Follicular keratosis is a common and fairly harmless skin disease that develops due to a disruption in the keratinization process of hair follicles. It is characterized by the appearance of small, small, rough spots or bumps on the skin. They are also called "goose bumps". This process is accompanied by a feeling of tightness and dryness. Most often, such pathological elements form on the forearms, thighs, buttocks, and less often on the face. Moisturizing cosmetics and exfoliants are used to treat keratosis pilaris. But it is equally important to follow a proper diet. It is better to entrust the choice of cosmetics to a dermatologist or cosmetologist.
…
Keratosis follicularis is the defining clinical and histological feature of certain symptomatic skin lesions or a group of dermatological diseases called “follicular keratoses”, accompanied by hyperkeratosis (excessive keratinization of the epithelium) and blockage of hair follicles.
What kind of disease is keratosis pilaris?
Follicular keratosis is a common dermatological disease associated with disruption of the normal processes in the upper layers of the epidermis.
It is seasonal in nature, since its symptoms most often appear in winter, which most experts associate with vitamin D deficiency in the cold season.
Signs of the disease often appear in childhood and are expressed only in external manifestations. In most cases, after puberty, symptoms go away on their own without any additional therapy.
Differential diagnosis
Differential diagnosis is carried out with the following diseases:
- Pityriasis pilaris - elements of the rash are located on the scalp, it looks like red keratinized nodules, in the center of which there is a hair. The skin feels hard and excessively rough to the touch. This form of pathology most often develops at 2-4 years of age, and already begins to subside in adolescence or youth.
- Palmoplantar, follicular punctate - the disease manifests itself only in the area of the soles and palms. The cause is usually previous infections.
- Flegel's lenticular keratosis - brown and red rash elements are formed, it is most often observed in the arm area. If you remove the crust, pinpoint bleeding appears.
- Morrow-Brook's keratosis or inverted - begins to manifest as dry skin, then nodules with hairs or horny spines appear. A rash appears on the soles and palms, in the area of skin folds, near the nails. During the cold season the condition improves.
- Darier-White disease is a keratosis vegetans, at first the elements of the rash differ little in color from healthy tissue, but then become brown. The areas of the back, chest, and head are most often affected.
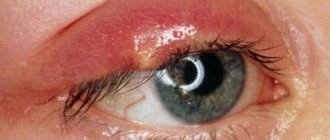
- Superciliary ulerythema - this form is characterized by the appearance of symmetrical nodules above the eyebrows. The disease causes hair loss.
Superciliary ulerythema
Causes of the disease
Follicular keratosis is a congenital dermatological disease, but the exact causes of its occurrence and development in children have not yet been established.
It is known that the external manifestations of this form of keratosis occur under the influence of the following factors:
- Deficiency of vitamins A, C or D in the body , most often it is caused by seasonal factors or lack of a balanced diet;
- Adverse reactions after taking potent pharmacological drugs , especially a similar risk occurs with long-term use of hormonal drugs;
- Mental and emotional stress , frequent experiences of stressful situations;
- Metabolic disorders , endocrine pathologies, diabetes mellitus;
- Chemical burns and systematically applied mechanical effects to the local area;
- Long-term exposure to various types of radiation , including X-rays;
- Autoimmune pathologies of a local nature.
- Fungal infections caused by various species.
Children suffering from various chronic diseases, most often eczema or asthma, are at risk - they are much more likely to develop keratosis pilaris.
Features of the disease
Skin cells are constantly renewed: the upper keratinized ones are exfoliated, their place is taken by younger ones. New cells are born in the basal layer - the base of the epidermis (the uppermost part of the skin). As cells grow, they become increasingly filled with the protein keratin, which leads to their keratinization. The process of skin renewal occurs unnoticed by humans. If everything is normal, it looks smooth and uniform due to the constant supply of nutrients and moisture.
Follicular keratosis is a group of skin diseases associated with an increased supply of keratin into its cells. Keratization occurs so quickly that they do not have time to mature, and the thickness of the stratum corneum increases. The accumulation of rough epithelium leads to blockage of individual hair follicles. As a result, the growing hairs cannot come out of them and curl into a knot. Horny bumps form on the skin. It becomes rough like sandpaper.
This skin defect can appear in early childhood, very often occurs in adolescents and often disappears on its own after the onset of puberty (by about 20 years). However, this does not always happen. For some people, the problem remains for life and does not cause any particular trouble.
Signs of keratosis most often occur during the cold season.
The disease is not dangerous and requires mandatory treatment. But sometimes complications arise if the affected skin is rubbed with clothes, combed, and becomes inflamed due to staphylococci and streptococci entering the wound. In place of keratotic tubercles, ulcers and boils can form. Chronic inflammation of the follicles and acne may develop.
Most often, the skin of the arms, legs, and buttocks is affected. Sometimes foci of keratosis pilaris can be seen on the face, scalp, elbows and knees, on the back between the shoulder blades, and on the shoulders.
