Children and adults sometimes develop inflammation behind the ear for various reasons. What it is and how to treat it correctly, a specialist will answer after a detailed examination, because the inflammatory process in this area is often a sign of many diseases. Inflammation can appear not only behind the ear, but also on the neck, accompanied by pain, fever or other symptoms. In any case, this condition requires medical attention, especially in childhood.
Sometimes redness appears along with inflammation. In infants and small children, the skin is very delicate, so it can often react with redness, and the immune system responds to any pathology by enlarging the lymph nodes behind the ear. In addition to the lymph nodes, the mastoid process of the temporal bone becomes inflamed, which leads to mastoiditis.
General symptoms during the development of the disease
In the first stages of development, the symptoms do not cause any inconvenience, the signs are almost invisible. But three to four days pass, the exacerbation of symptoms cannot be ignored due to the rapid and aggressive increase in symptoms.
Both adults and children become restless, cannot concentrate on their usual activities, children refuse the most exciting games, they are not attracted to their favorite toys and entertainment.
Further development of the disease leads to the fact that it becomes difficult for the patient to focus on certain matters. In general, we can say that the patient’s quality of life is significantly reduced
First of all, this is due to significant cosmetic defects in one of the most injury-prone areas of the body.
It is difficult not to notice the presence of red spots in the area of the earlobe or in the folds of skin behind the ears.
Sometimes the manifestations of the disease can be quite vague, which requires additional diagnostics and tests. Treatment must be carried out under the supervision of a doctor, as there is a risk of progression of the disease.
Based on the study and recording of symptoms, the main causes are identified, allowing for effective treatment of the underlying disease and associated complications.
Psychological reasons for the appearance of red spots on the neck
First of all, you need to know in what situations they appear and after how long they disappear. If it is related to stress and goes away after you calm down, then it is most likely due to psychological problems.
Red spots often occur in people with closely spaced vascular capillaries as a result of the influence of irritating factors on a person’s emotional state.
Mental experiences through a complex system of connections between hormonal and immune factors, the autonomic nervous system with the participation of neurotransmitters influence the state of skin wall tension, the course of metabolic and inflammatory processes.
To correctly determine the causes, consult a doctor who can refer you to an appropriate specialist (psychologist, psychiatrist, dermatologist, allergist, gynecologist or endocrinologist).
Paroxysmal redness of the skin is the result of excessive activity of the sympathetic system, which is stimulated in stressful situations or during strong emotions.
Overactivity of the sympathetic nervous system can lead to symptoms from even the most minor emotional stimuli.
One of the reasons for the appearance of psychologically based red spots on the neck and décolleté may be social phobia.
This is an anxiety disorder that belongs to the group of neurotic disorders. Occurs in approximately 7-9 percent of the population. Often goes unrecognized, because is taken for ordinary shyness.
Social phobia is associated with specific situations in which a person feels judged or perceived negatively, such as public speaking or dating situations.
In addition to redness, there are other symptoms such as:
- Cardiopalmus;
- Trembling of hands, voices;
- Dyspnea;
- Increased sweating;
- Dizziness.
The factor that causes this type of phobia may be a previous history of public humiliation or ridicule, for example, in childhood.
The result is an exacerbation of symptoms to such an extent that they also appear upon contact with close relatives.
Social phobia has a negative impact on a person’s entire life and leads to a limitation in activities.
How to treat eczema on the scalp in the hair?
Today, there are many ways to treat this disease; many necessary medications and auxiliary products are available without a prescription from a doctor, so most people independently determine the specifics of therapy.
However, it is still better to consult a dermatologist first to make sure the diagnosis is correct. The most popular treatments for various forms of eczema are discussed below.
Shampoo
There are a large number of over-the-counter shampoos that you can start using even before visiting a dermatologist.
Before purchasing, you need to carefully study their composition; the following components can help in the fight against eczema:
- Selenium sulfide eliminates existing inflammation and dryness, eliminates itching, and also destroys yeast fungi, which can provoke the occurrence of many dermatological diseases.
- Tea tree oil, the optimal concentration in shampoo is about 5%. Such remedies eliminate not only eczema, but also the infections that arise from it.
- Zinc pyrithione. This component eliminates peeling and also destroys all bacteria and fungi. Additionally, it will promote accelerated regeneration of damaged skin.
- Ketoconazole can be found in both over-the-counter and prescription shampoos. This is one of the most effective components to fight eczema.
- Salicylic acid. The component is added to many medicinal shampoos; it cleanses the upper layers of the skin and promotes accelerated healing of damaged areas.
