In children under ten years of age, the disease “viral pemphigus” occurs quite often. It is infectious and, as can be easily determined by its name, is of a viral nature. It is transmitted from sick children by the healthy Coxsackie virus, one of the types of enteroviruses.
Typically, the disease develops in a mild form with minor symptoms, but without proper treatment, long-term complications may appear, especially in a small child. Outbreaks of the disease often occur in the off-season, since frost and heat can destroy the virus.
What is pemphigus and the causes of the disease in children?
The disease viral pemphigus is a viral infection of the body, as a result of which blisters appear on the skin, which can be either small in size or, together with other formations, cover most of the body.
Viral pemphigus also tends to appear on the mucous membranes; the formation contains a cloudy liquid inside.
A child can become infected in public places, after which he can remain a carrier of the virus for some time and infect others.
The disease can occur for the following reasons:
- Weakened immunity;
- Use of medications;
- Congenital pathology;
- Hormonal imbalances;
- Incorrect personal hygiene of the child;
- Poor nutrition, which does not provide the body with all the necessary vitamins;
- Metabolism problems;
- Diseases of the nervous system.
The disease is caused by the Coxsackie virus, which has the property of quickly infecting the body and causing unpleasant symptoms similar to a cold.
Prevention
Contact between healthy children and a sick child must be completely avoided. A sick child should have his own dishes, a separate bed, and a personal towel. Toys must be disinfected; It is necessary to ventilate the room more often and carry out wet cleaning in it. Be sure to treat the rash only with gloves; after bowel movements, use antiseptic soap to wash the baby.
It is important to teach children to observe the rules of personal hygiene. And the most reliable prevention of this viral disease will be hardening the baby and other actions to strengthen the immune system. Then he will not be at risk of re-infection with pemphigus or other infectious diseases.
Routes of transmission
This type of viral disease can be contracted in almost any public place.
The most common methods of infection with viral pemphigus are:
- Airborne droplets - most often when visiting public places such as kindergartens and schools;
- Through contact with household items that have previously been touched by an infected person.
Thus, it should be noted that short-term contact of a healthy child with an infected person can cause infection with viral pemphigus.
Children especially often become infected with viral pemphigus in the absence of necessary food processing and failure to wash their hands after visiting the street.
How to recognize pemphigus: signs
Pemphigus of newborns develops towards the end of the first - beginning of the second week of a child's life. Most often, the disease manifests itself on days 3-5-10 after birth, but can develop earlier or later.
Blistering formations appear on the child’s body, which is how the disease got its name. They are filled with translucent yellow-gray contents, which soon turn purulent. The blisters initially measure on average 2-5 mm, but as they progress they can increase to several centimeters in diameter. Soon they begin to burst, leaving ulcers and erosions (bright red) in their original place, causing severe itching and anxiety in the sick child. At this time, new “fresh” bubbles may appear.
The areas where the blisters are located may appear inflamed, meaning the skin becomes red. But it also happens that blisters are located on unchanged areas of the skin. Usually they are grouped into multiple clusters and merge with each other, but single purulent formations can also occur.
First of all, the areas around the navel, lower abdomen, arms, skin folds are affected, and then the rash spreads to the entire skin: chest, back, buttocks, legs. With a rapidly progressing form of the disease, blisters form on the palms of the hands and soles of the feet (which is rare), as well as on the mucous membranes of the genital tract, nasal passages and eyes.
There may be no other accompanying symptoms of the disease, but often there is an increase in the child’s body temperature to 38 ° C or higher, general malaise, anxiety, lack of appetite and loss of body weight. In severe cases of the disease, a blistering rash affects the entire body, which becomes covered with red spots and ulcers. One of the most severe forms of pemphigus, when in just a couple of days the body is completely covered with inflamed erosions, is Ritter's exfoliative dermatitis, which very often ends in purulent inflammation of cells (phlegmon) or blood poisoning (sepsis), which poses a great danger to the life of the baby. In severe cases of the disease, vomiting, tachycardia, rapid breathing and difficulty breathing in the child may appear. As complications of pemphigus, otitis media, pyelonephritis, and pneumonia can develop.
Symptoms of viral pemphigus in children
The disease in children most often manifests itself with the following symptoms:
- Formation of specific blisters on the epidermis that contain liquid;
- Cough;
- Redness of the throat;
- Formation of wounds and blisters on the mucous membranes;
- Runny nose;
- Weakness;
- Lack of appetite;
- The child becomes passive and constantly sleeps;
- Sharp weight loss;
- High body temperature.
Most often, the first affected areas in the form of blisters form on the mucous membranes of children. However, blisters may occur on the arms, legs, face, and body.
At a complex stage of development of viral pemphigus in children, blisters and serous fluid may appear on the palms of the hands.
Features of the disease
Pemphigus has many subspecies. The leaf-shaped form of the disease has such a specific name due to the fact that multi-layered crusts appear on the dermis. Their appearance is similar to stacks of sheet material. These layered crusts appear on top of the erosions that formed after the blisters.
Pemphigus foliaceus occupies only about 1.5% of the total number of dermatoses.
This dermal lesion is the most common form of pemphigus that dermatologists see in children. As for adult patients, in them this pathology prevails in frequency over the vegetative type of pemphigus.
Pemphigus foliaceus in humans (photo)
Forms of viral pemphigus
There are certain forms of development of viral pemphigus in children, which can be accompanied by various symptoms and require compliance with certain features during treatment.
Pemphigus vulgaris
This form of viral pemphigus most often manifests itself as blisters, which, if damaged, can form ulcers.