Types and classifications
In total, there are two main forms of keratosis pilaris:
- The acquired form is often found among older children; it can develop against the background of fungal infections, syphilis, cutaneous tuberculosis, scleroderma, lupus erythematosus, as well as due to exposure to occupational factors of a mechanical or chemical nature. Acquired keratosis can appear as a single lesion or multiple lesions. It is often accompanied by acne, which can cause a secondary infection and the development of acute inflammation;
- The congenital form is caused by genetic factors; unlike acquired keratosis pilaris, it is virtually incurable; only symptomatic therapy is practiced to eliminate the main external manifestations. Symptoms of the disease occur in children under the influence of external factors or when the immune system deteriorates. Sometimes keratosis does not manifest itself in any way in childhood and begins to develop in adulthood.
Congenital keratosis pilaris has its own classification, which includes three types:
- Papular varieties of keratosis - have less pronounced external manifestations, these include diseases such as Devergie's disease, lenticular hyperkeratosis and lichen pilaris. In children over 2-3 years of age, lichen pilaris most often occurs; it occurs more often in girls than in boys; in adolescence or youth, the disease usually goes away on its own;
- Atrophying types of keratosis - characterized by extremely slow progression or its absence; A characteristic feature of the disease is local atrophy of the skin on the affected areas of the body. This type includes Siemens keratosis, superciliary erythema, ulerythema and other diseases;
- Vegetative types of keratosis are also found in childhood, but such pathologies are more rare. The most common type is Darier-White disease, which affects not only the skin, but also the nail plates. The main danger lies in the frequent occurrence of secondary infections and complications due to exposure to ultraviolet rays.
Follicular keratosis (parafollicular keratosis, Kirle disease - CD) is a rare skin disease from the group of perforating dermatoses, which is based on a violation of keratinization with intradermal invagination of the epidermis [1] (synonyms: follicular and parafollicular hyperkeratosis, penetrating the skin, follicular and parafollicular hyperkeratosis with penetration into the skin (hyperkeratosis follicularis et parafollicularis in cutem penetrans), penetrating hyperkeratosis [2, 3]).
The disease was first described in 1916 by the Austrian dermatologist J. Kyrle, who observed this dermatosis in a patient with diabetes mellitus [3-5].
Epidemiology.
The disease is rare. The age of patients is 20-70 years. Women get sick more often, children - very rarely. Concomitant diseases: often - diabetes mellitus and chronic renal failure, less often - heart failure, hypothyroidism, type II hyperlipoproteinemia (increased blood levels of cholesterol and triglycerides) [1, 3-6].
Etiology and pathogenesis
have not been fully studied. The previously assumed role of a viral or bacterial infection, a violation of vitamin A metabolism in the development of this dermatosis is only of historical interest [4]. A certain significance in the development of the disease, in addition to impaired carbohydrate metabolism, is attributed to liver damage (chronic hepatitis) with the development of secondary vitamin A deficiency [5].
The genetic predisposition to the development of CD has not been conclusively proven, although cases of the disease among relatives in the same family with consanguinity (first-degree relatives) have been described [1, 3-5].
According to the original definition by J. Kirle [7], this is a disease in which an atypical clone of keratinocytes penetrates through the epidermis into the dermis. It is believed that the basis of the pathological process is a violation of keratinization, differentiation and keratinization of keratinocytes (formation of dyskeratotic foci and acceleration of the keratinization process). This leads to the formation of keratotic plugs with areas of parakeratosis. Keratification begins already at the border of the epidermis and dermis. The rate of differentiation and keratinization exceeds the rate of cell proliferation, therefore the parakeratotic cone partially penetrates deeper into the damaged epidermis and causes its perforation into the dermis [1, 3-6].
Unified classification
There are no follicular keratoses. Among the independent nosological forms, papular, atrophying and vegetative follicular keratoses are distinguished [8]. A number of authors [4, 6] draw attention to the similarity of CD with lenticular persistent hyperkeratosis of Flegel and consider the latter as a variant of CD, although the clinical manifestations differ. Other authors [5, 8] classify CD as vegetative follicular keratoses, and persistent keratosis follicularis (Flegel's disease) as papular.
The concept of reactive perforative keratinization disorder against the background of kidney, liver, and diabetes mellitus is considered. A concept has emerged - perforating skin diseases; it includes a group of diseases in which the elimination of altered skin components occurs through the epidermis (a process called transepidermal elimination). Some authors dispute CD as an independent nosological entity [7].
In the International Classification of Diseases, 10th revision, in class XII (diseases of the skin and subcutaneous tissue), heading L87 is allocated - transepidermal perforated changes, in which CD is assigned a separate subheading L87.0.
Pathomorphology
very characteristic and has diagnostic significance. The recesses of the epidermis and the dilated openings of the hair follicles are filled with hyperkeratotic plugs. Under the plugs in the epidermis, the growth of the granular layer is pronounced, and in places where there is no hypergranulosis, there is parakeratosis, penetrating the entire epidermis to the dermis. Subsequently, thinning of the epidermis occurs and penetration of horny masses into the dermis with the formation of inflammatory infiltrates such as granulomas from lymphocytes, leukocytes, histiocytes and giant cells of foreign bodies in the dermis. Death of the sebaceous glands in the area of the affected follicles, degeneration of collagen fibers, and hyperelastosis are observed [1, 2, 5, 6].
Clinical picture.
