10.10.2018 When communicating with loved ones or patients, this topic is raised, you can often hear the following statements: “cancer developed after removing a mole,” “he removed a mole and died,” and so on. Every time these relationships are presented to me, my first question is: “Are there documents?”
Histological examination? Extracts from hospitals, CT, MRI, PET? But there are no documents. But for some reason we believe the storyteller, although 99% of such stories always reach us in the form of rumors, retellings, through third parties and are not at all supported by facts.
In this article, we'll take a closer look at where these stories come from, whether they have any basis in reality, and what the remaining 1% consists of.
Here are a few scenarios that may suggest that there is a connection between mole removal and death from cancer.
Is it possible to remove nevi (can moles be removed)
From the perspective of the likely development of skin cancer, removing any mole is completely safe
Often, wanting to remove one or more moles, people ask the question: “Is it possible to remove these moles and will this cause any harm?” This question is natural, since at the everyday level there is a widespread opinion that it is better not to touch moles. However, from the perspective of the likely development of skin cancer, removing any mole is completely safe. This means that removing a mole may not contribute to the development of skin cancer. Therefore, you can safely remove any mole that causes discomfort or creates a cosmetic defect. Any operations to remove moles are safe, since complications during their implementation are extremely rare and, in most cases, are associated with an allergic reaction to an anesthetic, bleeding, etc.
Reasons affecting the production of anti-cancer proteins
The production of protein P15 is reduced or stopped for completely everyday reasons. In many cases, patients are to blame for their problems themselves. Mole cancer is caused by:
- Intense UV exposure - abuse of sunbathing and solarium;
- Traumatization of a mole by clothing, jewelry, accessories, etc.;
- Unsuccessful “information” with celandine, vinegar and other means that cause chemical burns;
- Trying to get a chocolate tan while having fair skin that doesn’t tolerate the sun’s rays well;
- Abuse of products containing carcinogens.
- Smoking and other bad habits that reduce immunity.
Genetic factors for mole cancer cannot be excluded. Sometimes the cancer defense system is weak from birth. Such people have numerous cases of cancer in relatives.
Knowing about bad heredity, you must be careful, excluding negative factors that provoke cancer. Examination of moles and birthmarks for patients at risk is strictly necessary.
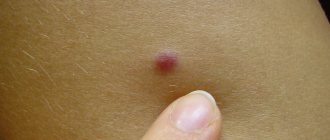
Which moles should definitely be removed?
Moles that look like skin cancer or have begun to actively change in recent months (grow, bleed, change color, shape, etc.) must be removed. Such moles should be removed as soon as possible in order to prevent possible tumor progression and the transition of the malignant pathological process to more severe stages.
At the same time, there is no need to remove all moles that are present on the body and cause any suspicion of their possible malignant degeneration in the future, since this is not rational and ineffective from the standpoint of preventing skin cancer.
Indeed, in most cases, skin cancer develops from a completely normal area of the skin, and not from a mole, the malignancy of which is extremely rare. Therefore, there is no need to remove all suspicious moles; it is better to leave them on the body and regularly visit a dermatologist for a preventive examination. In addition, you can remove any moles that do not satisfy a person for aesthetic reasons, that is, they create a visible cosmetic defect.
The second scenario is a doctor’s mistake (oncologist, dermatologist or surgeon)
A mole was removed without histology, and skin cancer (melanoma) developed at the site of removal.
In our country there is no law that prescribes that all removed skin lesions must be sent for histological examination. Therefore, a very large part of them is removed after a visual inspection - “by eye” - and sent to a waste container. This is where a tragic mistake can occur. If the doctor mistook skin cancer (melanoma) for a benign mole and removed it without histology and corresponding indentation, events unfold as follows:
- a recurrence of melanoma (skin cancer) develops at the site of removal;
- relapse grows more aggressively than the primary tumor and metastasizes early;
- after this, only 30% of patients have a chance to live five years or more [1].
Methods for removing moles (nevi)
Currently, moles can be removed using the following methods:
- Surgical removal;
- Laser removal;
- Removal with liquid nitrogen (cryodestruction);
- Electrocoagulation (“cauterization” with electric current);
- Radio wave removal.
The choice of a specific method for removing a mole is made individually, depending on the properties of the nevus. For example, it is recommended to remove ordinary brown moles surgically (with a scalpel), since only this method allows you to completely cut out all nevus tissue from the deep layers of the skin. A cancer-like mole should also be removed surgically, since this method allows for an inspection of the skin tissue and excision of all suspicious areas. All other moles can be removed with a laser or liquid nitrogen, which allow the manipulation to be carried out as carefully and bloodlessly as possible.
Mole removal - consequences of the procedure
Removing a mole is a very responsible procedure that requires special care for the operated area of skin after it is performed. There is absolutely nothing complicated about the care itself, the main thing is not to forget about it. Otherwise, unsightly scars may remain on the human body.
We recommend: In general, there is no particular need to remove moles, since initially they do not pose any danger. However, if they begin to degenerate into malignant tumors from benign ones, you should immediately contact a specialist.
