Erysipelas occurs due to streptococcus, which causes the disease by penetrating through microtraumas on the skin. The presence of erysipelas manifests itself in redness, swelling, and a shiny area of the skin, accompanied by high fever, sometimes headache and nausea. Treatment of this disease at home is permissible after consultation with a doctor.
Related articles:
Getting rid of itchy skin at home - quickly and effectively We treat pediculosis in children using traditional methods We treat seborrhea on the head in children Causes and treatment of herpes on the lips Treatment and photos of warts on the legs
Forms
Erysipelas of the skin of the leg has several types:
- The erythematous form is the most common disease with classic symptoms.
- The bullous type is characterized by the formation of blisters with transparent contents.
- The hemorrhagic variety affects small vessels and capillaries, which form blisters filled with blood.
- The necrotic form is the most severe course of the disease. It looks like necrosis of the skin with infection penetrating deep into the tissue.
- Wandering type - the disease can form over several days in different parts of the body on the right or left side. The previous inflamed area is healing. This form is typical for newborns.
Causes of erysipelas
The bacterium responsible for causing erysipelas is group A beta-hemolytic streptococcus, which is highly survivable but has low resistance to heat. This microorganism provokes an infectious-allergic response of the body. Patients with erysipelas who have the following risk factors consult a doctor:
- diabetes;
- decreased immunity;
- minor skin damage due to the presence of streptococcus in the body;
- fungal infections;
- wearing synthetic or simply tight clothing and shoes;
- presence of chronic diseases;
- occupational hazards;
- degenerative processes of the skin;
- lack of vitamins in the body.
When beta-hemolytic streptococcus enters the body, erysipelas does not always manifest itself, since this requires a predisposing factor.
The source of infection can be either a sick person or a carrier. Therefore, the main rule is to prevent the progression of trigger factors. When a doctor treats erysipelas, he must explain to the patient how to reduce the number of relapses or achieve their complete elimination.
Symptoms
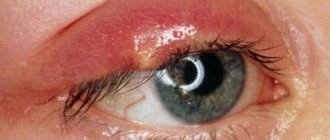
Erysipelas on the legs begins in the latent stage. The incubation period of the infectious disease lasts up to 5 days. Erysipelas may affect the lower leg or another part of the body. The disease is accompanied by fever and a rise in temperature up to 40 degrees. The patient is weakened, quickly gets tired, drowsiness, apathy, and increased sweating appear. Local symptoms of erysipelas on the legs begin a few hours after a change in the general condition of the body.
Erysipelas of the leg is characterized by:
- Severe hyperemia, which slightly rises above healthy areas of the skin and is delimited from them by a roller.
- Soreness when touched.
- Swelling in the affected area. Swelling can affect the lower limb from the toes to the knee.
- Enlargement of nearby lymph nodes.
- The appearance of rashes in the form of blisters filled with clear or hemorrhagic liquid.
Is erysipelas on feet contagious to other people?
Since the infection is caused by Haemophilus influenzae streptococcus, the disease is contagious to others. The pathogen can infect a person who cares for the patient and, accordingly, comes into contact with him.
When carrying out hygienic procedures for treating an inflamed surface, you should wear gloves and wash your hands thoroughly with soap.
Also, the sick person must be provided with personal items (dishes, towels, clothes).
Variants of the course of the disease
Erysipelas begins violently and acutely. A person is seized by a fever with a headache, chills, nausea or vomiting, and severe weakness, which quickly intensify as the body becomes increasingly intoxicated. The affected area of the skin turns red, swells, because of this it becomes very stretched, and the slightest touch to it causes pain.
The duration of the disease depends primarily on the form of erysipelas and the degree of streptococcal intoxication. If the skin turns purple and swells, it is erythematous erysipelas. In the hemorrhagic form, the capillaries burst and pinpoint hemorrhages occur.
And with bullous erysipelas, in addition to the rash, blisters with watery contents also form, similar to blisters, such as occur with burns. When they subside, the skin becomes covered with crusts, which peel off only after two to three weeks. The disease drags on if non-healing ulcers form in their place.
If the foci of erysipelas are small and the patient immediately began treatment, then the febrile state does not last long, only two to three days, and after five to six days the rash goes away completely. With moderate intoxication, acute inflammation lasts for about a week, and the redness goes away after ten days.
In severe cases, when the lesions are extensive, the temperature is under forty, vomiting is exhausting, treatment can last for two to three weeks or even more.
Often, symptoms of severe poisoning of the body with streptococcal toxins occur when erysipelas metastasizes in places far from the original source of inflammation. In the bullous form, residual effects - peeling, slight swelling, skin pigmentation, peeling of dry crusts - take at least another week.