Ointment
Various ointments also demonstrate a high degree of effectiveness in the treatment of eczema.
Dermatologists recommend using the following varieties:
- Salicylic ointment. You can read what salicylic ointment helps with on our website.
- Zinc ointment.
- Naphthalene ointment.
- Corticosteroids in the form of ointments are used in the most complex or advanced cases; they can only be used as prescribed by the attending physician.
Folk remedies
Various traditional medicines have not lost their relevance; some effective ways to eliminate the main symptoms of eczema are given below:
- Applying natural bee honey to your head can reduce flaking and get rid of itching. If necessary, it can be diluted a little with water, after which, for 2-3 minutes, begin to rub into the damaged areas with gentle movements. After the procedure, your hair should be washed using regular shampoo.
- Sage lotions can speed up the healing process of damaged skin. To do this, tablespoons of dried sage are diluted in 0.5 liters of water, which is then brought to a boil. You can add one tablespoon of fresh honey to the finished product, after which cotton swabs are moistened with it and applied to areas affected by eczema for 20-30 minutes.
- You can prepare a decoction, which is obtained by adding 40 grams of oak bark to 200 ml of water, brought to a boil. The product sits for 12 hours, after which one tablespoon of fresh honey is added to it. All components are thoroughly mixed to ensure uniformity of the structure, after which the decoction is applied to the affected areas of the head. After an hour, you will need to rinse it with warm water.
Eczema does not pose a serious health threat, but at the first signs of the disease you should seek medical help immediately. Treatment in the initial stages shortens the recovery time for damaged areas of the head and minimizes the risk of relapses in the future.
Prevention
The main methods that can prevent peeling of the skin in the ears are:
- Compliance with the rules for cleaning the ears - only the outer part of the ear canal is treated with a cotton swab, since wax comes out of the inner part on its own when chewing movements of the jaw are made.
- Regular treatment of hearing aids (if used) with special means, as well as the use of ear rinsing drops.
- Protecting ears from water, for example, in a swimming pool, which is important for adults and children. Infants (up to 1 year) must be bathed after closing the ear canals with special cotton swabs.
- Protect your ears from cold air and drafts.
- See a doctor and take prescribed medications for colds, acute respiratory viral infections, etc., which can stimulate the appearance of otitis media.
- To clean the ear canals, do not use improvised means that can injure the skin (hairpins, toothpicks, etc.).
Self-medication with the achievement of a visible cosmetic effect is not always evidence that the cause of peeling has been eliminated. Only a doctor can say exactly why the ears are peeling and how to eliminate this problem most effectively without harming other body systems. Timely therapy, selected taking into account the patient’s health characteristics, increases the chances of complete restoration of the skin in the ear area.
The most important of them are:
- A varied, balanced diet, including plenty of fresh fruits and vegetables.
- Quitting smoking and drinking alcohol.
- Regular physical activity.
- Timely treatment of colds.
- Protect your ears from water when visiting swimming pools.
- Avoid being in drafts without a hat.
We suggest you read: Do crab sticks make you better? You should pay special attention to cleaning your ears. The procedure should be carried out with cotton swabs only in the outer area of the ear canal. There is no need to try to get sulfur from the “depth”, since it comes out on its own during chewing.
If peeling of the auricle occurs, you should not self-medicate. Only a doctor after a comprehensive examination can determine the true cause and prescribe effective therapy.
https://www.youtube.com/watch?v=Ah4m_masEfI
You should be especially careful when cleaning your ears. The procedure should be carried out with cotton swabs only in the outer area of the ear canal. There is no need to try to get sulfur from the “depth”, since it comes out on its own during chewing.
How to get rid of scabs
The mistake of many people suffering from the formation of crusts in the ears is that they do not go to the doctor and direct all their efforts towards eliminating the scabs. This is fundamentally wrong, as a result of which the skin again becomes covered with a yellow coating, scales and crusts.
First of all, therapy is aimed at the underlying disease. Only after complete recovery will crusts on the ears stop appearing. Treatment depends on the diagnosis, as well as on the stage of the process and the individual characteristics of the patient.
Otitis involves the use of the following medications:
- antibiotics – Ciprofloxacin and analogues;
- combination drugs – Sofradex, Candibiotic;
- antiseptics – Miramistin.
Fungal infections:
- solutions and drops – Nitrofungin, Clotrimazole;
- ointments – Pimafucort, Lamisil;
- capsules – Fluconazole.
Eczema and dermatitis require comprehensive treatment aimed at both suppressing the pathological process and supporting the body’s immune system.