It is observed in children in the following locations, such as the arms (especially the armpit area), abdomen, mucous membranes, face, thighs.
This form of viral pemphigus has the following features:
- The blisters are large in size and can, when combined, occupy large areas of the epidermis;
- The blisters quickly become damaged and form wounds, which gradually turn into crusts and cause a feeling of itching;
- Very often, wounds do not heal well and can become inflamed. As a result, swelling of the skin appears and ichor is released;
- Affects the oral cavity, as a result of which the child cannot eat food normally;
- When pressing on the blister, severe pain and burning may occur.
When this form of the disease occurs in children, the following unpleasant symptoms are observed:
- The appearance of blisters;
- Itching, resulting in the formation of sores;
- Feeling thirsty;
- Increased body temperature;
- The formation may have a specific odor;
- Cough;
- Runny nose;
- A sore throat.
The lack of timely treatment for this form of viral pemphigus can lead to the fact that most of the body is covered with a crust that constantly bleeds and itches. As a result, an infection is introduced into the damage and an inflammatory process is formed.
Seborrheic pemphigus
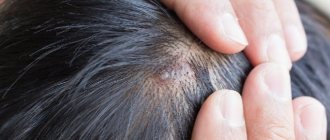
One of the severe forms of viral pemphigus, which is most often localized in the scalp of the body in children and is accompanied by a large number of symptoms.
Seborrheic viral pemphigus has the following features:
- Appears in the form of bubbles in the area of hair growth;
- Has the ability to quickly spread throughout the body;
- The blisters quickly become damaged and form crusts, which most often bleed;
- The wounds that exist under the crust can secrete clear liquid for a long time and bother the child.
Symptoms of seborrheic viral pemphigus are as follows:
- Increased body temperature;
- Itching in the area of hair growth;
- Increased sweating;
- Lack of appetite;
- Restlessness;
- Cough.
This form of pemphigus is difficult to treat in children, since it is difficult to treat the bubbles in the area of hair growth without damaging the blister itself. As a result, children experience itching and scratching of blisters.
Pemphigus foliaceus
Refers to a form of viral pemphigus that occurs in rare cases. Appear as a large number of small blisters, which quickly become damaged and form a continuous wound. Most often it forms on the face and abdomen in children.
The leaf-shaped form of viral pemphigus has the following features:
- It can form in almost any area of the body;
- It spreads only to the layers of the epidermis, while the mucous membranes do not become infected;
- Most often transmitted through touch and poor hand hygiene;
- The scabs that cover the wound may peel and crack, resulting in bleeding;
- Only the upper layers of the epidermis are damaged.
Viral pemphigus foliaceus manifests itself with the following symptoms:
- The appearance of small bubbles;
- Increased body temperature in children;
- Formation of a wound at the site of a blister;
- Dry and flaky skin in children;
- The presence of a specific odor.
With this type of viral pemphigus, a purulent discharge from the wound is very often observed, and painful sensations may form when touching the damaged area.
Pemphigus vegetans
This type of viral pemphigus can manifest itself as normal, gradually turning into another form. Most often it begins to manifest itself in the oral cavity and gradually moves to other parts of the body.
This form has the following features:
- Very often the places of formation are the armpits, groin area and behind the ears;
- After damage to the bladder, purulent erosion appears, which has a specific odor;
- The blisters tend to merge into one focus and form a wound with purulent discharge;
- This form of viral pemphigus can last for a long time, periodically disappearing and appearing again.
Pemphigus vegetans has the following symptoms:
- The appearance of itching in children;
- A sharp increase and decrease in body temperature;
- Headache;
- Lack of appetite;
- The largest number of blisters appears in the folds of the skin;
- Lesions most often appear in a specific location and slowly spread to healthy areas.
Very often, this form of viral pemphigus can transform into another, while the symptoms of the disease do not disappear, but only accumulate.
Enteroviral pemphigus
Many experts do not distinguish this form as a separate one, since enteroviral pemphigus combines the features and symptoms of all forms of the disease. Appears most often in children under 10 years of age.
Has the following features:
- The palms and feet of children are affected;
- Affects the oral cavity and can form in almost any part of the body;
- The bubbles form an elongated shape and can be of different sizes;
- When touching the bubbles, pain appears;
- An inflamed red line may appear around the blisters;
- If the bladder is damaged, purulent discharge from the wound may appear.
The following symptoms should be highlighted in children:
- Feeling overwhelmed;
- Fever;
- Itching and burning;
- Lack of appetite;
- Headache;
- Sleep disturbance;
- Lethargy;
- Cough.
The enteroviral form of viral pemphigus is a complex type of disease and requires correct diagnosis of the disease. It is almost impossible to independently determine the disease, which very often leads to complications.
There is another form of pemphigus, the Brazilian one, but this form does not appear on the European continent and often occurs in a mild form that does not require treatment.