Diagnostics
Before making a diagnosis and starting treatment for erysipelas on the leg, you should consult a specialist to undergo examinations.
Basic methods:
- Taking anamnesis and visual inspection of the affected area.
- Palpation of the inflamed area and lymph nodes, assessment of the condition of the skin under pressure.
- Blood for general analysis, biochemistry.
- Additionally, Doppler or rheovasography of the vessels of the lower extremities is prescribed, and in rare cases, angiography.
If necessary, the therapist will refer you to specialists for consultation.
Prevention of the disease
The prerequisite for the appearance of this disease is a weakened immune system and various types of injuries. Therefore, every person should try to avoid possible damage. This applies to working with various household appliances and devices, as well as playing with animals.
Particular attention should be paid when a person has a weakened immune system.
Streptococcus, which lives in almost every human body, is immediately activated. If an injury has been sustained, even a minor one, it must be immediately treated with an antiseptic. This action will help avoid the appearance of erysipelas in the future.
Quite often, it is enough for a person to start watching his diet and strengthening his immune system so that this disease does not bother him.
If pathology has been identified, then treatment should be started immediately. Once the disease is defeated, a person should focus on strengthening their own health to prevent re-infection. This is not difficult to do; as a rule, the doctor carries out preventive prescriptions after treatment. In this case, the patient must strictly adhere to all the doctor’s recommendations.
Treatment
Erysipelas on the legs should be treated comprehensively. Basic principles of therapy include:
- elimination of the infectious agent;
- reduction of inflammation;
- strengthening the body's defenses;
- removal of toxins and normalization of blood circulation in the affected part of the body.
Nutrition for erysipelas of the leg
In order for the treatment process to be as effective as possible, you should adhere to a certain menu:
- The patient is prescribed a strict diet. It is necessary to drink more clean water, as well as lemon or orange juice (if you are not allergic to citrus fruits).
- Two days after the onset of the disease, fruits are introduced - apples, pears, peaches: they help the body remove toxins.
- Dairy products and honey should be present in the diet daily, provided they are tolerated.
- Food should be steamed, boiled or baked. Cereals, lean meats and fish are allowed.
When recovery may take longer
Whatever the form of the disease, the lymphatic system of the body is always affected. And the duration of treatment for erysipelas also depends on the degree of its damage. After all, it is necessary to treat not only the skin, but also lymphadenitis - inflammation of the lymph nodes or lymphangitis - inflammation of blood vessels. A particularly severe complication may develop: elephantiasis of the legs, and then treatment may take more than one month.
Primary erysipelas most often appears only on the face and can be forgotten quite quickly. But the disease is insidious in that it often returns, affecting the legs. This is especially likely if there are problems with the veins of the extremities (varicose veins or thrombophlebitis), or skin diseases, allergies, or bronchial asthma. It happens that erysipelas goes away and appears again over many years and even decades.
Any form of this disease has age-related characteristics. For example, children rarely get erysipelas, but easily and recover quickly. But in older people, the disease is usually much more severe, and the acute febrile period can last about a month with exacerbations of concomitant chronic diseases.
Finally, recovery can be significantly delayed if the patient’s skin is exposed to ultraviolet rays. If you mistakenly use compresses or ointments that stimulate blood circulation to relieve swelling, then the infection spreads throughout the body. Or use traditional medicine recipes, having no idea what the form and stage of the disease are, and not taking into account concomitant diseases.
Variants of the course of the disease
Erysipelas begins violently and acutely. A person is seized by a fever with a headache, chills, nausea or vomiting, and severe weakness, which quickly intensify as the body becomes increasingly intoxicated. The affected area of the skin turns red, swells, because of this it becomes very stretched, and the slightest touch to it causes pain.
The duration of the disease depends primarily on the form of erysipelas and the degree of streptococcal intoxication. If the skin turns purple and swells, it is erythematous erysipelas. In the hemorrhagic form, the capillaries burst and pinpoint hemorrhages occur.
And with bullous erysipelas, in addition to the rash, blisters with watery contents also form, similar to blisters, such as occur with burns. When they subside, the skin becomes covered with crusts, which peel off only after two to three weeks. The disease drags on if non-healing ulcers form in their place.
If the foci of erysipelas are small and the patient immediately began treatment, then the febrile state does not last long, only two to three days, and after five to six days the rash goes away completely. With moderate intoxication, acute inflammation lasts for about a week, and the redness goes away after ten days.
In severe cases, when the lesions are extensive, the temperature is under forty, vomiting is exhausting, treatment can last for two to three weeks or even more.
Often, symptoms of severe poisoning of the body with streptococcal toxins occur when erysipelas metastasizes in places far from the original source of inflammation. In the bullous form, residual effects - peeling, slight swelling, skin pigmentation, peeling of dry crusts - take at least another week.