Only completing the full course of treatment is guaranteed to get rid of crusts on the ears. It is not recommended to self-medicate, or use dubious methods of traditional medicine. The most effective and safest ways to get rid of yellow crusts is the use of chamomile, calendula or string in the form of a decoction.
For preparation, you need 1-2 tablespoons of the plant and 200 ml of boiling water. The decoction is infused for 5-6 hours and cooled to room temperature, after which the affected area is moistened with a cotton pad. Do not rub the scales too hard or try to get rid of them mechanically. Wiping must be done 5-6 times a day. Chamomile, string and calendula have antibacterial and healing effects.
Before using a traditional recipe, you should consult a doctor. Possible contraindications and individual intolerance.
Dandruff is not just a cosmetic problem
In the world, 70% of the population suffers from dandruff. This is a sign of some changes in the body that affect the condition of the skin on the back of the head and the scalp. Exfoliating skin particles cause irritation and cause a person to constantly scratch the area. You can fight this scourge at home by purchasing the appropriate hair care product. But, there are cases when seborrhea is caused not by drying of the skin, but by the activity of fungal organisms.
The fight against “oily” dandruff caused by a fungus is impossible without consulting a doctor. Regular shampoos will not help here, but will only make a person scratch the back of his head even more. Persistent dandruff, which causes severe discomfort, appears due to improper metabolism. Dysbacteriosis and diabetes are some of the main causes of this type of seborrhea. You can get rid of it only with the help of qualified medicine, normalizing the functioning of the sebaceous glands of the scalp.
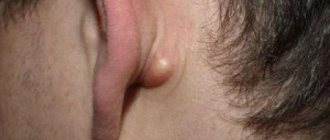
Atheroma
Atheroma is a benign formation from the secretion of the sebaceous glands, which occurs if the duct of the sebaceous gland is blocked. Atheroma can become one of the causes of inflammation behind the ear in a child, since the sebaceous glands are located there.
The exact cause of the disease is unknown. It is believed that the factors may be: impaired metabolism, insufficient body hygiene, increased work of the sebaceous glands, heredity, hormonal disorders, unfavorable ecology.
Symptoms
Atheroma looks like a round formation located under the skin. It usually doesn't hurt or itch. Externally, it is practically no different from a lipoma.
Sometimes the atheroma becomes inflamed, then the swelling noticeably increases, pain appears, the skin above the inflammation turns red and becomes hot. Rarely, the atheroma itself opens and contents with an unpleasant odor are released from it.
In infants, atheroma looks like small white rashes with a pearlescent tint. They are located in groups behind the ear, on the cheeks, forehead, nose and nasolabial folds. Atheroma of infants is also called milia.
Sometimes atheromas in infants can become inflamed and even suppurate, but usually do not require treatment and go away on their own. You just need to monitor the hygiene of the skin of a newborn baby.
Treatment
Treatment of atheroma is carried out only surgically: it is removed along with the capsule. This is a guarantee that atheroma will never grow again in this place. The operation is performed under general anesthesia, either classically or using a laser or electric knife.
If the atheroma does not bother the child, does not grow, or does not become inflamed, then doctors advise waiting to remove it and performing surgery after 3 years.
Treatment
Treatment of this symptom requires identifying an accurate diagnosis and causes. After identifying them, the doctor prescribes a number of measures. Depending on the etiology of the disease, this may include both drug treatment and various concomitant procedures.
If the patient experiences an allergic reaction, the doctor prescribes the following recommendations:
- Avoiding contact with allergens (metal jewelry, household chemicals, certain categories of food);
- The use of antihistamine antiallergic drugs (Fenistil, Loratadine, Suprastin).
In case of eczema or dermatitis, to eliminate swelling of the skin, as well as crusts that have arisen, the doctor prescribes anti-inflammatory drugs, in particular Sofradex, Otipax, drying and softening creams and ointments.
If the patient is bothered by a boil, then, as a rule, surgical intervention may be required, and then antibiotic therapy is prescribed.
In case of fungal infection, the type of fungus is first determined, then all the necessary ointments are prescribed to reduce the impact of the pathogen and neutralize its effect on the skin.
If the patient comes with otitis, then treatment is carried out only under the strict supervision of a doctor using antibacterial drugs such as Amoxiclav, Nitrofural. Auxiliary physiotherapeutic procedures are also prescribed.
All dosages of drugs are prescribed only by a doctor, and each case requires a professional approach and careful monitoring.
Seborrheic dermatitis
Seborrheic dermatitis is a fungal disease that affects areas of the skin rich in sebaceous glands. If a person suffers from itching specifically in the parotid area, the possibility of this disease should first be considered.