Clinical case of pemphigus vulgaris in old age
True pemphigus is one of the most serious diseases. It accounts for 0.7 to 1% of all skin diseases [1, 4]. According to the regional dermatovenerological dispensary in Astrakhan for 2014, only 9 patients with pemphigus were treated as inpatients. Pemphigus can occur at any age. Most often, women over 40 years of age are affected; in recent years, cases of the disease among young people aged 18 to 25 have become more frequent. The most severe course is observed between the ages of 30 and 45 years [1, 4]. Pemphigus (acantholytic, or true, pemphigus) is an autoimmune disease characterized by the appearance of intraepidermal blisters on apparently unchanged skin and/or mucous membranes. The characteristic morphological basis is suprabasal blisters with acantholysis [4, 7, 8]. The etiology of pemphigus still remains unknown [1]. Currently, the leading role of autoimmune processes that develop in response to changes in the antigenic structure of epidermal cells under the influence of various damaging agents is recognized. Cell damage is possible as a result of chemical, physical, and biological factors [4]. It was found that in pemphigus, autoantibodies are directed against the surface structures of epidermal cells - keratinocytes. The binding of autoantibodies (pemphigus IgG) to glycoproteins of cell membranes (pemphigus antigens) of keratinocytes leads to acantholysis - impaired adhesion between cells and the formation of blisters. It has been shown that the complement system and inflammatory cells are not involved in this process, although the presence of complement enhances the pathogenicity of autoantibodies, and infection in areas of skin damage leads to the addition of an inflammatory process, which aggravates the patient’s condition [6]. Risk factors for the development of true pemphigus may include various exogenous and endogenous factors (including genetic predisposition). HLA-DR and HLA-DQ polymorphisms have been shown to be the basis of genetic predisposition to pemphigus (and other autoimmune diseases) [4, 6].
There are four clinical forms of true pemphigus: vulgar (ordinary), vegetative, foliate and erythematous (seborrheic). All clinical varieties are characterized by a long-term chronic wave-like course, leading in the absence of treatment to a disturbance in the general condition of the patients. Pemphigus vulgaris is the most common (up to 80% of all cases) [4]. In more than 50% of cases, the disease begins with damage to the mucous membranes of the oral cavity and pharynx. Small flabby blisters with serous contents that appear on unchanged mucous membranes, initially single or few in number, can be located in any area. Over time, their number increases. The blisters quickly (within 1–2 days) open, forming weeping, painful erosions with a bright red bottom or erosions covered with a whitish coating, bordered along the periphery by fragments of whitish epithelium. With further intensification of the erosion process, they become numerous, increase in size and, merging with each other, form foci of scalloped outlines. Patients experience pain when eating, talking, or swallowing saliva. A characteristic symptom is hypersalivation and a specific putrid odor from the mouth. If the larynx and pharynx are affected, the voice may be hoarse. For a long time, patients are observed by dentists or ENT doctors for stomatitis, gingivitis, rhinitis, laryngitis, etc. Damage to the mucous membranes can remain isolated from several days to 3–6 months. and more, and then the skin of the torso, limbs, and scalp is involved in the process.
Skin damage begins with the appearance of single blisters, then their number increases. The blisters are located on an unchanged, less often on an erythematous background. They are small in size, have a tense tire and serous contents. After a few days, some blisters on the skin dry out into yellowish crusts, or when the tire ruptures, bright red erosions may be exposed, releasing a thick exudate. Erosions at this stage of the disease are not painful and quickly epithelialize. The general condition of the patients remains satisfactory. The rashes that have regressed are replaced by new ones. This initial phase can last from 2-3 weeks. up to several months or even years. Then comes the generalization of the process, characterized by the rapid spread of rashes over the skin and the transition to the mucous membranes of the oral cavity and genitals, if they were not previously affected. As a result of eccentric growth due to exfoliation of the upper layers of the epidermis, the blisters increase in size, the tire becomes flabby, and the contents become cloudy or purulent. Under the weight of exudate, large blisters can take on a pear-shaped form (“Sheklakov’s pear syndrome”). The blisters spontaneously burst with the formation of extensive eroded areas of the skin. Erosions in pemphigus vulgaris are usually bright pink in color with a shiny, moist surface. The peculiarity of erosions is a tendency to peripheral growth, while generalization of the skin process with the formation of extensive lesions, deterioration of the general condition, the addition of a secondary infection, the development of intoxication and, in the absence of treatment, death are possible [1–5]. An important diagnostic sign of pemphigus vulgaris is Nikolsky’s symptom: detachment of the apparently unchanged epidermis when pressing on its surface near the bubble or even on apparently healthy skin far from the lesion [1]. There are three variants of Nikolsky's symptom, which allow us to assess the prevalence of acantholysis. In the first case, when the tire of a burst bladder is pulled, the epidermis peels off beyond its borders. In the second option, the upper layer of the epidermis peels off, and an erosive surface is formed if healthy skin is rubbed between two blisters. The appearance of erosion after rubbing healthy skin in a place near which there are no bullous elements indicates the presence of the third variant of Nikolsky’s symptom [5]. A modification of Nikolsky's symptom is the Asbo-Hansen phenomenon: finger pressure on the tire of an unopened bladder increases its area due to further stratification of the acantholytically altered epidermis with vesical fluid. In the initial phase of pemphigus vulgaris, Nikolsky’s symptom is not always detected, and even then only in the form of a marginal one. When the process is generalized, it is positive in all patients in all modifications [3]. Diagnosis of true pemphigus is based on the totality of the results of clinical, cytological, histological and immunological examination. The clinical picture of the disease, the presence of a positive Nikolsky symptom and its modification, the “pear” phenomenon described by N.D. are taken into account. Sheklakov, which are based on the phenomenon of acantholysis. Cytological examination reveals acantholytic cells (Tzanck cells) in impression smears from erosions and blisters after staining using the Romanowsky-Giemsa method (Tzanck test). The presence of Tzanck cells in the blisters is not pathognomonic, but a very important diagnostic sign of the disease.