The onset of the disease is gradual, new rashes appear as old elements disappear. Follicular or parafollicular papules are characteristic, first the color of healthy skin, and subsequently grayish or brownish-red in color, with a diameter from a pinhead to 1 cm. In the center of the elements there is a horny plug, when removed, a crater-shaped depression is formed. Papules tend to grow peripherally and merge with the formation of dry polycyclic plaques covered with layers of scales and crusts. The consistency is dense, the surface is uneven, warty. Fresh rashes are accompanied by mild itching (more often in patients with diabetes) or do not bother the patient. Older, larger lesions are painful, especially when pressed. In the places of calculations there is a linear arrangement, which indicates the possibility of the occurrence of the Koebner phenomenon. A secondary infection may occur. Localization of rashes - extensor surfaces of the limbs, torso, buttocks. The mucous membranes are not affected [1-6]. Rashes in the mouth, palms, soles, and genitals are rare [4].
Flow
CD is chronic, relapsing. The disease is difficult to treat. The prognosis largely depends on the underlying disease.
Diagnostics
based on anamnesis, clinical and histological picture of the disease. Differential diagnosis of CD should be carried out with Devergy's lichen pilaris, Darier's follicular dyskeratosis, Mibelli's porokeratosis, transepidermal perforated skin changes (perforating creeping/serpiginous elastosis, reactive perforating collagenosis), Flegel's disease [8].
Flegel's disease
(hyperkeratosis lenticularis perstans), like CD, is a rare form of keratosis pilaris. It is believed that the basis of this disease is a hereditarily determined (autosomal dominant type) pathology of keratinization, expressed in a violation of the synthesis of keratin 55K, the content of which is sharply reduced in the lesions of Flegel's disease, while in normal skin this type of keratin dominates. Histologically, thinning of the epidermis, follicular orthokeratosis with foci of parakeratosis, and spongiosis in places are revealed; a band-like lymphocytic (mainly T-helper) infiltrate is expressed in the dermis. The previously attached great importance in the pathogenesis of dermatosis to the absence or disruption of the structure of Odland bodies [4] is now being questioned. Odland's granules appear in the upper rows of the spinous layer in keratinocytes, occupy a peripheral position and release their contents by exocytosis into the intercellular space, where it takes on a lamellar structure (intercellular cement) - a component of normal keratinization. Unlike CD, this dermatosis appears more often in adolescence and middle age, and is characterized by the formation of disseminated, smaller (1–5 mm) and more superficially occurring horny papules (without a tendency to form plaques). In CD there is no impairment of keratin 55K [6].
Treatment:
vitamin A, long-term aevit, retinoids (neotigazone, etretinate, acitretin at the rate of 0.5 mg/kg per day). Externally - keratolytic ointments, 2% sulfur salicylic ointment, retinoid cream, 0.1% tigazone cream, 5% fluorouracil cream (for an area of no more than 500 cm2 at a time), electro-, cryo- and laser destruction (carbon dioxide laser) of individual lesions, ultraviolet irradiation . The effect of treatment is temporary. After removal of the horny plug, an atrophic, unevenly pigmented scar remains; relapse may occur nearby. Correction of visceral pathology is necessary [3-6].
We present our own clinical observation.
Patient B., 57 years old, retired (military orchestra musician), was admitted to the purulent surgery department on September 13, 2010 for surgical treatment for osteomyelitis of the left foot. The attending physician prescribed a consultation with a dermatologist due to skin rashes.
Anamnesis.
The first rash on the skin of the front chest appeared about 20 years ago. The rashes practically did not bother me; minor itching was rarely noted; I was more “worried” about the cosmetic aspect. Diagnoses were made: dermatitis, xerosis, keratosis. There was no effect from the recommended salicylic ointment, creams with chamomile, string, or taking vitamin A orally, which was explained by the “peculiar structure of the patient’s skin.” According to the patient, the best effect was noted from the use of cindol (“the chatter dries well and peels off the plugs” on the skin). The rashes did not disappear completely, no seasonality was noted.
Since 1995, he has been suffering from type 2 diabetes mellitus and has been taking oral hypoglycemic drugs (diabetes). In 2009, he received inpatient treatment at his place of residence for diabetic foot syndrome, a purulent-necrotic wound on the left foot; healing by secondary intention. Since the summer of 2010, the rashes have increased significantly, which the patient associated with extreme heat. In July, I received a puncture wound in my left foot (I stepped on a nail at the dacha), which did not heal for a long time, and my blood sugar level increased. Due to worsening severe pain, the patient was hospitalized.
Skin status.
On the skin of the body there are multiple follicular and parafollicular papules of a red-brown color, in places grouped into small plaques covered with dense scales. In the center of the papules there are horny plugs. Where the plugs have come off, there are crater-shaped depressions filled with the previously applied zindol. In place of the resolved elements there are small scars. On palpation, the rashes are dense, the skin resembles a “grater”, and is moist. Several intradermal nevi are round, dome-shaped, soft in consistency, and brown in color (Figure a-c).
Figure 1. Patient B., 57 years old: manifestations of CD.
The patient suffers from diabetes mellitus and diabetic nephropathy. a—c—many pinkish-red and grayish-colored papules and nodules with horny plugs. In those places where the patient scratched the skin, the elements of the rash are located linearly (Koebner's symptom). Several intradermal nevi. Skin of the head, limbs, visible mucous membranes without rashes, physiological coloring. Results of special examinations.