Seborrheic dermatitis develops as a result of an increase in the number of fungi of the genus Malassezia in the skin microflora. It is known that this disease affects people suffering from hypersecretion of the sebaceous glands (the fungus feeds on the lipids that make up the sebum). Malassezia is considered an opportunistic fungus, meaning it is present on the skin of most healthy people. When immune defense is reduced (for example, due to hormonal imbalance, sudden climate change, treatment with antibacterial drugs, etc.), the amount of fungal microflora increases significantly. As a result, the following violations develop:
- peeling skin behind the ears;
- dandruff;
- itching;
- oily skin and hair;
- the appearance of a rash (“irritation”) as a result of inflammation of the sebaceous glands;
- decreased skin resistance to infectious and chemical irritants.
Some symptoms are caused by the influence of fungal waste products on the skin, others by a decrease in the number of beneficial bacteria (since fungi and bacteria constantly compete for the surface of the epithelium as a habitat).
Seborrheic dermatitis primarily affects the scalp - the scalp, the upper part of the forehead and the area behind the ears. In rare cases, inflammation spreads to the groin and armpits.
The affected areas of the skin behind the ears often crack and bleed. The situation is aggravated by the patient scratching the skin (this increases the risk of secondary infection). The fungus that causes seborrheic dermatitis can also affect the ear canals, in which case otitis externa occurs.
If left untreated, seborrheic dermatitis develops into seborrheic eczema.
Prognosis and prevention
If you follow the treatment regimen, the discomfort in the form of weeping ears recedes quite quickly. Thus, wet wounds become covered with a crust, which gradually begins to peel off during treatment. At the end of therapy, the patient may notice already healthy, slightly pink areas of the skin, which will eventually acquire a normal color.
- maintain ear hygiene;
- have a nutritious diet;
- do not overindulge in sweets;
- find time for exercise;
- avoid stress.
If your ears are itchy, flaky or red, you should consult a dermatologist. This will eliminate the possibility of an infectious disease and certainly prevent its development.
Every mother knows that her baby’s skin is very sensitive and requires special care. But even with the strictest monitoring of the child’s health, there is a possibility of various rashes and redness. Very often, children experience redness behind the ear.
Hygiene procedures for scrofula
Daily hygiene is essential for a child suffering from scrofula. The area behind the ears is washed during water procedures - taking a bath or shower. The water should not be hot (36-37°), purified through a filter or boiled.
To further soften and relieve discomfort from the problem area, bathing products are used:
- Emolium is a special emulsion;
- Atoderm with zinc;
- Trixera;
- Mustela is a bath oil that is good for chapped spots.
Adding infusions of medicinal herbs with antimicrobial and wound-healing effects to bathing water - string, chamomile, oak bark, St. John's wort, bay leaf - is allowed for children from birth and helps cure scrofulous crusts behind the ears.
Using soap to wash your baby is a common mistake parents make. Ordinary alkaline soap, even with the label “baby”, is not suitable for skin hygiene with scrofula behind the ears.
Washing with soap will dry out the skin even more, causing peeling and painful cracks.
For the hygiene of children with scrofula, it is important to use soap with a neutral pH level and the absence of sodium lauryl sulfate. Pharmacies offer soft soap-free detergents with herbal extracts (chamomile, string) - Moraz baby soap, Chereda soap from Aptekoff. Important! Mild soap is not recommended for daily use; it is optimal to use it 2-3 times a week
Back to contents
Important! Mild soap is not recommended for daily use; it is optimal to use it 2-3 times a week. To the content. Back to contents
Back to contents
The skin behind the ear peels and gets wet: causes, treatment methods for adults and children
Peeling of the skin behind the ear indicates the development of a pathological process in the body. Inflammation occurs under the influence of various provoking factors. Only a doctor can determine the exact reason why the skin behind the ear peels and gets wet, and prescribe the correct treatment.
Symptoms
If inflammation occurs behind the ears, a number of general symptoms appear on the epithelium:
- itching, discomfort, rash,
- the skin peels and gets wet,
- blisters appear on the irritated areas, after opening which yellow crusts form,
- humidity in the lesions progresses,
- cracks appear
- there is pain, redness, burning,
- the inflamed areas begin to itch unbearably,
- a foul odor emanates from wet skin,
- patients develop psychoemotional disorder.
If treatment is not started, the signs of the pathological process will increase:
- irritation appears
- sleep is disturbed
- performance decreases,
- a complication develops: in addition to the fact that the person’s skin behind the ears peels and gets wet, a secondary infection occurs in the areas of inflammation.
