Dermatomycosis is a very common infectious disease in which the fungus affects the skin of the torso, scalp, nail plates, plantar or groin area. Dermatomycosis manifests itself in the form of severely itchy, scaly red spots that have a rounded shape, from which, in severe cases, purulent discharge can come out of them.
For many, ringworm is better known as ringworm. People and animals can get sick from it. The disease is highly contagious and can spread to humans from pets. However, there are vaccines for animals that protect them from ringworm for a certain period of time. But there are no drugs to prevent this disease in humans yet.
Classification
Dermatomycoses are classified according to location:
- smooth body skin;
- scalp and beard;
- nails;
- groin area;
- stop.
Depending on the pathogen, dermatomycosis is classified into:
- keratomycosis: nodular microsporia, lichen versicolor;
- dermatophytosis: athlete's foot, athlete's foot, trichophytosis, imbricate mycosis, favus, rubrophytosis;
- deep mycoses: aspergillosis, chromomycosis, blastomycosis, sporotrichosis, etc.;
- candidiasis: superficial, visceral and chronic generalized;
- pseudomycosis: actinomycosis, trichomycosis, erythrase, etc.
Pathology affecting the feet
Dermatomycosis of the smooth skin of the feet, a photo of which you can find in this article, first occurs on the skin between the toes, after which it begins to gradually spread over the entire surface of this part of the body. The skin begins to turn red, peel and become covered with dry cracks. If the disease is not treated on time, it can lead to suppuration. In this case, the disease causes extremely unpleasant sensations in the patient. His skin begins to actively itch and itch. Sometimes it is simply unbearable to endure, so the patient begins to scratch the damaged areas of the skin, which leads to a significant deterioration of the condition.
Causes
Speaking about the etiology of the disease, it is important to take into account that the causative agents are a variety of fungi: microsporum, trichophyton, epidermophyton (the latter group includes varieties of this type of fungus, all of them are united under the common name “dermatophytes”). It is always extremely difficult to identify pathogens in body tissues, since a specialist must first isolate a pure culture for research.
Another difficulty is that the causative agents of dermatomycosis are very common, so infection occurs easily, and in some cases such manifestations may have something in common with epidemic symptoms. Most often, dermatomycosis is characteristic of countries with a tropical climate, that is, humid and hot, since fungi usually multiply actively at a temperature of 25-30 degrees Celsius. The summer season and alkaline environment are ideal for them. At the same time, experts say that children are much more likely than adults to become infected.
As a rule, the pathogen appears on the skin after a person has been in contact with the lesion for some time. Doctors distinguish three main types of pathogens:
- bestiality;
- geophilic;
- anthropophilic.
The source of infection in the first case is animals, or rather, parasites living in their bodies. This includes parasites that use domestic dogs, cats or cattle as hosts.
In the second case, we are talking about pathogens living in the ground and soil. A person can work or simply come into contact with the ground without using protective equipment, and as a result become infected.
The third case is parasites that live in the body of a person who is a carrier of the disease. The very fact of infection occurs through contact.
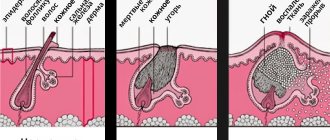
The development of dermatomycosis is expressed in the fact that conidia and hyphal fragments of pathogens enter the hair, upper layers of the skin, and nails (that is, those tissues that contain keratin). The degree of infection in dermatophytes is quite low, so tissue damage does not appear in healthy people. However, pathogens have a characteristic feature: they can subject keratin to complete destruction and destruction.
Pathogens located in the hair shaft can be divided into two types based on their growth. First: endothrix begin to grow from the skin into the hair and follicles, but they do not go beyond the boundaries of the hair shaft itself. Second: ectothrix grow directly into the hair directly from the hair follicle.
Much in the occurrence and development of the disease depends on the characteristics of the person’s body. Some types of dermatomycosis may be characteristic exclusively of an adult, while others - only of a child. In many ways, the disease is caused not only by age, but also by the secretion of the sebaceous glands, the composition of sweat and many other characteristic features.
Primary infection with dermatomycosis is a consequence of sensitization, after which it is time for a relapse to develop. Immunodeficiency largely determines the level of risk of dermatomycosis. In addition, various metabolic disorders, poor nutrition, problems with the hormonal system, and vitamin deficiency can also become a favorable background for infection. It is also important to remember that the fungus penetrates damaged skin faster, so people with ulcers, wounds and scratches on the skin are at particular risk.
Conidia, hyphae, and spores penetrate hair, nails and skin. Since the nutrient medium for the fungus is, first of all, keratin, the epidermis after infection begins to deteriorate at a rapid pace. In this case, healthy areas of the skin are also affected.