Clinical blood test: hemoglobin - 124 g/l, erythrocytes - 4.0 1012/l, leukocytes - 6.7 109/l (upon admission 12.8 109/l), neutrophils - 67%, segmented - 65 %, band - 2%, eosinophils - 3%, lymphocytes - 23%, monocytes - 9%, erythrocyte sedimentation rate - 35 mm/h (on admission 53 mm/h). ASTL-0 titer and rheumatoid factor were not detected. PSA -10 mg/l. Urinalysis upon admission: specific gravity - 1020, protein - 0.132‰, sugar - 0.3 mg/l, acetone - no, leukocytes - 3-5 in the field of view, erythrocytes - 4-5 in the field of view, cylinders - 4 in drug. Upon discharge, urine analysis was normal.
Radiography
chest organs - without pathology. X-rays of the left foot show complete destruction of the head of the third metatarsal bone, partial destruction of the second metatarsal joint. Electrocardiogram - sinus rhythm, heart rate 76 per minute; changes in the myocardium; phenomenon of early ventricular repolarization.
Endocrinologist.
Diabetes mellitus type 2, severe, insulin-requiring, decompensated. Diabetic angiopathy of the vessels of the lower extremities. Diabetic nephropathy. CRF-0.
Ophthalmologist.
Proliferative diabetic retinopathy. Initial cataract of the right eye.
Surgeon.
Flaccid granulating wounds of the plantar surface of the left foot. Osteomyelitis of the II-III metatarsal bones of the left foot.
Dermatologist.
Keratosis follicular and parafollicular, penetrating (KK). Intradermal nevi. There are no contraindications to surgical treatment.
On September 20, 2010, the patient underwent transmetatarsal resection of the head of the third metatarsal bone. Amputation of the third toe of the left foot. Received antibacterial therapy, humulin, lantus; Dressings with dimexide, water-soluble ointments, and physiotherapy were carried out. The skin of the body was treated with cindol once a day.
Recommendations for discharge.
Observation by an endocrinologist or surgeon at the place of residence; humulin 18 units 3 times a day before the main meal, lantus at 22:00 16 units. Dressing of residual wounds with betadine ointment. Laser coagulation of the retina after normalization of sugars in a separate hospitalization, then see a dermatologist.
Discussion
Every dermatologist encounters strange patients. This is especially true for rare dermatoses, some of which a doctor may encounter only once during his practice. “It’s better to see once than to hear a hundred times,” says Russian folk wisdom. “The main tool of a dermatologist is his eyes” [3].
The fact that our patient had severe symptoms of hyperkeratosis of the trunk was obvious, but we had not encountered either CD or Flegel’s disease before. Only on the basis of anamnestic data, a characteristic clinical picture and information obtained from literature sources (the patient refused the proposed skin biopsy) was the final diagnosis made. Our patient suffers from diabetes mellitus and diabetic nephropathy. If the recommended screening of all patients with hyperkeratoses to detect latent diabetes [4] had been done earlier, the diagnoses might have been made earlier. This is precisely the purpose of this publication.
Symptoms and locations
With keratosis pilaris in children, the following symptoms of the disease may occur:
- Redness and changes in the structure of the skin , the appearance of lumpiness in the affected areas. The diameter of the resulting tubercles usually does not exceed 2-3 mm, but with exacerbation of keratosis it can temporarily increase to 5 mm;
- The appearance of small rashes, small pimples in the lesions;
- Mild itching caused by peeling of the skin, in some cases this symptom is completely absent;
- Clogging of follicles with exfoliated skin particles , against the background of this symptom, severe inflammation may develop.
The appearance of other symptoms usually indicates that keratosis pilaris is accompanied by other diseases, which requires diagnosis and the prescription of complex therapy.
If left untreated, the area of the lesions may increase over time.
Lesions are usually localized in the following areas of the body:
- Face, mainly cheeks;
- Shoulders;
- Inner and outer thighs;
- Breast;
- The area of the back between the shoulder blades;
- Forearms;
- Hands;
- Feet.
In the back, hands and feet, lesions are localized in the most severe cases, when, due to lack of treatment, keratosis continues to progress.
Question answer
Since keratosis pilaris often appears in men, especially young men, many are interested in whether they are recruited into the army with such a diagnosis. Definitely yes, since this disease is safe both for the patient himself and for others. The exception would be cases when a young person suffers from severe itching and the affected area is constantly increasing.
On thematic forums you can often find questions about whether it is possible to get a tattoo with keratosis. Experts say that this disease is a clear contraindication to such actions. This can cause serious complications.
This is not a fatal pathology. But, nevertheless, if nothing is done, it can progress and bring discomfort to a person (for example, severe itching).
What does keratosis pilaris look like in children?
Keratosis pilaris, which occurs in children, looks like a small nodular rash, which is called “goose bumps.”
It has the following features:
- Nodular formations are numerous, but their size usually does not exceed a few millimeters;
- The nodules have a rough surface and a dense structure;
- Redness and itching occur during periods of exacerbation of keratosis; during remission, physical discomfort is completely absent.
Keratosis increases the tendency for the skin to dry out. If the skin on the feet and palms is very dry, children are diagnosed with a hereditary form of the pathology.