Scrofula, gneiss
With exudative diathesis, the skin in the parotid area peels and becomes wet in adults and children. Leads to scrofula:
- uncontrolled consumption of sweets,
- decreased immunity,
- genetic predisposition,
- lack of vitamins and minerals,
- unbalanced diet (monotonous, poor diet),
- complications after viral infections (flu, acute respiratory infections, measles).
When the skin becomes wet and itchy behind the ears of women, men or children, one should not take such a dermatological disorder carelessly. This is a pretty serious disorder. The development of inflammation leads to damage to:
- circulatory system,
- joints,
- cartilage and bones.
In the parotid area, the skin begins to become wet due to gneiss caused by metabolic disorders. Areas of peeling with wet spots form near the ears and cover the scalp. Gneiss appears in the background:
- poor nutrition,
- hereditary predisposition,
- disrupted lifestyle,
- psychogenic disorders,
- nervous breakdowns, stress, depression.
Allergy
Epithelial tissues may peel and become wet when allergic reactions develop. Foci of inflammation appear on the skin that comes into contact with the irritant.
Allergies are provoked by:
- cosmetics (creams, shampoos),
- jewelry and accessories (earrings, glasses, headphones),
- aggressive chemicals from the environment (industrial gases, aerosols).
Allergens that penetrate inside the body lead to negative reactions:
- medicines,
- food products (citrus fruits, chocolate, honey, nuts).
Therapy
Treatment of the patient begins by determining the cause and type of disease. The treatment regimen includes the necessary medications and procedures.
If a man, woman or child has skin damage behind the ear caused by allergies, use the following algorithm:
- eliminate the irritant (jewelry, cosmetics, medicines),
- adhere to a hypoallergenic diet,
- Antihistamines are prescribed: Fenistil, Loratadine, Suprastin, Tavegil, Zyrtec.
For eczema or dermatitis, treatment is carried out as follows:
- They use drugs that can relieve inflammation and itching: Sofradex, Otipax.
- They use ointments and creams to eliminate swelling, dry out, soften the skin, and regenerate cells: Radevit, Dexpanthenol, Fenistil-gel, Ichthyol and Zinc ointment.
- In severe forms, the lesions should be smeared with external agents containing corticosteroids: Hydrocortisone, Pimafucort, Afloderm, Elokom.
- If a secondary infection occurs, antibiotics are used: Erythromycin, Doxycycline, Ciprofloxacin.
For fungal infections, therapy includes:
- ointments, drops and solutions that can suppress the development of pathogenic microorganisms: Itraconazole, Terbinafine, Naftifine, Econazole, Clotrimazole, Fluconazole, Pimafucin,
- tablets: Flucostat, Pimafucin,
- medications to restore intestinal microflora: Bifiform, Acipol, Linex.
Skin lesions behind the ear with otitis media are treated with antibiotics:
Medicines and dosages are selected by the doctor depending on the pathology that has arisen. Self-medication without clarifying the diagnosis leads to the development of dangerous complications.
Ear allergy rash
According to medical statistics, most often a red rash in the ear area indicates an allergic reaction. Therefore, if you identify this symptom in yourself or your child, you should not panic too much. Think about what you ate and what you did the day before. Please note that allergies do not only occur due to ingestion of the allergen. In some cases, the disease manifests itself due to other factors:
- If we are talking about a child no older than two years old, the presence of a rash behind the ears may indicate underdevelopment of the gastrointestinal tract. This usually happens when a child is switched to adult foods too abruptly after breastfeeding or formula.
- Even if a person regularly eats a particular product without problems, sooner or later an allergy may develop to it. This usually happens when a person’s immunity is significantly reduced.
- Allergies can be seasonal. that is, it occurs during the flowering period in spring.
- If an animal lives in the house, a reaction may occur to the fur.
- Often, a rash occurs when wearing jewelry on the ears made of low-quality material.
- The cause of the development of the symptom may be the use of cosmetics, including powder and fabric softener with aromatic fragrances.
READ ALSO: A child has red bumps on his tongue: reasons for what it could be (photo)
Scrofula in children behind the ears: photo and treatment of cracked, weeping and flaky skin
In the process of carrying out hygienic manipulations, it is necessary to pay attention not only to the ears, but also to the space behind them. When taking a bath, you need to lower the baby’s head into the water so that only the face remains on the surface, this will soften the crusts and remove them without problems
Immediately after the water procedures, you need to take a piece of bandage, wrap it around your finger, moisten the material in vegetable or medicinal pharmaceutical oil (for example, sea buckthorn) and treat the clean and dried skin behind the baby’s ears.
