What is lichen
How compatible are concepts such as pregnancy and lichen?
Ringworm is a collective name for various dermatological diseases, which are characterized by the formation of spots of different sizes, shapes and colors on the skin. In other words, it is not one specific disease. There may be several of them, and depending on which of them manifests itself in a woman, the further prognosis will depend.
Ringworm appears in a pregnant woman due to three reasons:
- viruses;
- fungal infection;
- complicated allergic reaction.
The effect of certain microorganisms on the internal state of the body determines the development of the disease. You can either become infected from someone, or get it due to a predisposition.
Provoking factors
Ringworm in a pregnant woman is a fairly common occurrence, which is associated with decreased immunity during this period. This happens due to the peculiarity of hormones in an “interesting position”, which suppress the immune system. What is necessary for successful gestation and development of the fetus.
At the same time, a “dormant” immune system is not able to fight back the negative influence of the environment. This leads to exacerbation of chronic diseases and the emergence of new diseases.
However, not only hormones lead to the fact that during pregnancy the body’s defenses are reduced, and lichen, a photo of which you can see, blooms wildly. There are other negative factors, the action of which is a real blow to the immune system. Among them:
- stress;
- acute viral diseases;
- lack of sleep;
- lack of nutrients.
It would seem that such simple things that every person regularly encounters actually cause irreparable damage to health.
Prevention
Simple preventive recommendations will help reduce the risk of developing the disease during pregnancy:
- preventing contact with an infected person;
- immunotherapy;
- consumption of fortified foods;
- regular observation by a gynecologist;
- avoid overheating and hypothermia;
- compliance with personal hygiene rules;
- selection of clothes made from natural fabrics, loose fit;
- limiting contact with pets.
Simple rules will help reduce the risk of disease.
Ringworm generally does not pose a health threat. But many drugs, even for external use, are contraindicated for pregnant women. Therefore, it is not recommended to self-medicate.
The material was prepared specifically for the website kakrodit.ru, edited by doctor E.Yu. Churilina. Specialty: dermatovenerology, general hygiene.
Ringworm
To talk about whether it is dangerous when pregnant women develop lichen, we will start with its most unpleasant type. Why unpleasant? Because it is this disease that brings the most discomfort, and getting infected is as easy as shelling pears.
Many people have heard about ringworm. It is considered a childhood disease, but it often affects adults as well. There are two varieties:
- Trichophytosis is caused by the action of fungi that parasitize only in the human body. You can get it from a sick person.
- Microsporia is the result of a fungal infection that can live both in the human body and on the body of an animal. Most often it is infected from indoor or outdoor cats and dogs.
Surely, everyone in childhood heard an instruction from their mother that you should not touch animals with visible bald spots on their bodies, because the same thing will appear on yours. These weren't horror stories. Lichen microsporia in pregnant women appears precisely as a result of such contact. Moreover, you can catch the disease even from an animal that at first glance seems healthy. The fact is that a fungal infection can be hidden in places that are inaccessible to your view, for example, on the stomach or in skin folds.
To say that the disease is highly contagious is an understatement. Both microsporia and trichophytosis are easily transmitted through any contact with patients. Moreover, fungal spores can remain in the environment for a long time and remain viable. So, ringworm during pregnancy can be acquired through:
- sand and soil;
- grass;
- household items;
- water;
- tools in the hairdresser, etc.
As you can see, it is very difficult to protect yourself from infection, but fortunately, the fact that it gets on your hands or any other area of the skin is not enough to cause serious damage. If there is no damage to the skin, then the spores will not be able to penetrate the body and begin to actively act there. In addition, they are easy to destroy with water and ordinary soap.
Wash your hands often, especially after playing with your cat or dog!
Symptoms of the disease
The photo shows a favorite place for ringworm in pregnant women - the scalp. It can also appear on nails and smooth skin. It got its name “ringworm” due to its characteristic symptom – the appearance of bald patches on the affected areas of the head.
Usually one inflammation appears, less often several smaller ones. The hair in this area thins and then breaks off a few millimeters above the roots. The skin begins to peel off and turns pink. The edge appears slightly brighter than the center. If the disease affects smooth skin, several spots appear there, and their color is brighter than on the head.
Is lichen dangerous during pregnancy? Despite its unsightly appearance and some discomfort, it does not pose any threat to the unborn baby or his mother. If you consult a doctor in time and start treatment, you can completely get rid of it in 2-3 weeks.
Symptoms of the disease during pregnancy
Like any other skin disease, lichen versicolor has characteristic symptoms. Their appearance should be a reason to contact a specialist (dermatologist), who will examine the pregnant woman, prescribe treatment and give appropriate recommendations.