Histological examination reveals the intraepidermal location of cracks and blisters [1, 4]. A necessary condition for a qualified diagnosis of true pemphigus is an immunofluorescence study. By means of indirect immunofluorescence, antibodies against components of the epidermis are detected when treated with luminescent anti-IgG human serum. Using direct immunofluorescence, IgG antibodies are detected in skin sections, localized in the intercellular spaces of the spinous layer of the epidermis [1]. Laboratory data (anemia, leukocytosis, increased ESR, proteinuria, hypoalbuminemia, decreased sodium excretion in urine, etc.) play a certain supporting role, allowing one to assess the severity of the process [3]. Differential diagnosis is carried out with Lever's bullous pemphigoid, Dühring's dermatitis herpetiformis, chronic benign familial pemphigus Gougereau-Hailey-Hailey, lupus erythematosus, seborrheic dermatitis, Lyell's syndrome, chronic pyoderma vegetans [4].
Treatment of true pemphigus has so far caused great difficulties. Since the main links of pathogenesis are interpreted from the standpoint of autoimmune pathology, all existing therapeutic measures are reduced to immunosuppressive effects on autoallergic processes through the use of corticosteroid and cytostatic drugs [1]. The introduction of corticosteroids into the treatment of pemphigus reduced mortality among patients from 90 to 10% [6]. Pemphigus is one of the few diseases in which corticosteroids are prescribed for health reasons, and existing contraindications in these cases become relative. The positive effect of glucocorticoids is explained primarily by the blockade of key stages of the biosynthesis of nucleic acids and proteins, shutdown of the afferent phase of immunogenesis, reduction of lymphoid organs, destruction of medium and small thymic lymphocytes, and inhibition of the formation of immune complexes. It is also believed that corticosteroids have a stabilizing effect on lysosome membranes and inhibit the synthesis of autoantibodies [1]. Typically, pemphigus vulgaris and pemphigus foliaceus are the most severe, therefore, for these clinical forms, the highest doses of glucocorticosteroids are prescribed (from 60–100 to 150–300 mg/day of prednisolone equivalent) [1,4]. The dose of prednisolone is selected taking into account the prevalence of the rash and the severity of the disease. It should be at least 1 mg/kg/day. The daily dose is distributed in such a way that 2/3 falls in the early morning hours (preferably after meals), and 1/3 in the afternoon (12–13 hours). If the patient’s condition is particularly severe, higher doses of prednisolone are prescribed – up to 300 mg/day [4]. At high doses, prednisolone can be partially replaced by parenteral administration or betamethasone (it is possible to use prolonged forms once every 7-10 days). Long-term use of corticosteroid drugs leads to the development of serious complications and side effects, and if they are quickly discontinued, the so-called withdrawal syndrome occurs, and the disease recurs. Therefore, it is necessary to correct and prevent side effects caused by long-term use of glucocorticosteroids. In order to prevent withdrawal syndrome, it is recommended to stop taking medications or reduce their daily dose carefully and gradually. Initially, a reduction in the dose of glucocorticosteroids is possible by 1/4–1/3 of the maximum initial dose after achieving a clear therapeutic effect (cessation of the appearance of new blisters, active epithelization of erosions), which usually occurs after 2–3, sometimes after 4 weeks. Then the dose of prednisolone is gradually, slowly, over several months, reduced to maintenance. The daily dose of the hormone is gradually reduced, approximately once every 4–5 days by 2.5–5 mg of prednisolone until the minimum maintenance effective dose of the corticosteroid is reached, the administration of which ensures remission of the disease.
In the future, a maintenance dose of corticosteroids is recommended to be administered alternately. However, periodically (every 4–6 months) it should be reduced by 2.5 mg prednisolone equivalent. Thus, by reducing the maintenance dose, it is possible to reduce the amount of hormone administered by 3-4 times compared to the initial maintenance dose. The maximum permissible minimum maintenance dose can vary from 2.5 to 30 mg/day. Typically, patients with pemphigus receive glucocorticosteroids for life, and sometimes their use can be abandoned [1, 4]. The addition of second-line drugs to therapy is indicated to increase the effect of treatment, reduce the side effects of corticosteroids, and also to prevent relapses during their gradual withdrawal. Adjuvant therapy includes azathioprine, methotrexate, cyclophosphamide, mycophenolate mofetil, intravenous immunoglobulin and dapsone [8]. The combined use of cytostatic and immunosuppressive drugs with corticosteroids allows one to achieve good therapeutic results in a shorter time and with lower daily doses of corticosteroids. Many drugs, such as alkylating agents and antimetabolites, have cytostatic properties. Of the alkylating agents, cyclophosphamide is the most widely used in the treatment of pemphigus. This drug is capable of entering into alkylation reactions with certain groups of proteins and nucleic acids of the cell, inhibiting various enzyme systems and dramatically disrupting the vital activity of cells, primarily highly active and lymphoid ones. Antimetabolites, which include purine base antagonists (azathioprine) and folic acid antagonists (methotrexate), resemble the structure of natural cell metabolites and, by competing with them, disrupt intracellular metabolism. The consequence of this is the accumulation of substances toxic to cells, leading to the death of cells, primarily actively proliferating ones. Azathioprine is prescribed at a dose of 1.5–2 mg/kg/day in 2–4 divided doses in combination with steroids. Methotrexate is administered intramuscularly at 10–20 mg (with good tolerance up to 25–30 mg) 1 time per week (for a course of 3–5–8 injections). Cyclophosphamide is administered orally at 100–200 mg/day, the duration of therapy is determined individually. During treatment, monitoring of blood tests (general and biochemical) and urine is necessary.