Photo of what keratosis pilaris looks like in children:
Preventive measures
It is unlikely that it will be possible to prevent the appearance of keratosis pilaris, but it is quite possible to reduce its symptoms and avoid exacerbation. It is enough to follow a number of rules:
- protect the skin from prolonged exposure to ultraviolet radiation;
- during the cold period, lubricate the skin with a rich cream every day before going outside;
- switch to proper nutrition;
- in spring and autumn, take a multivitamin complex;
- wear clothes exclusively from natural materials;
- Avoid contact with allergens if possible;
- use mild detergents.
To prevent keratosis from causing physical discomfort, it is important to follow all medical prescriptions and listen to the advice of professional cosmetologists. You also need to follow simple rules of personal hygiene.
Are there possible complications and consequences?
Follicular keratosis, not accompanied by other diseases, does not pose any threat to the child’s health. Pathology only causes psychological discomfort due to its external manifestations.
The disease proceeds without complications and does not have a negative effect on the child’s internal organs.
The risk lies in scratching the affected areas and mechanical damage to the skin when itching occurs. Through the resulting wounds, a bacterial infection can occur, which will lead to the formation of foci of purulent inflammation of varying severity.
Diagnostics
An experienced dermatologist can usually determine the type of disease by examining the patient based on the nature of changes in the skin, as well as the presence of accompanying symptoms. In case of doubt, the diagnosis can be confirmed using histological analysis of scrapings taken from the affected area of the skin.
When examining a patient, it is necessary to exclude the presence of diseases with similar symptoms, such as follicular psoriasis, lupus erythematosus, seborrheic keratosis, lichen planus.
Note: If the keratosis lesions are small, are not an aesthetic problem and do not cause discomfort, then treatment is not necessary. However, every person who is faced with manifestations of keratosis pilaris should know that it is most often possible to get rid of skin defects using fairly simple means.
Diagnosis and which doctor should I contact?
Despite the safety of keratosis pilaris, it is mandatory to seek medical help, since independent diagnosis is impossible, and self-medication can aggravate the situation.
If symptoms of keratosis appear in children, you should contact the following specialists:
- Dermatologist - will carry out a set of diagnostic measures to confirm the diagnosis and determine further actions;
- A pediatrician can help if you can’t see a dermatologist. He will conduct an initial examination, prescribe tests and, if necessary, write a referral to a highly specialized doctor.
Diagnostics are necessary to exclude other diseases with similar symptoms, primarily this concerns Darier's disease and keratoderma.
Two main methods are practiced:
- Visual inspection of the affected areas on the child’s body;
- Carrying out histological studies to determine the nature of the rash.
Symptoms of follicular hyperkeratosis
One of the first signs of the disease is the appearance of lumps of rough skin, after which it becomes rough, like sandpaper. In appearance, it resembles the “goose bumps” that appear in a person during a chill. Therefore, people call this disease “crow’s feet”, and sometimes “pimples”.
The tubercles can be located in one place in a small area, but they can also be numerous, scattered throughout the body. Sometimes a hair comes out of them. As a rule, the affected skin does not itch.
Touching skin covered with plaques may be painful. The rash may have a red or brown tint. The size of the tubercles is 1-3 mm in diameter, they may alternate with pimples, as well as the appearance of wen and scars.
Signs of follicular hyperkeratosis of some types
Jeveri's disease. The hard tubercles protruding above the surface of the skin have a conical shape. Their color is usually reddish or orange. Initially, individual plaques with several keratinized spots appear, and then they merge. Rashes appear on the head and itch. Pimples move to the body, face, phalanges of the fingers. The shape of your nails may change. The affected skin peels off. This disease is classified as chronic inflammatory.
Lenticular keratosis (Flegel's hyperkeratosis). With this disease, single, sparsely located red-brown papules appear on the feet, legs, and upper limbs. Mild itching occurs. The disease is hereditary. Appears after 40-50 years.
Superciliary ulerythema. Most often, this type of keratosis pilaris occurs in children and adolescents. There is keratinization of the skin and follicles above the eyebrows, which gradually spreads to the forehead, cheeks, and chin. The cheeks become red and scars appear. Eyebrow hair falls out. The disease often occurs against the background of pathologies of physical and mental development.
Pityriasis pilaris (pityriasis versicolor, Devergie's disease). The skin becomes covered with small conical papules that have a grayish-white crust, from under which a hair emerges. Rough plaques form on the body, surrounded by red, inflamed skin. As they grow, keratosis spots cover a large area and are found on almost any part of the body (especially on the head, neck, soles and palms, and elbows). The affected skin itches slightly, tightens, and pain is felt.
Palmoplantar keratosis. This is the name given to a group of hereditary diseases in which smooth, thick plates of yellow skin appear on the feet or palms. They have clear boundaries and feel moist to the touch. The disease is hereditary, the first signs appear in early childhood. The lesions are fully formed by 15-20 years. May occur on the knees and elbows. Sometimes painful cracks appear (usually on the heels).
Darier's disease. A cream-colored rash appears on the face, scalp, chest, back, and in the folds of the skin, which is gradually covered with a grayish layer of crusts. Keratosis pilaris spots resemble a cluster of warts. Most often the disease occurs in children and adolescents.
Treatment methods
In most cases, keratosis pilaris in children does not require special treatment, since it is only an aesthetic defect.