In order to prevent skin cancer, it is necessary to very carefully monitor changes in those formations that already exist on the body, as well as the appearance of new ones. Of particular concern should be moles that increase in size and change their color (also the color of the border with the skin), marks with scales or a cracked surface, bleeding nevi or those from which fluid oozes. In addition, factors such as burning, itching or tingling in the area of the mole also indicate a malignant formation.
Cancer can be caused by a variety of factors, such as prolonged exposure to the sun or excessive use of tanning beds. Moreover, sealing moles with a band-aid or covering them with a Panama hat or a towel is not only useless, but even more harmful, since the greenhouse effect has an extremely negative effect on moles. Any trauma to a mole can also serve as an impetus for the development of cancer. If this happens, you must definitely contact a specialist. By the way, those who have a lot of marks on their body should also not use a hard sponge when taking a shower.
Complications after removal of a mole occur only if the wrong influence was exerted on it. Therefore, it is necessary to approach the choice of both the clinic and the doctor with special attention. Once the removal procedure is completed, you need to listen to what experts advise on further skin care. After removing a mole, the wound very quickly becomes covered with a dark crust, which must be protected from exposure to various gels, creams and even plain water.
Attention: Under no circumstances should the resulting crust be removed on your own, since within five days a new, rather sensitive area of skin will form under it. Forcible removal of the crust can lead to the formation of an unsightly scar in this area. As soon as it falls off on its own, there will be delicate pink skin in this place, which, of course, must be especially protected from ultraviolet radiation.
As a rule, it is impossible to say with perfect accuracy how long a mole will take to heal after removal - it all depends on the individuality of the body. This process lasts approximately twenty days, after which the skin may also experience some discomfort for two to three weeks. The smaller the mole, the faster the healing. You need to take care of the area of skin where the mole was located until the skin color is completely equalized.
The cause of oncology of birthmarks is protein P15
Research conducted in Philadelphia confirmed the theory that moles and birthmarks (nevi) on the human body are formed in the womb and are probably genetic in nature. This means that it is impossible to prevent their occurrence, at least with the current level of progress. But stopping the degeneration of tumors into cancer is quite possible.
According to American researchers, birthmarks turn into cancer when the P15 protein, responsible for destroying cancer cells, disappears. The creation of drugs based on the protein compound P15 will help defeat not only skin cancer, but also other malignant tumors.
Scientist Toddy Ridkey found that the appearance of moles is caused by a mutation in the BRAF gene, to which the body responds with increased release of the P15 protein, which inhibits the development of tumors. Its concentration in a normal mole is 140 times higher than in the skin of a healthy person. Having implanted skin cancer (melanoma) cells into experimental mice, scientists discovered that tumors grew only in animals with reduced levels of P15. In other cases, the body destroyed the malignant cells, and melanoma did not develop.
Caring for a removed mole
After removal of a mole, pain may appear in the wound area, which can be relieved with non-steroidal anti-inflammatory drugs
A few hours after removal of a mole, pain of varying degrees of intensity may appear in the wound area due to a violation of the integrity of the skin structures. These pains can be relieved by taking drugs from the group of non-steroidal anti-inflammatory drugs (NSAIDs), such as Paracetamol, Nurofen, Nimesulide, Ketorol, Ketanov, etc. The wound itself does not require any special care or treatment until the stitches are removed, which occurs on days 7–10. After this, to speed up healing and prevent scar formation, it is recommended to lubricate the wound with Levomekol, Solcoseryl or Methyluracil ointments.
Until the wound heals completely, so as not to provoke inflammation, infection and the formation of a rough scar, the following rules should be followed:
- Do not apply cosmetics to the wound;
- Do not pick or wet the crust;
- Cover the wound with a cloth or adhesive tape from exposure to sunlight.
Complete wound healing after surgical removal of a mole occurs within 2 to 3 weeks. When using other methods of mole removal, wound healing may occur somewhat faster. In rare cases, the wound after removal of a mole may become inflamed due to the entry of pathogenic bacteria into it, which will lead to longer healing and scar formation.
Signs of infection are as follows:
- Inflammation of the wound;
- The pain in the wound area became stronger;
- Pus in the wound area;
- Broken edges of the wound.
If the wound becomes infected, you should consult a doctor who will prescribe the necessary treatment. In rare cases, the sutures may diverge, causing the edges of the wound to diverge to the sides and slowly grow together. In such a situation, you should consult a doctor so that he can apply new stitches or tighten the existing ones.
Care after laser mole removal
If the laser destruction procedure was performed by a qualified specialist, the risk of side effects is minimal.
If the laser ablation procedure was performed by a qualified specialist, the risk of side effects is minimal, but the patient will also have to follow certain post-procedure rules, listed below.
- It is necessary to provide rest to the wound surface, without injuring it by friction of clothing or shoes, and also by taking care of the protective crust;
- Contact of the wound with water should be avoided for two weeks after manipulation;
- It is recommended to protect the skin surface from direct sunlight, and also use creams with a high UV protection factor. To the question of when you can sunbathe after removing a mole, the answer will be at least three weeks;
- You cannot use ointments, creams and gels for healing on your own without a doctor’s prescription;
- The procedure area should be protected from any mechanical damage, carefully protecting the integrity of the protective scab.