If the therapeutic effectiveness of glucocorticosteroids is insufficient and there are contraindications to the use of cytostatics, immunosuppressants are prescribed. Cyclosporine A for the treatment of patients with true pemphigus is used in combination with corticosteroid drugs, and the daily dose of corticosteroids is reduced by 3-4 times and corresponds to 25-50 mg of prednisolone equivalent. The daily dose of cyclosporine A in the complex therapy of patients with true pemphigus in the acute stage should not exceed 5 mg per 1 kg of the patient’s body weight and averages 3–5 mg/kg/day. This takes into account the clinical picture, severity and prevalence of the disease, the patient’s age, and the presence of concomitant diseases. For the first 2 days, to assess the tolerability of the drug, cyclosporine A is prescribed in half the dose, subsequently the daily dose is divided into 2 doses - morning and evening with an interval of 12 hours. The daily dose of cyclosporine A begins to be reduced after intensive epithelization of existing erosions. Typically, a loading dose is taken on average for 14–20 days, followed by a gradual reduction in the daily dose of the drug to 2–2.5 mg per 1 kg of the patient’s body weight. Complete cleansing of the skin should not be considered the final goal of treatment. After achieving remission, the patient should continue to take the minimum effective maintenance dose of cyclosporine A, which should be selected individually. At this dosage, the drug can be used for a long time (2–4 months) as maintenance therapy. Currently, treatment with immunosuppressants is not generally accepted [1, 4]. Aniline dyes, corticosteroid creams with an antibacterial or antimycotic component, and aerosols are used locally [3]. For additional treatment of pemphigus, extracorporeal detoxification methods (hemosorption, plasmapheresis) are successfully used [1]. Despite the successes of domestic and foreign researchers in clarifying the mechanisms of pathogenesis and improving treatment methods for patients with true pemphigus, the problem of pemphigus remains relevant and is due to the severity of the disease, its incurability and potential mortality [1].
We present a clinical case demonstrating the difficulties of differential diagnostic search when diagnosing pemphigus. Patient Zh., born in 1945, has been ill since the fall of 2014, when rashes first appeared on the scalp. I treated myself, used ointments with antibiotics without effect. In May 2015, an exacerbation of the skin process began. The rash has spread to the face and torso. He was observed in the clinic at his place of residence, and due to the torpidity of treatment, he was sent to the regional oncology clinic, where a pathohistological examination of the scalp was carried out. After examination, a diagnosis was made: multiple scalp cancer. Т1N0М0. Radiation therapy is recommended. Within 2 weeks. the process on the skin has spread significantly: elements have appeared on the chest, back, and upper limbs. Serous-purulent discharge was noted on the scalp, and the erosions took on a draining character. Taking into account the change in the clinical picture, he was sent for consultation to the regional dermatovenerological clinic with a diagnosis of pemphigus vulgaris. As a result of examination in the department, this diagnosis was clinically and laboratory confirmed. At the same time, pathohistological preparations were reviewed at the oncology clinic, and the diagnoses of cancer and basal cell carcinoma of the scalp were removed as erroneous. From the anamnesis it is known that the patient has a burdened premorbid background. In 2012, he suffered a small-focal myocardial infarction. Suffering from chronic bronchitis. Upon examination, a widespread pathological process was revealed. On the skin of the scalp, face, neck, torso and upper extremities there were multiple bright red erosions with serous and serous-purulent discharge. Some of the erosions were covered with dense crusts of gray-yellow color (Fig. 1–3). On an erythematous background, there were blisters of various sizes with a flabby cap and cloudy contents. Nikolsky's symptom is positive. During a laboratory examination, smears from blisters on the forearms revealed single acantholytic cells in a specimen with coarse nuclei. Epithelial cells with signs of atypia (enlarged coarse nuclei, binucleate cells) up to 8–10–12 per field of view were identified. During bacteriological examination of discharge from erosions, staphylococcus was isolated. According to the pathomorphological study, the morphological picture of pemphigus was revealed - a bubble with serous fluid and acantholytic cysts with purulent inflammation along the periphery was found in the epidermis. When reviewing the drugs at the oncology center, the morphological picture of pemphigus was confirmed and no tumor growth was detected. A general clinical examination showed an increase in ESR and a sharply positive C-reactive protein. Fibrogastroduodenoscopy revealed erosive antrum gastritis, erosive and ulcerative bulbitis and duodenitis. Small (up to 0.2 cm) acute ulcers of the bulb and the upper horizontal part of the bulb were found.
Taking into account the generalized process of skin lesions, parenteral administration of prednisolone at a dose of 90 mg was prescribed with a gradual transition to oral administration of the drug at a dose of 30 mg. He also received detoxification, antibacterial and antifungal systemic therapy and local treatment using antiseptics, reparatives and anti-inflammatory drugs. Due to the presence of erosive gastritis, erosive-ulcerative bulbitis, and also because of taking prednisolone, the patient was given antisecretory therapy. During therapy for 3 weeks. positive dynamics were noted. On the skin of the scalp, neck, chest, and back, erosions were completely epithelialized, and the crusts fell off (Fig. 4–6). He was discharged for outpatient treatment with recommendations to reduce the dose of prednisolone by 1/4 tablet every 7–10 days under the supervision of a dermatovenerologist at the place of residence.
The development of pemphigus in a 70-year-old man with a latent onset of the disease may have been the reason for late diagnosis and, consequently, untimely initiation of therapy. After correct interpretation of clinical and morphological data and complex therapy, a positive result was achieved.