How does lichen manifest itself:
- The areas around the mouth of the hair follicle become yellow in color - this indicates that pityrospora fungi have begun to multiply.
- Small spots form on the skin, the color of which can range from yellow to pink. As the spot enlarges, its color may change to brown.
- The spots grow and connect with those located nearby. Large lesions form. They can cover large areas of skin.
- Skin lesions have scalloped edges.
- Pityriasis-like scales can be seen on top of the spots.
Quite often you may encounter spots appearing on the skin that are much lighter than healthy skin. It was not possible to fully understand the issue of their appearance. But it can be assumed that the reason for their formation is the lack of ultraviolet access to the epidermis. This is caused by the fact that the structure of the lesions is loose and keratinized.
Typically, lichen affects the upper part of the body. Lesions can occur on the arms, chest, shoulders, abdomen, thighs, and head.
Ringworm Zhibera
Zhiber's lichen is called pink, or catarrhal. Why a cold? Because it often makes itself felt just at the moment when a person is suffering from ARVI. It is believed that the disease awakens against the background of reduced immunity.
This type of lichen has not yet been studied, so its true causes are unknown. In addition to poor immune function, its development can be affected by a predisposition to allergies. Most scientists believe that the disease is neuro-allergic in nature. It is not contagious.
Ringworm during pregnancy looks like pink spots of different sizes, which are most often located on the torso, less often on the head and limbs. Usually, a large maternal spot forms first, and after a few days, slightly smaller daughter spots.
The spots begin to peel off from the center, changing color to yellowish. A bright pink ring remains around the edges. Often the disease no longer bothers the pregnant woman. Any discomfort is not typical, but against the background of a weakened immune system, there is a risk of secondary infection on the damaged skin, which will lead to suppuration. Also, due to nervous experiences, itching occurs, which is sometimes very annoying.
Treatment of pityriasis rosea during pregnancy is considered appropriate only if there is severe itching or large areas of skin are affected. In all other cases, the disease goes away on its own in 1.5-2 months. It is not dangerous for the mother, the baby, or others, as it is not at all contagious.
Treatment tactics
Ringworm should be treated only after examining the sick woman. Diagnostics includes a detailed survey, examination of the skin, identification of Beignet's symptom (flaking of scales when the affected areas of the skin are scraped), examination of the scalp under a Wood's lamp, microscopic examination of material taken from the skin (scales). A general and biochemical blood test is also required. If pityriasis versicolor is detected, treatment during pregnancy should be carried out only with topical agents. Additionally, folk remedies can be used.
Systemic antifungal drugs are not used as they can affect the fetus and the course of pregnancy.
Treatment of pityriasis versicolor involves the use of antifungal ointments (Lamisil, Ketoconazole). Clotrimazole can be used, but it is contraindicated in the 1st trimester of pregnancy. During pregnancy, Tolmitsen cream can be used.
Treatment often involves the use of various antiseptic solutions (iodine, sodium thiosulfate). You can treat the affected areas of the skin with vinegar. Additionally, treatment with folk remedies can be organized. For this purpose, you can use various herbs (celandine, sandy immortelle, St. John's wort, fresh sorrel). Decoctions and infusions are prepared from herbs. They can be ingested without fear and used to wipe the skin. For a speedy recovery, you need to strengthen your immune system. To do this, women are advised to normalize their diet, cure concomitant chronic diseases, and take vitamins. To keep your skin clean, you need to shower regularly.
Pityriasis versicolor
Pityriasis versicolor, cauliflower, or, as it is also called, beach lichen during pregnancy is another fairly common occurrence. It occurs against a background of reduced immunity and is not contagious. The reasons that cause it are still unknown. There is an assumption that it is caused by specific fungi, due to which the pigmentation of the skin is disturbed. However, these fungi live on the body of every person, so the version about the poor state of the immune system in this case is confirmed.
The disease is characterized by the appearance of spots of various sizes, which are located at some distance from each other and do not merge. The spots are lighter than the base color of the skin. They are best visible on dark-skinned people, especially if they tan. The tan does not stick to stains. Because of this, they may be more pronounced in the summer than in the winter, when a person’s skin becomes lighter.
Apart from changes in skin color, nothing else happens during the disease. It is extremely rare that spots can become inflamed in winter and slightly peel off, which can be easily prevented by proper body hygiene and the use of moisturizers. The answer to the question whether tinea versicolor is dangerous during pregnancy is negative. It does not affect the child or the woman’s body in any way.