Tip: Increased attention should be paid to the area behind the baby's ears during the summer months. If sweat constantly accumulates in the hidden area, the baby will suffer from diaper rash, irritation and inflammatory processes
In some cases, you can even use powder to prevent moisture buildup.
If sweat constantly accumulates in the hidden area, the baby will suffer from diaper rash, irritation and inflammatory processes. In some cases, you can even use powder to prevent moisture buildup.
Tip: Increased attention should be paid to the area behind the baby's ears during the summer months. If sweat constantly accumulates in the hidden area, the baby will suffer from diaper rash, irritation and inflammatory processes. In some cases, you can even use powder to prevent moisture buildup.
In some cases, you can even use powder to prevent moisture buildup.
After a few minutes, carefully wipe the treated areas, removing any remaining plaque and medication.
Such manipulations are also good for preventing the condition. As a last resort, it is recommended to wipe the problem area every day with a cotton swab dipped in warm water. Twice a week we apply moisturizing cream or a little vegetable oil to the skin to soften the tissues.
Scrofula in children behind the ears
Scrofula is the name of exudative diathesis, known since the time of our grandparents, which is considered a manifestation of dermatitis at an early stage. Basically, this disease affects the area behind the ears and most often affects children from two to ten years old. Scrofula behind the ears in infants is much less common.
Scrofula behind the ears - causes of occurrence
- In most cases, the main causes are hereditary predisposition. Children whose parents suffered from syphilis, tuberculosis and various cancers have a high risk of developing scrofula.
How to treat such unpleasant scrofula behind the ears?
For topical use, sudocrem, zinc ointment, bepanthen or fucorcin are recommended. Traditional medicine recommends bathing the baby every evening in decoctions of medicinal plants (oak bark, tricolor violet, etc.) to relieve itching and inflammation. Infusions and decoctions are also used internally (for example, coltsfoot).
womanadvice.ru
- Scrofula in adults
- Gneiss in adults
If an adult gets wet behind the ears, it can be a symptom of various diseases. First of all, weeping skin indicates the presence of some kind of skin disease, so treatment should be carried out under the supervision of a doctor.
Often, constant moisture behind the ears can be accompanied by itching, peeling of the skin, irritation and burning. The causes of a constantly weeping area behind the ear are determined using secondary symptoms.
(adsbygoogle = window.adsbygoogle || []).push({});
Scrofula in adults
Scrofula most often occurs in children, but any adult is not immune from this disease. Why is it necessary to promptly treat scrofula? Although the disease itself is not terrible, tuberculosis can become a complication, and the infection easily spreads to the brain and causes life-threatening inflammation there.
Scrofula is a disease of the circulatory system, affecting joints and bone tissue, as well as the lymphatic system. Its symptoms appear on the skin: behind the ears in adults most often.
If left untreated, scrofula on the skin can spread to other areas of the body. The skin affected by the symptom of scrofula is very itchy and becomes golden in color, a crust forms on it, which may come off over time.
The skin at the site where the crusts form is very flaky, and after they disappear, it turns pink and constantly gets wet.
Scrofula is not an infectious disease and is not transmitted from person to person through skin-to-skin contact or airborne transmission. Main causes of the disease:
- improper diet with a lack of vitamins;
- low immunity due to lack of physical activity;
- insufficient skin care, especially in the area of the ears and ear canal.
Basic therapy methods
Hives on the neck are treated with medications and folk remedies. In this case, you should not self-medicate. Any medications should be taken under medical supervision.
If redness in the neck is caused by nervous tension, take valerian infusion, motherwort herb, Tenoten, Afobazol, Novopassit, Persen. Itchy pimples can be lubricated with ointments and gels that contain an antibiotic. They dry out the rash on the face and neck, relieve inflammation, and destroy bacterial flora.
When the itching is allergic in nature, histamine blockers are prescribed. They reduce the production of this hormone, which, in turn, provokes the formation of allergy symptoms. When treating a red rash on the neck in an adult, the following are used: Loratadine, Diazodlin and Suprastin.
For demodicosis, emulsions Medifox and Benzyl benzoate, Wilkinson's ointment and sulfur ointment are prescribed. They treat only the affected areas. As the mites die, the intensity of the itching decreases. The neck completely stops itching after three uses.
Fungal infections, dermatitis, and infectious diseases are treated with medications. Only a doctor can prescribe the necessary medications. Self-medication in this case is contraindicated, since these medications have a large number of contraindications and side effects.