Literature 1. Matushevskaya E.V. Pemphigus // Russian Medical Journal. 1997. No. 11. 2. Mordovtsev V.N., Mordovtseva V.V., Alchangyan L.V. Erosive and ulcerative skin lesions // Consilium Medicum. 2000. No. 5. 3. Paltsev M.A., Potekaev N.N., Kazantseva I.A., Kryazheva S.S. Clinical and morphological diagnosis and principles of treatment of skin diseases. Guide for doctors. M.: Medicine, 2010. 4. Kubanova A.A., Kisina V.I., Blatun L.A., Vavilov A.M. and others. Rational pharmacotherapy of skin diseases and sexually transmitted infections: A guide for practitioners / edited by. ed. A.A. Kubanova, V.I. Kisina. M.: Litterra, 2005. 882 p. (Rational pharmacotherapy: ser. handbook for practicing physicians; vol. 8). 5. Rubins A. Dermatovenerology. Illustrated guide. M.: Panfilov Publishing House, 2011. 368 p. 6. Svirshchevskaya E.V., Matushevskaya E.V. Immunopathogenesis and treatment of pemphigus // Russian Medical Journal. 1998. No. 6. 7. Kumar R., Jindal A., Kaur A., Gupta S. Therapeutic Plasma Exchange-A New Dawn in the Treatment of Pemphigus Vulgaris // Ind. J. Dermatol. 2015. Vol. 60(4). P. 419. doi: 10.4103/0019-5154.160509. 8. Quaresma MV, Bernardes-Filho F., Hezel J. et al. Dapsone in the treatment of pemphigus vulgaris: adverse effects and its importance as a corticosteroid sparing agent // An. Bras. Dermatol. 2015. Vol. 90 (3 Suppl. 1). R. 51–54.
Pemphigus in newborns
The manifestation of viral pemphigus in newborns occurs as a result of reduced immunity and damage to the body by the staphylococcal virus.
Viral pemphigus most often forms after the 20th day of a newborn’s life, since in the first days maternal immunity is still active, which reduces the risk of infection with pemphigus.
Causes of pemphigus in newborns:
- Weak immunity;
- Insufficient maternal hygiene;
- Infection during childbirth;
- Premature birth;
- Damage to the baby's skin.
Viral pemphigus disease is manifested by the following symptoms:
- Skin rashes;
- Peeling of the skin;
- Swelling;
- Inflammation of the umbilical cord;
- Wounds in places where a blister with liquid is damaged;
- Lack of appetite;
- Lethargy;
- Increased body temperature.
There are several stages of development of viral pemphigus in newborns:
- Erythematous stage - red spots appear on the skin with the release of colorless liquid;
- Exfoliative stage - manifested by the appearance of blisters in the arms, thighs and abdomen. It tends to pass quickly and does not require long-term treatment;
- Regenerative stage - blisters form on the newborn’s skin, which quickly become damaged and form small erosions.
Staphylococcal pemphigus is also isolated, which is formed as a result of the staphylococcus virus, which affects the skin.
Viral pemphigus in newborns is transmitted by airborne droplets and appears in children only through contact with an infected person.
Classification
Pemphigus vulgaris occurs due to autoimmune disorders. The mucous membrane of the mouth and lips is the first to be affected; the blisters are small, their surface is very thin. To confirm the diagnosis, a sample of fluid from the blister is taken for analysis. Watery blisters appear in the mouth, then the lesion spreads throughout the body.
It occurs in an acute form. The blisters can be large in size, and when opened, clear or bloody fluid flows out of them. As it dries, a brown crust forms. The disease can be triggered by a burn, an excess of ultraviolet radiation and a number of medications. The disease can last for several years. Traces of pigmentation remain at the affected areas. During the acute stage, the number of blisters increases.
Steroids may be prescribed. As a local treatment, doctors recommend products with a drying effect and ointment dressings. Pemphigus vulgaris is dangerous due to complications. If the outcome of treatment is unfavorable, the kidneys, liver and heart are affected. To avoid relapse, you should monitor your blood sugar levels, take vitamins and calcium.
Pemphigus leaf - the blisters are flat, with a thin surface; at the site of the rupture of the bubble, erosion occurs, which does not heal for a long time. Constantly appearing blisters form a large non-healing wound. The mucous membrane of the mouth is not affected in this form of pemphigus. New bubbles form under the crust.
Seborrheic is a type of leaf pemphigus. The rash appears in the form of small blisters, which dry out and become covered with yellow crusts. They are localized on the face, in the scalp and spread to the chest and back. After removing the scales, the surface of the lesion becomes wet. They appear very rarely on the mucous membrane.
Doctors associate this form with systemic lupus erythematosus, since the symptoms of the diseases are similar. It differs from others in that the lesions are symmetrical and erosion does not form in place of the bubbles. Seborrheic pemphigus can be confused with measles and rubella. For treatment, glucocorticosteroids in high dosages, immunosuppressive drugs, broad-spectrum antibiotics and plasmapheresis are prescribed.
Vegetative form. Blisters are localized in the genital area, in the armpit and on the head. The blisters burst, forming a purulent plaque. Then, in place of the blisters, the skin grows. Healing takes a long time, leaving a lump similar to a wart.
Benign familial chronic pemphigus Gougereau-Hailey-Hailey. Small blisters appear mainly on the neck, shoulder blades, armpits, and groin area. For treatment, antibiotics and corticosteroids are prescribed, and wounds are treated with alcohol. Treatment is usually effective.