During periods of exacerbation, symptomatic therapy is used to suppress the resulting inflammation and itching, leading to scratching of the affected areas of the body.
With normal functioning of the endocrine system, manifestations of keratosis usually go away on their own upon reaching the age of 15-17 years.
To get rid of the main symptoms of keratosis pilaris, the following treatment methods are used:
- Completing a course of drug therapy - prescribed for the treatment of acquired forms of keratosis;
- Undergoing physiotherapeutic procedures - prescribed as an addition to the main therapy in the treatment of acquired keratosis;
- Use of traditional medicine methods - herbal remedies are used for symptomatic therapy; in childhood, permission from a pediatrician is required;
- The use of children's cosmetics to moisturize the skin and nourish all layers of the epidermis;
- Taking preventative measures to prevent the progression of keratoses and reduce the risk of relapses.
How to cope with illness at home
At home, keratosis pilaris can be cured using various homemade masks and peels. After such procedures, any nourishing cream must be applied.
To help smooth out skin texture, start with a daily cleansing routine. This could include dry brushing before showering or using an exfoliator that contains glycolic or salicylic acid.
While skin feels damp after swimming, immediately apply a moisturizer containing lactic acid, glycolic acid, salicylic acid, ceramides, hyaluronic acid, or a combination of these.
Dermatologist Alicia Zalka
It is recommended to systematically scrub the skin, but without fanaticism - twice a week is enough. Otherwise, irritation may occur.
Along with the use of emollient creams and ointments, you can use folk remedies:
- Aloe - compresses are prepared from it. To do this, succulent leaves are plucked from plants older than 5 years. They are washed and frozen. Then they are cut into thin strips and applied to problem areas with fixation with an adhesive plaster or film and bandage. Leave the compress on all night. The procedure is repeated every other day.
- Propolis - used in the form of compresses. The propolis composition is applied in a thin layer to the affected areas, covered with cling film on top and tied with a bandage.
- Potatoes - application similar to previous options. Unpeeled tubers are finely grated and the resulting pulp is placed in gauze, then applied to the skin with keratosis. After 2 hours, the compress is removed.
It is important to first exclude the cause, otherwise local treatment will not bring the desired result.
Drug treatment
To reduce the severity of symptoms of keratosis pilaris in children, the following medications are used:
- Vitrum is a children's vitamin complex for oral administration; the large amount of retinol it contains is of particular value in the treatment of keratosis. It has a general positive effect on the epidermis and all its derivatives, improves skin condition and helps prevent dryness, which is one of the symptoms of pathology. Admission for preventive purposes is recommended 2 times a year in agreement with the pediatrician, which will reduce the risk of recurrence of keratosis. The Vitrum vitamin line includes several complexes for children. The duration of the course is 1-2 months. The average cost is 300 rubles ;
- Elidel - can be used to treat children from the age of 3 months; individual dosage adjustment is not required. The drug is intended for the treatment of eczema and atopic dermatitis, but they are often prescribed for keratosis pilaris, if the disease is acute or accompanied by severe inflammation. Release form – 1% cream. Apply to affected areas 2 times a day. The drug should be used until the symptoms of keratosis disappear, but the maximum duration of the course should not exceed 40 days. The cost of a 15 gram tube is about 1000 rubles ;
- Salicylic acid - used for local treatment of areas affected by keratosis. It can be used to treat children older than 1 month. The daily dosage in childhood is 1 ml, the duration of the course should not exceed 5-7 days. The product softens diseased areas of the skin and helps get rid of excess stratum corneum. It must be taken into account that salicylic acid can accelerate the absorption of the active components of other drugs for topical use included in therapy for the treatment of keratosis pilaris. You can purchase the drug at a price of 15 to 40 rubles ;
- Protopic is an ointment for external use based on tacrolimus monohydrate; the drug has immunomodulatory properties and the ability to eliminate acute inflammation. The drug is prescribed for severe keratosis. Ointment 0.03% can be used for children over 2 years of age, and ointment 0.1% can be used to treat adolescents over 16 years of age if they still have signs of keratosis. Apply a thin layer up to 2 times a day. The duration of the course is 1 week, the maximum duration of treatment for severe symptoms is 2 weeks. The cost ranges from 650 to 1500 rubles , depending on the volume of the tube.
Vitrum Elidel Salicylic acid Protopic
Corticosteroids are almost never prescribed for the treatment of keratosis pilaris at an early age. Their use is possible in adolescence.
If, due to other health problems, the disease continued to progress and became more severe. The use of any hormonal ointments is possible only by the decision of the attending physician.
Etiology and pathogenesis of keratosis pilaris
Some authors propose to subdivide follicular keratosis of the skin, depending on the etiological (causal) factor, into congenital and acquired. The latter, in turn, is divided into primary, which occurs on the skin that has not previously been changed by inflammatory or any other pathological process, and secondary. At the same time, these authors warn that such a difference is purely conditional, since the proliferation of the layer of horny cells without previous changes in the skin area is only apparent and practically impossible.
The principle of the mechanism of development of pathology
Under normal physiological conditions, epithelial cells are formed in the basal layer as a result of the division of germ cells of keratinocytes. Subsequently, young cells no longer divide. They undergo differentiation and growth, gradually lose their nucleus and organelles and are filled with the protein keratin - keratinization, or keratinization.