Laser removal is one of the simplest and least traumatic methods of mole destruction. Compliance with simple rules of rehabilitation will allow you to avoid scars, cicatrices and other unpleasant consequences and obtain an ideal physiological and aesthetic result.
Wound healing - misconceptions
Many people believe that the wound must be open during healing, as this will help speed up the process. In fact, this is not so, since the wound heals much faster if a bandage is applied to it and it is treated with a solution of brilliant green or potassium permanganate.
What to apply to the operated area after removing a mole before applying a bandage is a controversial issue. Depending on the size of the mole, as well as the removal methods used and other conditions, the patient may need the help of a specialist after the operation.
A visit to your doctor may be necessary to:
- undergo certain tests - a specialist must analyze the removed tissue, after which the patient is informed of the results of the study;
- remove sutures after surgery. They are removed on the fourth to seventh day on the face, depending on the type of thread and the area where the sutures are applied. On other parts of the body, sutures are removed on the eighth to twentieth day (depending on the surgeon’s recommendations);
- determine the necessary additional measures to prevent infection.
Important: You need to be very careful about the operated area, try to make sure that no dirt gets there. In addition, it is necessary to protect this area from any damage, pressure on it and heavy loads.
Symptoms that may bother you
There are, of course, post-operative symptoms that may be of particular concern to the patient. For example, what if a lump appears after a mole is removed? There is only one answer - again, turn to professionals for help. They must see this seal, feel it and then draw certain conclusions. Most often, such lumps are forming scar tissue, although it may be something more serious. In short, you should definitely contact a doctor for an examination if you have any questions, complaints or other reasons for concern. Only a specialist can actually determine whether these are serious reasons or imaginary ones.
It is also necessary to consult a doctor in cases where the scar after mole removal is very painful. Of course, any of the following symptoms requires an immediate visit to the doctor:
- bleeding or constant discharge of an unpleasant-smelling liquid from the wound;
- strong increase in temperature;
- acute pain that does not stop even when taking painkillers.
Do not: Taking ibuprofen or aspirin after surgery is prohibited, as they affect blood thinning, which increases the likelihood of bleeding. If taking these medications is absolutely necessary, the patient should definitely consult a doctor.
By the way, you need to be prepared for the fact that in case of heavy bleeding, severe infection or other dangerous changes, the patient will need not just a visit to the doctor, but even hospitalization. Although, in fact, the likelihood of such complications is incredibly low, so a patient’s stay in the hospital after surgery is almost never required.
We recommend: If one of these symptoms is noticed, you should seek advice from the surgeon who performed the operation on the patient. This step will likely help eliminate hospitalization.
So, dermatologists remove many different moles every day, but in each case they never tire of repeating the same instructions to the patient: “The main thing is to monitor your health and consult a doctor at the first unpleasant and disturbing sensation.”
Current issues
“Before” and “after” mole removal
Most patients, after undergoing a laser mole removal procedure, observe some characteristic reactions of the body during the first two weeks, some of which are normal responses that are compensatory in nature. Let's consider several pressing issues regarding the consequences of removing nevi on the face and body.
Can cancer occur after mole removal? Skin cancer, or melanoma, usually develops as a consequence of the malignant transformation of a melanoma-prone mole. Moreover, if during the laser correction process the specialist incorrectly determined the required depth of the beam and did not completely remove the mole, the risk of developing melanoma increases.
After removal, a tubercle appeared. Despite the low-invasiveness of the technique, in the process of removing the nevus, healthy surrounding tissue remains, which will have to undergo the healing process of the wound surface that has formed in place of the mole. In this case, this zone can form a small tubercle, which will be covered with a dense crust in a few days. This is considered a normal reaction to manipulation.
Inflammation after removal of a birthmark. The inflammatory process after laser correction usually lasts for the first days, after which it goes away. If inflammatory signs persist for a long time, you must immediately contact the specialist who performed the procedure.
Can a scar or scar form after removal of a nevus? The formation of scars can only be observed in the case of forced premature removal of the protective crust from the wound surface.
The scar itches and hurts after mole removal. Itching, burning, peeling and redness around a mole after removal are characteristic symptoms of a burn, which can be caused by unprofessional work of a doctor. This unpleasant complication develops if the specialist incorrectly determined the depth of exposure and subjected healthy skin cells to laser burning.
Bibliography
- V. V. Anisimov, Yu. V. Semiletova, A. S. Barchuk, Z. A. Radzhabova. Current issues in surgical treatment of patients with primary cutaneous melanoma. Siberian Journal of Oncology, 2010 No. 2 (38).
Other articles:
- Five important tips on how to choose a dermatologist oncologist
- How does melanoma develop more often: from nevi or de novo - FOR COLLEAGUES
- Removing moles in summer: is it dangerous?
- How not to go crazy reading about melanoma
Useful article? Repost on your social network!