Lichen planus
Lichen planus is typical for women over forty, but with reduced immunity it can appear at a younger age. This disease is not caused by the action of any microorganisms and is not transmitted to others. Scientists have not yet been able to figure out what exactly its development is connected with. Many studies indicate a connection with a person’s nervous state or allergies to something.
Before treating lichen during pregnancy, you need to make an accurate diagnosis, differentiating it from other similar diseases. This disease is accompanied by:
- intense itching;
- the formation of small flat nodules on the flexor areas of the limbs, inner thighs, armpits or groin. Sometimes lichen appears on the oral mucosa.
There is a depression in the middle of each nodule. Individual elements of inflammation often merge into plaques, on the surface of which a mesh pattern can be seen.
As in previous cases, the disease is not at all dangerous and only causes physical and moral discomfort.
Herpes
Lichen vesica in pregnant women is the most common of all varieties of this disease. In another way it is also called “herpes”, or “cold” on the lips.
Who hasn’t at least once encountered unpleasant rashes in the form of itchy watery blisters? After hypothermia or against the background of acute respiratory infections, they appear right there!
Lichen vesica is caused by the herpes simplex virus. Do not be afraid of herpes infection, as it accompanies most people from childhood. There is no treatment for it. The only thing that can be done is to avoid relapses by strengthening the immune system.
During pregnancy, herpes can be truly dangerous only in one case - if the infection first occurred during pregnancy. This is difficult to imagine, since it usually occurs between the ages of six months and 4-6 years. The virus is highly contagious and, given that 95% of all people are carriers of it, it is impossible to hide from it.
Shingles
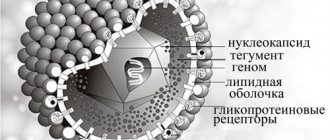
Shingles, or herpes, is the result of another herpes infection.
Herpes virus type 3 or Varicella-Zoster is no less common than the previous virus. During primary infection, it causes chickenpox in children. After recovery has occurred, a person forever develops immunity to this disease. However, the virus remains in the body, and already in adulthood it can manifest itself as shingles.
The disease is quite severe, with very unpleasant symptoms, but does not pose a danger to the unborn child. However, the woman will have to suffer, since the infection causes, in addition to rashes, severe neuralgic pain. And all because the virus attacks the nerves.
Treatment in this case should begin immediately. Therefore, if characteristic blisters appear on the body, immediately contact a dermatologist or infectious disease specialist.
What could be the causes of lichen?
It is necessary to understand that the cause of this skin disease can be anything. The main causes of the disease in pregnant women are considered to be hormonal imbalance in the body, as well as contact with a person who is already suffering from shingles.
The following are possible causes of infection in pregnant women:
- insufficient amount of vitamins in the body;
- manifestation of allergies;
- hypothermia;
- fatigue, weak immunity, severe stress;
- disruption of the normal flow of hormones;
- direct contact with the carrier of the disease (people, animals);
For the baby in the womb, lichen is completely harmless, but for the expectant mother it can cause severe discomfort.
Treatment of lichen in pregnant women
It is important to consult a doctor for any changes in the skin, since it makes sense to treat lichen in a pregnant woman only in two cases, if it is ringworm or shingles. For the first disease, local and systemic antifungal drugs are prescribed, and for the second, antiviral therapy is prescribed.
For other types of lichen, the use of medications may occasionally be necessary to eliminate unpleasant symptoms. How to treat lichen planus during pregnancy, which is very itchy? For this purpose, antiallergic drugs are used. Taking other medications is useless as they cannot speed up the healing process.
If a secondary infection occurs with any type of lichen (bacterial or fungal in nature), antibiotic therapy will be required. Therefore, for any skin diseases, it is important to follow the rules of hygiene.
What to apply for ringworm during pregnancy should be told by your doctor, whom you should contact if something bothers you. During this period, not many products are allowed to be used, so consultation with a specialist is of great importance. There are also universal “harmless” antiseptic and emollient creams that can be used without a prescription. These include Bepanten and Sudocrem.
Danger for pregnant women
During pregnancy, lichen is transmitted to a woman from an infected person or animal through household contact. In some cases, fungi can enter human skin through hairdressing tools, hygiene products and bedding.
Pityriasis versicolor is considered harmless, so usually treatment for pityriasis versicolor does not cause harm to the fetus. Systemic therapy (in tablets) is used only in advanced form. To minimize the negative impact on the fetus, doctors prescribe local medications that eliminate the external manifestation of symptoms. Full treatment is carried out after childbirth.