Immunostimulants are prescribed for psoriasis. This includes tinctures of Eleutherococcus and Echinatia, Lykopid tablets. For external use, ointments, gels and emulsions are prescribed.
The easiest way to relieve itching is to take a bath in cool water. An oatmeal bath will also help. To do this, you need to grind a glass of cereal using a coffee grinder and dissolve the resulting powder in water. The bath should be taken for at least 15 minutes.
You can use a baking powder mask. To prepare it you need to take 2 tablets of ascorbic acid, a few drops of water and a little baking powder. These ingredients must be mixed until smooth and applied to the affected area.
A decoction of medicinal herbs will help relieve itching and redness on the neck. It includes chamomile, calendula and string. Using a decoction you can relieve inflammation, irritation and itching. To do this, you need to wipe your neck three times a day with a moistened disc.
You can also rub your neck with olive oil and use moisturizers.
To avoid the appearance of a rash on the neck, you should not wear massive jewelry in the summer for more than 6 hours a day. All jewelry should be cleaned regularly with a special solution. This will remove any dirt or oil that may be causing irritation. Neglect of these simple rules explains why the back of the neck itches in hot weather.
If the neck constantly sweats, then it should be wiped with a dry soft cloth. In the summer, it is worth taking a shower daily.
Since it is impossible for men to give up shaving, to avoid minor rashes on the neck, you should purchase a high-quality razor with smooth shaving blades. It is also worth using special shaving products.
Clothes and linen should be washed using products that do not contain fragrances or fragrances. To clean it of all chemical compounds, you need to use an additional rinse.
When choosing clothes, give preference to natural materials. It is better to wear cotton; wool and polyester can irritate the skin. Make sure that your clothes do not have a too tight neckline.
And remember, if irritation does appear on your neck, do not scratch or scratch it! Even a small wound can open the door to infection.
Red spots on the neck appear unexpectedly. Even with a little stress and embarrassment. They are a sign that something wrong is happening inside. Their appearance can be unpleasant and lead to avoidance of social contacts.
- Why do red spots appear on the neck?
- Psychological reasons for the appearance of red spots on the neck
- Treatment of social phobia
- Eritophobia or fear of spots
- How to overcome your fear of blushing
- What to do or how to deal with the problem
- Other causes of red spots on the neck
Duration of treatment
Scrofula is a long-term disease with periods of subsidence of negative symptoms and exacerbations.
Treatment - regular, if there is external well-being (palening and reduction of spots, peeling behind the ears, disappearance of itching sensations), the use of ointments is continued with prevention for up to 3 months, otherwise the risk of recurrence of rashes behind the ears is high.
The diet after cleansing the skin is expanded gradually; if scrofula symptoms return, dietary restrictions are reintroduced.
Scrofula behind the ears in infants and children over one year of age is treated for an average of 4-6 months. In most children, the disease completely resolves by the age of 5. A protracted course of exudative catarrhal diathesis occurs against the background of errors in the child’s diet and weakened immunity.
The following signs indicate recovery:
- Long-term absence of rashes and spots.
- The skin acquires a natural color and does not peel off.
- Itching and other unpleasant sensations do not bother me.
- The general condition of the child is satisfactory.
- Blood and urine tests are normal.
- When expanding the diet, there are no negative reactions from the skin.
Scrofula behind the ears requires immediate treatment. In the absence of therapy, the disease progresses - the spots spread throughout the head, and problem areas may become infected with suppuration. Against the background of scrofula, lichen and lupus erythematosus sometimes develop.
Back to contents
Diagnostics
The doctor diagnoses the disease after a visual examination of the foci of inflammation and laboratory tests. The following methods are used to make a diagnosis:
- In case of purulent-inflammatory processes, the patient's ear is examined using an otoscope.
- If the disease is allergic, the patient is prescribed blood tests. Tests allow you to identify the irritant that led to a negative reaction.
- In case of eczema, damage to the epithelium is carefully examined.
- Patients suffering from diabetes undergo hormone tests.
The doctor selects diagnostic methods, taking into account the specifics of the disease.
Why does a child's ears itch?
In children, as in adults, the causes of ear itching can be very different, but pediatric ENT specialists can successfully treat all of them.
- If water gets into your ears - after taking water procedures, be sure to dry them with a napkin and avoid exposure to cold. If a child, for example, needs to go outside after swimming in the cold season, carefully dry his head and ears and put on a hat.