Growing young cells displace older ones lying above them and take the place of the latter. The full life cycle of the normally occurring process of “soft” keratinization is two days and ends with a barely noticeable exfoliation of one layer of the horny epithelium. This process, which forces newly formed cells to move to the surface of the skin, also promotes the movement of substances that penetrate the epidermis.
Due to the influence of various causative factors (acquired or genetically determined), a disruption of the keratinization processes of the epithelium occurs, accompanied by incomplete maturation and delayed rejection of the cells of the stratum corneum, an increase in its thickness and the closure of the lumen of the hair follicles.
Folk remedies for treatment
Below are the safest traditional medicine techniques for suppressing the symptoms of keratosis, which can be practiced in childhood.
The most effective of them:
- Compresses with aloe leaves are a completely safe way to eliminate problems associated with keratosis pilaris in children. You will need to take the leaves of an adult plant, wash them, cut them into pieces and keep them in the refrigerator for 2-3 hours, but not in the freezer. After this, the leaves are applied to areas of the body with skin lesions, their position is fixed using cling film and gauze bandages. You can remove the compress after 12 hours, the procedure is repeated every 2 days until the main symptoms of keratosis disappear. Aloe will provide the skin with nutrients, reduce the severity of inflammation, eliminate itching and relieve increased dryness characteristic of keratosis;
- Propolis - can be used to treat keratosis in children over 1 year old; at an earlier age the risk of an allergic reaction is too high. The affected areas of the skin are covered with a thin layer of propolis, a gauze bandage and cling film are applied on top to create a thermal effect. The compress can be left in place for 24 hours; after 2 days the procedure can be repeated. Usually 2-3 compresses are enough to reduce the severity of keratosis symptoms; This method is especially effective in the development of inflammation;
- Baths with added starch are recommended for children over 3 years old. For this procedure, you will need to dilute 500 grams of starch with cold water to obtain a solution, which is then poured into the bath. The duration of the procedure should not exceed 30 minutes; after its completion, it is necessary to rinse the child’s body with water, wipe it and treat it with baby cream. Taking 2-3 for 1.5-2 weeks allows you to get rid of the main symptoms of keratosis.
Ways to cure the disease (2 approaches)
Keratosis pilaris does not always require treatment. If the manifestation is minor, it will be enough to eliminate the itching and inflammation so that the skin defect is not so visible. There are several ways to relieve symptoms of the disease.
Use of medications
Since the development of this skin anomaly is mainly associated with a deficiency of vitamins, the doctor first prescribes tablets that help fill the deficiency (like Etretinate and Notigazon).
Dosage varies depending on the severity of the lesion and is usually prescribed in the range of 25-75 g per day.
You cannot take several medications with retinoids at the same time.
Dermatological surgeon Christian Halvorson
To restore the skin when treating keratosis pilaris, special creams and ointments are often used.
Typically, they contain: salicylic acid and AHA acid. They promote the rejection of keratinized crust from the skin surface.
Ointments with vitamin A are also recommended for use (Tazarotene, Uriage and Klindovit gels have proven themselves to be excellent).
On Rusmedserver (medical discussion forum) you can find many positive reviews regarding Uriage Keratosane urea cream. Of all those available, it gives the most effective result in the fight against cutaneous keratosis.
Release form: metal tubes with a capacity of 40 and 75 ml. The price for this product varies between 700-1500 rubles.
This cream-gel is cloudy white in color, easy to apply and quickly absorbed without leaving a trace. After it there is a short feeling of tightness.
Due to the urea in the composition, the skin is moisturized and receives protection in the form of a film that retains moisture inside and minimizes the impact of external factors. Urea also removes dead skin particles well, relieves pain and accelerates healing.
Cosmetological approach (4 procedures)
A cosmetologist in the salon will help you get rid of the stratum corneum and nourish the skin with important components. Treatments for keratosis pilaris include:
- Chemical peeling. The skin is exposed to acids due to the application of various active compounds. Depending on the degree of impact, peeling can be superficial, medium and deep. It is selected depending on the skin type and the strength of its keratinization.
- Brossage. Facial cleansing using a special device with a rotating head on which an antiseptic gel or scrub is applied.
- Ultrasonic exposure . Cleanses the skin without mechanical influence. Ultrasonic waves are used here to create acoustic pressure. In this way, it is possible to quickly and painlessly remove the dead layer of the epidermis.
- Cryotherapy. Based on the action of liquid nitrogen. As a result, the skin takes on a healthy appearance and metabolic processes at the cellular level are normalized.
Laser treatment of keratosis is also used. But this method should be resorted to only when the disease is advanced.
Glycolic scrubs or chemical peels work great. Glycolic, retinol and trinion creams also help.
Dermatological surgeon Ben Behnam
Physiotherapy methods
Physiotherapy is usually prescribed for the treatment of acquired keratosis or in the acute course of the congenital form of the pathology.
The following methods are effective:
- Exposure of the epidermis to directed ultraviolet rays using quartz treatment - the procedure stimulates the natural synthesis of vitamin D in the body, destroys attached pathogenic microflora and reduces the severity of inflammatory processes in the lesions;
- Taking medicinal baths with the addition of sodium chloride or baking soda - the dosage of the components is determined by a specialist individually. After completing the procedure, it is necessary to treat the skin with baby cream or any cosmetic product with a moisturizing effect.