Pemphigus of the eye. More common in older people. Damage to the mucous membrane of the eye leads to fusion of the eyelids with the eyeball and narrowing of the palpebral fissure. The disease can lead to blindness.
Determining the specific type of disease is necessary to prescribe a specific course of treatment. To treat certain types of the disease, it is necessary to use special drugs and regimens for their use. Pemphigus can develop in mild, moderate, severe or chronic forms.
Types of pemphigus:
- Leaf-shaped (bubbles on the child’s skin begin to burst, and crusts form in their place; the development of the pathological process causes them to be layered on top of each other).
- Viral form (blisters can appear on any part of the child’s body, their appearance is accompanied by a deterioration in the general condition of the little patient; the blisters resemble the symptoms of chickenpox).
- Seborrheic form (this type of disease is characterized by damage to the scalp, the general symptoms of the pathological process do not change).
- Vegetative form (the pathological process affects the mucous membranes of the mouth, lips, area around the nose or on the child’s genitals; a distinctive feature of this type of pemphigus is the formation of purulent crusts with an unpleasant odor).
Complications
If viral pemphigus is not treated correctly, the following types of complications may occur:
- Formation of a chronic form of the disease;
- Infection of wounds with discharge of pus;
- Malfunctions of internal organs;
- Meningitis;
- Development of pneumonia;
- Major weight loss;
- Possibility of spots and scars after treatment of the disease.
Pemphigus can cover a child's entire body and cause other types of skin diseases that make the viral infection worse.
Forecast
- If you make a diagnosis in time and determine the required dose of treatment, especially with regard to the amount of corticosteroids, then it is quite possible to avoid the tragic outcome of the disease.
- However, another danger arises. Once the rash has resolved and the erosions have healed, a lower dose of corticosteroids will be indicated for the rest of the patient's life. Therefore, there is a possibility of destruction of the patient’s body due to regular use of medications.
- Complications occur that affect the patient’s internal organs and entire vital systems.
- Long-term use of medications that inhibit the reappearance of pemphigus is dangerous because of its destructive ending—death.
Diagnostics
When the first symptoms of the disease appear, you must contact a specialist to undergo the necessary diagnostics.
Diagnostics is carried out using the following methods:
- Visual examination of the patient;
- Blood analysis;
- Study of the component of the bubble;
- Histological analyses;
- Stool analysis.
If a specialist observes the addition of additional types of infection to viral pemphigus, then additional tests may be prescribed.
Differential diagnosis
Ordinary pemphigus must be distinguished from the following diseases:
- Dühring's dermatitis;
- lichen planus (bullous form);
- toxidermy.
Pemphigus vegetans sometimes resembles condylomas lata, foliate - erythroderma, seborrheic - seborrheic dermatitis and impetigo. Only a dermatologist can carry out such a differential diagnosis.
Viral pemphigus
In children, a disease such as enteroviral tonsillitis, also called viral pemphigus or hand-foot-mouth syndrome, occurs quite often. Unlike true pemphigus, this disease is caused by Coxsackie viruses and enteroviruses. Is pemphigus caused by viruses contagious? Yes, the disease is easily transmitted from child to child.
Signs of the disease in children:
- True pemphigus is observed in adults, viral (infectious pemphigus) - mainly in young children.
- Viral pemphigus has a prodromal period, during which there is malaise, fever, and sometimes cough and loose stools.
- On the 2-3 day of illness, with the viral form, a rash appears on the palms, soles and oral mucosa. The blisters in the mouth are small, similar to stomatitis; after they are opened, small (up to 8 mm) separate painful erosions are formed, covered with a light coating. The mucous membrane around them is red. They disappear within a week from the onset of the disease.
- On the palms and soles, small (up to 4 mm) oval grayish blisters form, not rising above the skin, on a reddened base. A rash of various types may also appear on the buttocks, arms, legs: spots, blisters, vesicles.
Differences between chickenpox and pemphigus in children:
- Mild and moderate forms of chickenpox do not affect the palms and soles.
- Viral pemphigus very rarely occurs on the scalp.
- The blisters of chickenpox are soft, the skin underneath is of normal color; there may be an indentation in the center of the vesicle.
- With chickenpox, the blisters gradually turn into crusts, and new elements also appear; at the same time you can see different stages of development of the rash.
Is pemphigus contagious? Causes and symptoms of the disease in pregnant women and newborns:
Syphilitic pemphigus
Occurs in newborns and infants in the first weeks of life with congenital syphilis. The blisters are located on the palms and soles. They can be observed on the forearms and legs, as well as on the torso.
Epidemic pemphigus
May develop in the first few days of life in newborns. This is a purulent lesion of the superficial layers of the skin, which is widespread. The rash is located on the thighs, buttocks, limbs, near the navel and extremely rarely occurs on the palms and soles, which distinguishes it from the syphilitic form.
The blisters are multiple, filled with cloudy, often purulent contents, they are up to 2-3 cm in size and open with the formation of painful erosions. Crusts do not form; after a few days the erosions heal, leaving behind pink spots. After 7-10 days, a new wave of rashes appears, accompanied by fever and poor health of the child.
With a mild course, the blisters are single, turning into peeling of the skin without disturbing the baby’s condition. Any form of epidemic pemphigus is contagious.
Pemphigoid
Non-acantholytic forms include individual diseases - bullous and cicatricial pemphigoid. They are also accompanied by the formation of blisters, but without signs of acantholysis.