- Accumulation of sulfur - with regular hygiene, this problem rarely occurs. It is enough to thoroughly clean the children’s ears with cotton wool 1-2 times a week. It is not recommended to use cotton swabs - they do not so much clean as they push sulfur inside, which is also fraught with serious problems.
- The appearance of a foreign body in the ear - no independent action, only the doctor will carefully remove the object, without frightening the child or causing him pain.
- Ear mites are, as in adults, a very unpleasant phenomenon, which, however, can be successfully treated.
- Inflammation of the outer or middle ear - a doctor prescribes antipyretic and painkillers along with antibacterial or antiviral treatment.
- Drowsiness - you may not have noticed, but often babies, when they want to sleep, begin to actively scratch their ears. The reason is unclear, but this phenomenon occurs in most children.
- Sulfur plugs - they try to remove plugs for children only mechanically, so as not to scare them.
Eritophobia or fear of spots
Another type of social phobia that causes red patches on the face and neck is erythrophobia, or the morbid fear of blushing.
A person suffering from this condition is terribly afraid of the appearance of red spots in society. As a result, he begins to avoid being in these types of places, often blushing at the very thought of being in large groups of people.
A person with this type of phobia feels like he is the center of attention and everyone around him can see his skin reaction.
The cause of erythrophobia is the abnormal functioning of the sympathetic nervous system, which is manifested by excessive stimulation in stressful situations and causes emotional tension.
Over time, this becomes chronic, causing frequent redness that is not related to the original cause.
Erythrophobia is also accompanied by shyness, embarrassment, and fear of condemnation and criticism. Dealing with this type of phobia is not easy. The more often the patient thinks about redness, the more often it appears. There is a fear of judgment from others.
This phobia occurs in both children and adults. Lack of feelings, coolness in communication on the part of parents, all this can cause the development of erythrophobia in a child.
Types of eczema of the scalp
Eczema, which affects the scalp, has a number of varieties. Each type has characteristic individual characteristics and specific course.
Types of eczema on the scalp:
- Seborrheic eczema. The seborrheic variety of eczema is one of the most common forms of this disease, its main features are as follows:
- Lesions are localized not only on the scalp, but at the same time they can appear on the chest, abdomen and skin folds throughout the body.
- At the initial stage, the formation of nodules with a pinkish-yellow color is observed. Later, characteristic plaques develop from them.
- The risk group primarily includes people who have been diagnosed with oily seborrhea of the scalp.
- Weeping eczema. Weeping eczema can be caused by an acute allergic reaction, as well as exposure to chemicals and other irritants on the skin. The main features of this form are discussed below:
- At the initial stage, an inflammatory process is observed that affects the upper layers of the epidermis, which had direct contact with the irritant.
- In places where skin redness and swelling have been noticed, bubbles of small diameter will soon form.
- The blisters merge with each other, which leads to the formation of erythema.
- The affected area has a constantly weeping surface, which gradually becomes covered with a crust.
- This form of eczema is characterized by a strong burning sensation in the affected areas and a feeling of unbearable itching. However, scratching or frequent touching should not be allowed, as wet areas can easily become infected, which can lead to serious complications.
- Microbial eczema. Microbial eczema can occur in the presence of existing skin lesions, especially if purulent inflammation appears. At risk are people with extensive head burns, deep wounds and other similar injuries, and erysipelas. Eczema has the following features:
- Small blisters filled with pus begin to appear on the affected areas of the skin.
- After some time, the bubbles open, which leads to the formation of crusts.
- The skin on the affected areas becomes rougher and becomes frequently wet.
Why do red spots appear on the neck?
The most trivial reason for a red neck is strong emotions. Sadness, anger or shame lead to increased blood pressure and dilation of blood vessels. For some people, this manifests itself as a flush on the neck and face.
They may be a sign:
- Stress;
- Allergies (for example, to certain foods, spices, alcohol or medications);
- Excessive activity of the sympathetic system;
- Disorders of the thyroid gland;
- Angioedema erythema.
Red spots on the neck are often a result of overexposure to the sun. The skin of the face, neck and décolleté is more exposed to sunlight than the rest.
On hot days, without using appropriate sunscreen, you can get a sunburn, which manifests itself as redness, pain and burning.
Erythema on the skin of the neck can occur due to insect bites, the venom of which causes local inflammation and mild pain.
However, it happens that a sudden, life-threatening allergic reaction occurs - anaphylactic shock. Rapidly progressive swelling of the neck can cause the airway to close and make breathing difficult. In this case, immediate hospitalization is required.
Another reason is skin diseases such as mycosis, psoriasis, dermatitis.
Discoloration and erythema may also indicate liver problems.