Follicular dermatitis: what is it?
Follicular dermatitis is an infectious skin lesion that manifests itself as a painful, purulent rash surrounded by redness. Pustules (or follicular papules) look like goose bumps. These are dense round nodules. They appear on the thighs, buttocks, arms, face and head. Along with them, redness, discharge of pus and sebum occur. Bursting pimples become covered with a yellow crust, which then peels off. People with symptoms of follicular dermatitis often report an elevated temperature.
Follicular dermatitis
In official medicine, this disease is also called “follicular keratosis.” It affects people of all ages and differs from other dermatitis in the absence of itching and flaking. Follicular dermatitis is not dangerous to health and rarely causes complications. The main problem faced by patients with this diagnosis is cosmetic. Skin affected by the disease looks unattractive. Facial papules are difficult to hide with cosmetics and often leave behind scars.
Recommendations for treatment and useful tips
It is important for parents to know a number of useful tips related to the treatment and prevention of keratosis in children:
- Taking hot baths or visiting a sauna in the absence of contraindications in a child reduces the risk of developing keratosis , since hot steam has a positive effect on the condition of the skin.
- Carrots with low-fat sour cream, kiwi and blueberries should be included in the child’s diet . All these products are beneficial for the body, and they also contain substances that help combat skin problems;
- Periodically, it is recommended to give your child a massage , but it is not necessary to contact specialists; you can massage various parts of the body yourself with a mitten, stimulating blood circulation;
- Protecting a child from chapping and frequent hypothermia is good protection not only from keratosis, but also from many problems with children's health.
Signs of keratosis
Keratosis pilaris can appear on the scalp, elbows, shoulders, knees, buttocks and thighs - where the skin is driest.
In the first case, the symptoms are as follows:
- The skin becomes rough and rough.
- Multiple red bumps appear, like pimples.
- The skin is extremely itchy.
- Hair falls out and breaks a lot (sometimes leading to baldness).
- Dandruff appears.
If you have dry skin, you are more likely to develop keratoses.
Dermatologist Dendy Engelman
If left untreated, this type of keratosis will spread to other parts of the body.
When the face is affected, partial thickening and drying are noted, but without the formation of small scales. In severe cases, these areas become covered with a thick crust.
If goose bumps are found on the legs, shoulders and elbows, many do not take any action to treat the disease because they do not pay special attention to it. Such inaction leads to complications in the form of bleeding cracks, stiffness and pain during movement.
Dermatologist Emily Altman
Prevention of occurrence
Taking preventive measures can reduce the likelihood of re-exacerbation of keratosis pilaris, as well as the primary occurrence of pathology.
The main recommendations are given below:
- Treating the skin with a cream with a greasy consistency during the winter season;
- Normalization of the nutrition process - it is necessary to eat food according to a set schedule, exclude potentially harmful dishes from the diet, increasing the amount of vegetables, fruits and other foods high in vitamins and beneficial microelements;
- Taking children's vitamin and mineral complexes at the beginning of winter and spring;
- Buying clothes and linen for children made from natural materials;
- When bathing a child, use special children's personal hygiene products that are gentle on the skin;
- Normalization and adherence to daily routine and schedule;
- Maintaining a normal environment at home - the absence of conflicts and stressful situations is necessary to strengthen the nervous system;
- Stimulating the functioning of the immune system and ensuring the body's natural resistance to various pathologies.
It is necessary to instill in children a love of sports and a healthy lifestyle from an early age, to do morning exercises and, in the absence of contraindications, to strengthen the body.
Prevention measures
In case of a congenital disease, from the first days of the baby’s life, parents must monitor the cleanliness of his skin, performing all necessary hygiene procedures. The doctor will recommend ointments, creams, and cosmetics that will help avoid manifestations of the disease in older age. The following preventive measures will help prevent relapse of pathology:
- taking vitamin and mineral complexes;
- balanced diet;
- avoiding hypothermia;
- maintaining a normal psycho-emotional state;
- strengthening the immune system;
- selection of quality body care products.
Acquired keratosis is difficult to prevent, but this can be done with timely treatment of skin diseases, proper nutrition, personal hygiene, and hardening of the body. An important rule is regular examination by a doctor. Keratosis pilaris is harmless, but can affect quality of life. This problem should not be ignored, because without treatment there is a risk of complications.
What to remember
- If you have a genetic predisposition to keratosis pilaris, lead a healthy lifestyle and watch your diet.
- At the first signs of the disease, begin treatment immediately. Take baths with herbal decoctions (chamomile, celandine, calendula), starch baths.
- Lubricate and moisturize problem areas of the skin (baby cream, Vaseline), wipe problem areas with salicylic acid.
- Sign up for physical therapy for quartzing. Ultraviolet rays have a beneficial effect on the skin.
- Avoid direct sunlight on problem areas.
- Do not scratch and try not to damage the skin, otherwise it will cause inflammation.
The condition of your body and skin directly depends on what actions you take, how you care for your skin, and what you eat. Strictly follow all the recommendations given in the article, and then your skin will always be healthy and no rash will appear on it.