to infections, allergies, heat and even medications. The outer covering is resistant to most influences, but is still vulnerable to invaders such as viruses, bacteria, and fungi. Staphylococcus is the name of a group of bacteria that can cause a number of diseases, including infectious ones - staphylococcus on the face. The structure of most of these microorganisms resembles a purple bunch of grapes (Staphylococcus is translated from ancient Greek as grape seed).
Traditional recipes for treating infection
How to treat? Staphylococcus aureus can be eliminated using traditional methods of treatment. You can cope with the infection with the help of juices, decoctions, and ointments. Treatment can act both to eliminate the cause of the disease and to strengthen the immune system.
To prevent the occurrence of this disease in young children, it is necessary to follow the rules of hygiene.
It is necessary to treat children's toys with antiseptic drugs. As soon as the mother begins to add some fruits to the child’s diet, the child’s body will be replenished with microelements and vitamins.
When staphylococcus appears on the skin, it is recommended to use herbs such as calendula, chamomile, St. John's wort, yarrow . They are used in the form of lotions and compresses. It helps to eliminate the infection in the initial stages of infection by treating manifestations with Fukortsin or Zelenka .
Nutrition
Fruits and berries are very beneficial for the body. They contain a large amount of vitamins necessary for the body. For example, black currant, apricot, rose hips.
Black currants contain a large amount of vitamins. It is recommended to use them to prevent the occurrence of disease and enhance the protective properties of the body.
Eating apricot promotes faster regeneration of skin cells. It helps increase vitality and strengthen the immune system.
Rosehip is a real Klondike of vitamins. It is recommended to be consumed as tea. It can even be used in autumn and winter as a prevention and treatment of colds.
Phytotherapy
You can eliminate general malaise and fever by taking decoctions and infusions.
- St. John's wort infusion . You need to take 1 tablespoon of the herb and add hot boiled water. Leave to infuse for an hour. You can take half a glass before eating.
- Infusion of burdock and comfrey leaves . You need to take 25 grams of burdock and comfrey leaves, pour a glass of hot boiled water. Take a glass before eating.
Diseases caused by microorganisms
Staphylococcus, depending on the site of penetration, causes the following types of pustular skin lesions:
- Ostiofolliculitis;
- Folliculitis;
- Furunculosis;
- Carbuncle;
- Vulgar sycosis;
- Hidradenitis;
- Acne.
All types of diseases are characterized by the formation of acne of various forms. Coccus infection affects people regardless of gender and age.
Ostiofolliculitis
Inflammation of the sebaceous gland and the upper part of the hair follicle is called ostiofolliculitis. The microorganism causes redness in the area of the gland duct, which gradually transforms into a pustule, shaped like a cone and having a yellowish cap at the top. It is small in size (up to 5 mm). The hair shaft passes through the center of the cone-shaped formation. Once formed, the element does not grow and disappears on average after 3-4 days. If this condition is left untreated, the inflammation quickly spreads deeper, affecting the entire follicle and then folliculitis occurs. Such pustular formations can be localized in different areas or form entire clusters.
Ostiofolliculitis - inflammation of the sebaceous gland and the upper part of the hair follicle
Folliculitis
Unlike ostiofolliculitis, when only the upper part of the hair follicle is affected, with folliculitis the infection spreads to its deeper parts and provokes purulent inflammation, which manifests itself in significant pain. The disease begins, as in the first case, with the formation of a purulent pustule. After the pus resolves, an erosion forms, which then shrinks into a crust, and after it is rejected, a scar or stain remains. The surface element resolves on average in 5 days; if the formation is deep, the period increases to 10 days. Most often, folliculitis caused by a microorganism occurs in men, affecting the chin area and skin where hair is constantly removed when shaving. Untimely or incorrect treatment leads to complications such as boils, carbuncles, hidradenitis, and sycosis. The last disease is chronic inflammation of the follicles, manifested by frequent relapses.
Folliculitis is similar to furunculosis
Furunculosis
With furunculosis, not only the hair follicle is affected, but also the sebaceous glands and neighboring tissues. The pustule quickly changes in size - in 3 days a cone-shaped formation with a diameter of 5 cm can grow from the head of a safety pin. The boil is very painful, both with palpation and without impact on it. Only after it is opened and the pus is rejected does the pain subside. Boils on the face are considered the most painful and dangerous, since there is a high risk of infection entering the bloodstream and further into the brain. A characteristic feature of a boil that allows it to be distinguished from other ulcers is the presence of a necrotic core, which remains after the boil has opened and the pus has flowed out. Gradually, the rod self-rejects and the ulcer begins to heal. A boil always leaves behind a scar, which can be either sunken or convex.
Abscessing boil is one of the forms of complication of furunculosis
Carbuncle
When purulent inflammation affects several follicles at once, a carbuncle is diagnosed. The infection affects the bulbs, glands and adjacent fatty tissue, spreading both in breadth and depth. The affected area changes color, becoming bluish and even black. This is why the carbuncle got its name, which translates as “coal”. These boils are very painful. As it matures, pus mixed with blood is released from several holes at once. Necrotic rods, unlike boils, are very difficult to separate and take longer. After they are rejected, a deep ulcer with jagged edges is formed. After scarring, a scar remains.