Paraneoplastic pemphigus
A rather rare condition that complicates the course of malignant lymphoma - a tumor of lymphoid tissue. It manifests itself in the formation of blisters on the mucous membrane of the oral cavity, less often in the area of the eyes and genitals. This form of the disease is difficult to diagnose, as it resembles acantholytic and non-acantholytic forms of pemphigus. When the lips and skin are affected, which is rare, the disease resembles polymorphic exudative erythema.
Diabetic pemphigus
Accompanied by the formation of bullae (large blisters) in people with diabetes, on the hands and feet, less often on the skin of the legs and forearms. In appearance they resemble burns. Such blisters are painless, they quickly dry out and disappear. This symptom of diabetes is caused by poor control of blood sugar levels.
Drug treatment of pemphigus in children
Treatment of this type of disease is most often carried out in several ways, depending on the cause of its occurrence.
There are several methods of treating viral pemphigus in children.
General therapy is necessary to eliminate the virus from the body and strengthen the immune system's resistance to other types of infections.
The most commonly prescribed drugs are:
- Antiviral agents - for example, Viferon rectal suppositories - are recommended to be used twice a day. The course of treatment is no more than 10 days. Allowed for use from 1 month of age. Average price 240 rubles ;
- Glucocorticosteroids are used individually for each child. The most commonly used is Dexamethasone, once a day before meals, for a course of no more than 3 days. Average price 150 rubles ;
- Cytostatics are necessary to block further spread of the disease. The most commonly prescribed drug is Sandimmune, used twice a day before meals for 5 days. Permitted age is over 6 years. Average cost 1300 rubles ;
- Antipyretics – Nurofen, used only if necessary depending on the child’s weight. Allowed to be used in the form of syrup from 3 months. Cost from 120 rubles .
Viferon Dexamethasone Sandimmune Nurofen
Local treatment is used to treat blisters, the most commonly used are:
- Antiseptics – Chlorhexidine, recommended for use on wounds twice a day for 5 days, allowed for use in children over 7 years of age. Average price 80 rubles , avoid contact of the drug with soap. An allergic reaction may occur. And also Miramistin, which can be used from a month of life, diluted with water in a 1:1 ratio. Cost from 240 rubles ;
- Combined antiseptic drugs - special talkers are used, which are made according to an individual prescription from the attending physician, depending on the complexity of the disease. On average, the cost of such talkers depends on the price of the components and can vary from 150 to 300 rubles :
- Antimicrobial drugs for the oral cavity - Orasept is used twice a day for 5 days. Can be used from the age of 3 years. The average price of the drug is 300 rubles . For children under 12 years of age, oral cavity treatment is performed by adults to prevent cases of overdose.
Chlorhexidine Miramistin Orasept
Physiotherapy - prescribed by the attending physician individually for each patient.
Provides for the following procedures:
- Electrophoresis;
- Electrical stimulation of the bladder;
- Magnetotherapy.
All types of physiotherapy methods are used for children older than one month, strictly under the supervision of the attending physician.
Treatment of pemphigus foliaceus
This form of the disease is treated using a variety of techniques, including both drug therapy and additional manipulations. The course of medications to be taken must necessarily consist of glucocorticosteroids: triamcinolone or prednisolone, metipred or dexamethasone. Sometimes it is necessary to supplement this set of drugs with immunosuppressive medications: methotrexate or azathioprine.
Experts note that a positive effect in treatment is achieved by combining corticosteroid drugs with synthetic drugs aimed at combating malaria. This could be delagil or plaquinil.
Separately, the patient is advised to use baths filled with a solution of a disinfectant or anti-inflammatory astringent.
Treatment with folk remedies
Folk remedies for the treatment of viral pemphigus are used at the beginning of the formation of diseases. And they help to quickly reduce unpleasant symptoms and improve the child’s condition.
However, all methods may have hidden side effects, so you should consult your doctor before use.
The most commonly used methods are:
- Nettle juice – helps reduce inflammation and has an antiseptic effect. It is necessary to chop the leaves and stems of fresh nettle and add a glass of water, let it brew for an hour. Strain, moisten cotton wool in the treated liquid and apply to the locations of the bubbles;
- Baths with a series - helps reduce discomfort and has the property of healing damage to the epidermis. To prepare, you need to pour two tablespoons of dry herbs with two glasses of boiling water and let it brew for 20 minutes. Add to water while bathing. Used from birth, in a course of two days;
- Mint and calendula flowers have the property of strengthening the immune system. To prepare, you need to mix a teaspoon of mint herb and a teaspoon of calendula flowers and pour a glass of boiling water. Give your child a tablespoon twice a day for 7 days. Recommended for use from the age of 3 years;
- Olive oil – has beneficial qualities for restoring the skin, it is recommended to use a cotton pad, apply a small amount to damaged areas and leave until completely absorbed. Allowed for use from the age of 6 months. Duration of treatment is 10 days.
Treatment
The only effective way to treat this disease is through the use of medications. As an auxiliary method, you can use a therapeutic one.
Therapeutic
Along with the use of medications, extracorporeal hemocorrection is prescribed. To purify blood, the following are most often used:
- plasmaphoresis;
- hemosorption.
Medication
Drug therapy involves the use of the following groups of drugs:
- corticosteroids (Prednisolone, Triamcinolone, Dexamethasone);
- cytostatics (“Cyclosporine”, “Methotrex”, “Azathioprine”).
Antibiotics are also needed in case of infection. In order to prevent complications that may arise as a result of corticosteroid therapy, it is necessary to take medications that have a protective function on the walls of the stomach (“Bismuth Nitrate”).