Which doctor treats erysipelas of the legs?
Erysipelas is caused by a streptococcal pathogen, which is difficult to treat. The disease has a short name by which most people know it – erysipelas. Many people have heard this name, but few people know which doctor treats erysipelas of the legs.
Those diagnosed with erysipelas must be committed to persistent and long-term treatment. You also need to know that this disease often recurs, so in some cases it takes years to solve the problem.
The most common locations for erysipelas are the face, arms and legs. This pathology occurs most often on the legs, since the lower extremities, as a rule, have obstructed venous outflow, which contributes to the development of erysipelas.
How does infection occur?
The causative agent of this pathology is group A streptococcus. It mainly affects women over 50 years of age. With weakened immunity, hypothermia, stress, damage to the integrity of the dermal integument or chronic fatigue, the chance of developing erysipelas increases many times over.
Infection occurs through direct contact with an infected person or carrier, sometimes the introduction of streptococcus occurs through contact with infected blood.
The high-risk group includes people with the following diseases:
- Diabetes;
- Obesity;
- Mycoses;
- Chronic infections (otitis media, caries, tonsillitis);
- Varicose veins;
- Alcoholism.
Symptoms of various forms
After contact and penetration into the skin, the incubation period lasts 3–5 days, and then symptoms begin to develop:
- Indicators of acute toxicity are temperature reaching 40°C, throbbing headache, weakness, vomiting and nausea.
- The appearance of local signs of infection.
External symptomatic manifestations are very dependent on the form of pathology. There are three of them in total.
Erythematous
The lightest of all forms. Redness of the skin with clear boundaries is characteristic. The reddened areas rise slightly above the level of the dermis and tend to increase in size. There is a burning sensation, pain and swelling at the sites where the lesions appear. You can feel the increased temperature of the inflamed skin to the touch.
Bullous
It is named so because of the presence of specific bullae - blisters with serous contents. After a few days, the bullous-looking blisters transform, leaving brown crusts in their place. These crusts fall off after a couple of weeks, after which ulcers and erosions are visible on the skin.
Gangrenous-necrotic
This form is the most severe and in most cases is the result of long-term treatment with traditional methods. Small hemorrhages and disruption of the integrity of blood vessels are noticeable in the affected areas.
Diagnostics
In order to understand the diagnosis and receive the correct treatment, you need to contact an infectious disease specialist or surgeon.
Specific manifestations allow a diagnosis to be made. Since erysipelas has similar symptoms to many dermatological diseases, the acute onset of the disease with symptoms of intoxication is important.
The specialist will require a blood test, which can be used to diagnose a bacterial infection, as it can be determined by an increased level of neutrophils and leukocytes.
In addition, a conversation with the patient helps to create a complete clinical picture and confirm assumptions with a number of specific signs of erysipelas:
- Localization of lesions;
- Typical signs of lesions;
- Enlarged lymph nodes;
- Disappearance of pain at rest.
A complete diagnosis is carried out with the detection of antibodies to hemolytic streptococcus and identification of the pathogen.
Treatment
After consulting a doctor and differentiating the pathology, treatment can be prescribed. For the treatment of mild forms of erysipelas of the legs, outpatient conditions are sufficient; inpatient treatment is recommended only for advanced cases of bullous or gangrenous-necrotic forms. Inpatient treatment is also preferable for children and elderly people.
To successfully combat erysipelas, three types of treatment will be used.
Drug treatment
The main remedy for getting rid of erysipelas is antibiotic therapy. Bacteria of this genus most often show sensitivity to the penicillin series, nitrofurans and sulfanilamide. The administration of these antibiotics can be intravenous or intramuscular; standard dosages are used. Usually a five-day or seven-day course is sufficient.
Sometimes oral antibiotics of mixed groups are chosen, which also gives quick results. Manifestations of the disease begin to decrease within a few days: the temperature drops to normal values, the lesions become less bright, turn pale and after 1 - 3 days they decrease to the general skin level. Drug therapy can be supplemented by taking sulfatone in the form of injections or tablets.
In cases of superficial damage, local antiseptic preparations are also used: various powders, tablets crushed into powder and ointments.
In combination therapy, simultaneous use of antihistamines and non-steroidal anti-inflammatory drugs is prescribed.
For severe forms, sometimes they develop support with vitamin preparations and biostimulants, and sometimes they recognize the need for plasma or blood transfusions.
Physiotherapeutic methods
Thanks to the use of physiotherapeutic procedures, you can reduce the risk of relapses and hope for a complete cure of erysipelas of the legs.
UHF is successfully used to treat affected areas, where skin tissue is restored after this procedure.