Optimal conditions for infection
Dermatomycosis of smooth skin, the photo of which can be simply amazing, prefers to live in humid conditions at a temperature of about twenty-five to thirty degrees Celsius. Also, the acidity of the skin is very important for their habitat.
As you know, the acidity of sweat changes with age in every person. The highest acidity level is observed in children before they reach the age of two. Until the age of twelve, these indicators gradually decrease. This means that childhood is an ideal age for dermatomycosis of smooth skin. Treatment at home for this disease can be carried out only after visiting a dermatologist and establishing an accurate diagnosis.
The acidity of sweat begins to increase again when the child begins a period of active sexual development. It is at this age that the immune system of adolescents is very active, which means that the likelihood of contracting fungal infections is minimized.
However, as a person begins to mature, his immune system can gradually deteriorate, as well as his general health and skin. The most optimal place for skin fungi to settle is between the toes. Unnatural shoes, as well as synthetic clothing in the summer, contribute to the accumulation of sweat, in which pathogenic microorganisms can begin to actively develop.
Symptoms of ringworm
In humans, the symptoms of dermatomycosis (see photo) depend entirely on its shape and location on the body. Dermatomycosis of the scalp is diagnosed more often in children. If it spreads to the scalp, then patients experience the following symptoms:
- pain, peeling and itching;
- rapid spread of rash in the form of papules;
- hair loss and fragility, which develops from purulent melting of the bulbs;
- the appearance of boils.
In the beard area, the phenomena are similar, but the pustular lesions are point-like, since the hair follicles are constantly infected. The skin here also becomes crusty and swollen. This form is highly contagious.
Dermatomycosis of the skin occurs in warm climates, as it is favorable for the rapid proliferation of the trichophyte fungus.
The symptoms of dermatomycosis described below in humans can affect absolutely any area on the body. They have several stages of development:
- The appearance of a rash on the epidermis in the form of circles.
- In the center, the area becomes lighter - this is the focus of the rash.
- The rash becomes moist and crusts begin to form.
- Severe peeling occurs around the circumference of the light area, and the patient is haunted by painful itching.
- The lesion takes on a healthy appearance, with a dark circle remaining around it.
Signs of tinea pedis depend entirely on the form of the disease. Thus, the dyshidrotic type of pathology is characterized by the appearance of a huge number of small blisters on the fingers and feet themselves, which subsequently open, forming areas of erosion. The latter are also characteristic of the intertriginous type of disease, but it is also accompanied by swelling and cracks. Symptoms of the squamatous form proceed as follows:
- primary lesion of the skin of the fingers;
- slight peeling, not accompanied by any other manifestations;
- worsening peeling, itching, formation of papules turning into erosions;
- suppuration of foci;
- the appearance of flakes of dead skin on the side of the foot;
- fusion of rashes, severe dryness, pain.
Ringworm affects the groin area, and then can spread as a result of self-infection to the folds of the body (under the breasts, etc.). Primary rashes appear on the inguinal folds, gradually spreading to the perineum, thighs, and anus. When the stage of the disease progresses to peeling, erosions begin to open, which is often complicated by pyoderma. The inflammation subsides, but relapses almost always occur, since fungi remain on the skin for a long time.
Dermatomycosis of the nails is also called onychomycosis. After suffering from the disease, the nail collapses and peels off. At the very beginning, the nail thickens and becomes deformed.
Photo of dermatomycosis in humans
In the photo you can see various manifestations of dermatomycosis in humans:
Depending on the symptoms of ringworm, treatment for a person will also differ. Accurate diagnosis is necessary.
Diagnostics
The diagnosis is established on the basis of anamnesis, clinical picture, and laboratory test results. When treating elderly patients, the possible interaction of systemic antimycotic drugs with chronically taken medications should be taken into account.
Before making a diagnosis, it is not recommended to treat the affected areas of the skin with antiseptic solutions, as this can blur the clinical picture and lead to a diagnostic error.
During microscopy of biological material taken from lesions (epidermal scales, hair, horny masses from the nail bed, etc.), mycelium, hyphae or spores of the pathogen are detected. Sowing scrapings from the affected area on nutrient media (universal and selective) allows you to identify the infectious agent and determine its sensitivity to antifungal drugs. Laboratory determination of antibodies to the pathogen in the patient's blood may be required.
An informative method for diagnosing some dermatomycosis is to examine the skin under a Wood's lamp - a greenish-blue, reddish, brown or golden-yellow glow of scales in the affected areas is revealed.