Carbuncle affects several follicles at once and is diagnosed
Acne
Staphylococcus aureus can also cause chronic skin disease such as acne. In this case, it often creates conglomerates with other microorganisms and especially with acne bacteria. This condition is characterized by excessive production of sebum and changes in its composition, which entails the occurrence of hyperkeratosis. The result of such changes is that a plug is formed at the mouths of the hair follicles, where the ducts of the sebaceous glands exit. It consists of sebum and desquamated epidermal cells, which, due to the large number, are not able to come out in time. These plugs are called comedones. Under the influence of various factors, comedones are transformed into various forms of acne.
Most often, you can find such a common pathogen as staphylococcus on a person’s face. It has a detrimental effect on the human body. Cutaneous staphylococcus is a collective name. This group includes many distributors of serious diseases. But Staphylococcus aureus poses a significant danger. It can lead to most diseases.
The most common skin diseases are:
- phlegmon;
- furunculosis;
- felon;
- carbunculosis;
- pyoderma;
- erysipelas and others.
Staphylococcus is quite resistant and difficult to fight. It retains its dangerous properties for six months even when dried. It is useless to influence the microbe with ultraviolet rays; there is no point in freezing it. He is able to protect himself with the help of a special substance. At the same time, it produces toxins that damage all layers of the skin. He is not afraid of leukocytes and antibiotics. Therefore, staphylococcus is difficult to cure. It is considered the most common among skin microbes. Staphylococcal infection can affect every organism. However, the disease progresses differently for everyone. This is facilitated by the causes of the disease and the characteristics of the immune system. It happens that a subcutaneous microbe lives on the skin of a person’s face for years without causing inflammation.
Symptoms depend on the location and resistance of the diseased body’s defenses. But there are times when the microbe manifests itself with non-standard symptoms.
This creates significant difficulties in making a diagnosis. When determining it, the doctor is guided by knowledge of such diseases as:
- Phlegmon. The disease is characterized by swelling, redness of the inflamed area of the skin, fever and general malaise. It can cause a severe inflammatory process, as a result of which tissue will die.
- Furunculosis. This is a type of staphylococcus on the face. The disease is very common. Inflammation occurs anywhere in the body. The symptoms of the disease depend on the area where the microbe is introduced. Redness occurs, with necrosis (tissue death) in the center. The necrotic tissue slowly begins to die, and dark green pus flows from the wound. After some time, the disease may appear again. Boils on the face and neck are especially dangerous. The inflammatory process can move to the lining of the brain.
- Felon. Cutaneous staphylococcus causes disease of the periungual fold. The affected nail plate and the surrounding skin become hot and red. A slight pain appears. When the epidermis is opened, pus will flow out. Inflammation can move to neighboring fingers and affect the deep layers of the skin.
- Pyoderma. It is observed more often in infants. The reason is poor child care. Staphylococcus covers the top layer of the baby's delicate skin. Small blisters filled with pus appear. When scratching them, the liquid flows out and spreads to other areas of the skin and subcutaneous integument. Body temperature rises, mild malaise appears.
- Erysipelas. A very serious illness. Localization area: lower limbs. They turn red, become hot, and minor rashes appear. The patient begins to feel sick, the temperature rises to 39 degrees. The condition is always serious.
Staphylococcus aureus is one of the most common infectious agents. Its main symptoms are inflammation of the facial skin and abscesses.
Sycosis. Rashes are observed on the chin, as well as in the upper lip area. The skin of the face takes on a bluish color and thickens. Sycosis can be treated over a long period of time and may recur after treatment.
Carbunculosis. It is also a type of staphylococcus. The skin on the face swells, thickens, becomes dark red, pustules and necrosis appear, and the discharge contains blood clots. After exfoliation of the stratum corneum, ulcers may appear on the skin, and after they heal, scars may appear. The patient is hospitalized. The surgeon opens the carbuncles and applies a disinfecting bandage.
Impetigo. On the face, impetigo manifests itself in the form of pustules and pustular (blistering) rash. Formations filled with pus appear near the mouth and nose.
Pathology includes erosion of the epidermis and pustular crusts. This disease is contagious and causes severe pain. It most often affects young people and those who ignore hygiene rules.
Reasons for pathogen activity
The endocrine and nervous systems are responsible for the functioning of the sebaceous and sweat glands and the acidity of the skin. When the pH of secretory secretions is at the level of 3.5-6.7, conditions are created that are detrimental to the growth and reproduction of pathogenic bacteria, but if this indicator shifts to an alkaline environment, conditions become favorable for pathogenic flora. Such changes occur due to disruption of the endocrine system and disruption of hormonal balance. Also, a decisive role in the development of infection is played by disruption of the skin due to mechanical or chemical injuries (scratching, abrasions, cuts, burns, insect bites).
Causes of acne on the face
When staphylococcus settles on the skin, acne occurs due to both external and internal reasons:
- physical and chemical irritants (shaving, friction against clothing, etc.);
- skin contamination;
- unhealthy diet, especially monotonous, exhausting diets and lack of vitamins;
- any infectious, chronic diseases, exposure to stress have a depressing effect on the immune system;
- frequent ARVI;
- increased sweating (hyperhidrosis);
- overheating, leading to increased secretion of the sebaceous glands;
- diseases of the endocrine system, especially diabetes.
This is not a complete list of reasons that weaken the antibacterial and protective function of the skin.