For a recurrent course, ozokerite therapy and paraffin therapy are prescribed. These thermal procedures have a positive effect on the chronic inflammatory process.
During an acute course, the use of phono- and electrophoresis with hydrocortisone is recommended.
Sometimes antibiotic therapy is combined with freezing of the superficial epidermis through cryotherapy.
Surgery
For bullous and gangrenous-necrotic forms of erysipelas of the legs, surgical methods are often used.
Success in this case depends on how early the patient contacted the surgeon. Under operating conditions, the surgeon will be able to open purulent lesions of the lower extremity and ensure the outflow of pus after opening the bulla. The surgical method is an effective means of stopping the spread of suppuration.
The main means of preventing erysipelas of the legs are maintaining hygiene, treating skin lesions with antiseptic solutions and maintaining a high immune status.
Consultations with a doctor online Taking care of your health is a life priority for everyone. Communicate with doctors online and receive qualified assistance without leaving your home. Try it
Note! The information on this page is provided for informational purposes only. To prescribe treatment, you must consult a doctor.
July 26, 2017
Source: https://DocTown.ru/kto-lechit/rozhistoe-vospalenie-nog/
How to deal with swelling
Dealing with swelling after childbirth is not always easy. After an easy birth, fluid exchange can normalize on its own and the patient will begin to feel well. In healthy women, edema completely resolves 1-2 months after childbirth; this usually occurs during the first weeks of the baby’s life.
In order to speed up this process, a woman is recommended to bandage her legs with elastic bandages and regularly perform exercises that require lifting her legs. The simplest exercise is a simplified version of the famous “birch” exercise - you need to lie on your back and raise your legs, leaning on some support, for example, a wall.
Complications
If treatment for erysipelas is not started when the first signs of the disease appear, complications such as:
- An abscess, which is a cavity filled with pus and delimited from healthy tissue by a capsule of connective tissue.
- Cellulitis is a diffuse purulent inflammation of the subcutaneous fatty tissue that has no definite boundaries.
- Phlebitis is inflammation of the vein walls. A condition in which a blood clot forms in the lumen of a vessel is called thrombophlebitis.
- Lymphostasis is a violation of the outflow of lymph from the affected areas with subsequent sweating into the soft tissues.
- Trophic ulcers are deep skin defects that do not heal for a long time.
- Meningitis is an inflammatory lesion of the membranes of the brain and spinal cord.
- Sepsis is a systemic inflammatory reaction that occurs as a result of the generalization of a local infectious process.
Changing your diet
The diet to combat edema is designed to reduce the intake of fluid and salts. The drinking regime is determined by the doctor based on the characteristics of each individual patient. Salt and salty foods are limited to the minimum required for health - 5 g per day. Salt promotes fluid retention in the body, swelling and increased blood pressure, so it is advisable to limit it to all pregnant women, even healthy ones.
In addition, limit protein intake. Its exact volume is also individual. Limiting protein helps reduce the load on the kidneys to speed up the process of removing fluid from the body. There are usually no restrictions on proteins and fats if a woman does not intend to lose weight.
Changing your diet alone is not effective enough to eliminate swelling. Reduced fluid intake alleviates the general condition, but does not affect the mechanisms that cause swelling.
Changing your diet helps achieve several goals at once: fully supplying the body with nutrients and vitamins, ensuring lactation, losing weight and fighting edema. To achieve a full result, the menu should be compiled together with a specialist - this will help avoid shortages of important elements.
When recovery may take longer
Whatever the form of the disease, the lymphatic system of the body is always affected. And the duration of treatment for erysipelas also depends on the degree of its damage. After all, it is necessary to treat not only the skin, but also lymphadenitis - inflammation of the lymph nodes or lymphangitis - inflammation of blood vessels. A particularly severe complication may develop: elephantiasis of the legs, and then treatment may take more than one month.
Primary erysipelas most often appears only on the face and can be forgotten quite quickly. But the disease is insidious in that it often returns, affecting the legs. This is especially likely if there are problems with the veins of the extremities (varicose veins or thrombophlebitis), or skin diseases, allergies, or bronchial asthma. It happens that erysipelas goes away and appears again over many years and even decades.
Any form of this disease has age-related characteristics. For example, children rarely get erysipelas, but easily and recover quickly. But in older people, the disease is usually much more severe, and the acute febrile period can last about a month with exacerbations of concomitant chronic diseases.
Finally, recovery can be significantly delayed if the patient’s skin is exposed to ultraviolet rays. If you mistakenly use compresses or ointments that stimulate blood circulation to relieve swelling, then the infection spreads throughout the body. Or use traditional medicine recipes, having no idea what the form and stage of the disease are, and not taking into account concomitant diseases.