Before prescribing systemic therapy for dermatomycosis, especially for elderly patients, a general blood and urine test, a biochemical blood test (liver transaminases, bilirubin, creatinine), as well as an ultrasound examination of the abdominal organs and kidneys, and electrocardiography are prescribed. This allows us to identify patients for whom systemic therapy is contraindicated.
Differential diagnosis is carried out with psoriasis, eczema, neurodermatitis, vitiligo, seborrhea, syphilitic leukoderma.
When is specialist help needed?
Consultation with an experienced doctor is necessary if you notice:
- Cracking and peeling of the skin of the foot.
- The appearance of watery blisters.
- Infection with a bacterial infection, that is, swelling, redness, pain, increased temperature of this area of the foot. And also the discharge of pus, the appearance of red stripes, an unclear increase in body temperature.
- Spread of fungal infection.
- Parallel diseases in which blood flow is impaired or diabetes mellitus.
- Signs of the disease are not eliminated by antifungal therapy after two weeks.
How to treat ringworm
Treatment tactics for dermatomycosis in humans should be selected individually for each patient. The dermatologist takes into account the following factors:
- type of fungus;
- course of the disease;
- age;
- general health.
The main method of treating dermatomycosis is the prescription of antifungal agents for external or internal use. Without the use of such drugs, it is impossible to achieve recovery for the patient.
Drug treatment
Pharmacists have developed more than a hundred drugs with antifungal effects. Only a specialist can correctly select them for a specific patient. Medicines include:
- External agents (ointments, creams, spray, gels). They are applied twice a day, only to clean skin, otherwise they will not be able to penetrate deep into the skin and begin to work. The course lasts on average 10 days, the first positive results appear on the 4th day. Popular drugs include Miconazole, Ketoconazole, Mycoseptin, sulfuric and salicylic ointment.
- Antiseptics for treating wet areas - Chlorhexidine.
- Antihistamine medicine – Suprastin.
- Antimicrobial agents. Used internally in severe, advanced cases, and only as prescribed by a doctor - Griseofulvin.
- Vitamin preparations. Accelerate healing processes.
The exact treatment regimen is selected by a specialist. The main thing to remember is that mycosis must be treated for a long time. On average, therapy takes about two weeks, but it is recommended to continue using the remedy prescribed by your doctor for another week after the symptoms disappear.
Treatment with drugs
Medicines are used topically, orally or in combination. These agents have an antimycotic (antifungal) effect.
Well proven:
- Miconazole,
- Fluconazole,
- Diflox,
- Difluzol,
- Irunin.
These drugs are available in various forms: ointments are applied to the affected areas, capsules are taken orally, and shampoos effectively fight ringworm on the head.
Complex treatment (taking oral medications + using ointments) effectively eliminates this pathology. If you become infected from a pet, take it to the vet. This way you will avoid a relapse of the disease, because fungal colonies are resistant to chemicals and have adapted to survive in an unfavorable environment.
The duration of the course of treatment and dosage will be prescribed by your attending physician, after an accurate diagnosis has been established. During treatment, limit or eliminate any contact with other people.
Prevention
Prevention of the disease mainly concerns compliance with hygiene standards that exclude infection (including self-infection) with a dangerous fungus. Here are the recommendations given by experts:
- You cannot use other people’s towels and combs;
- You should have wet wipes with you (at work, while traveling) to keep your hands and face clean;
- after swimming in the sea, pool, bath, the skin between the toes should always be wiped;
- do not wear tight clothes and underwear, preferring a loose fit;
- do not touch stray animals, and regularly show pets to the veterinarian.
Remember that when the first signs of dermatomycosis appear, you should immediately contact a dermatologist. Only a doctor can prescribe effective treatment, and you can get rid of these unpleasant diseases forever.
Preventive measures
In order to protect yourself from such an unpleasant disease as dermatomycosis of smooth skin, it is very important to follow some preventive requirements. Let's look at what exactly experts recommend doing in order to protect yourself from contracting such a dangerous disease:
— Carry out all work around the house, as well as in the garden, using protective gloves.
- Be sure to take care of the skin of your feet. Remember to cleanse this part of your body daily. Also use various care products that contain antibacterial components.
- Never use someone else’s shoes or clothes, even if you trust the person who wore them one hundred percent.
— Buy only comfortable shoes that fit, made from natural fabrics.
- Monitor the health of your pets. After handling them, be sure to wash your hands with antibacterial soap.
- Be sure to normalize your diet. Your body must receive enough nutrients. Only in this case will your immune system work without interruption.
— And, of course, watch your personal hygiene when visiting public places such as saunas and swimming pools. An incredible number of bacteria live in places of high humidity, so the chances of getting infected increase many times over.