The most common disease among men is a fungus on the genitals. It can quickly spread to other genital organs. Most often, the genital area and folds are affected by this disease. The appearance of a fungus in the scrotum area prevents a man from living a full life. Read about the treatment and symptoms of fungus, a photo of which is not included for aesthetic reasons, in this article.
The fungus can appear on any part of the body in people, as it is an infection of internal organs. In a man, such a disease may appear on the scrotum, which causes him to panic. If a fungus occurs on the scrotum, you should not treat it yourself, as this can lead to even greater complications. At the first symptoms, it is best to consult a specialist who can make the correct diagnosis and prescribe the necessary treatment.
Reasons for appearance
The disease is caused by fungi (Tinea cruris) or bacteria (staphylococci).
Fungal infection is more often found in adult men around 40 years of age. When the pubic area sweats, fungi begin to multiply. Inflammation appears in the intimate area.
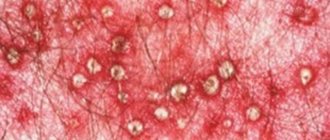
Image: groin fungus in men
Most often, men who are susceptible to the disease are:
- visit public baths;
- suffer from excessive sweating (hyperhidrosis);
- wear tight-fitting synthetic underwear;
- live in hot countries;
- have endocrine, cardiovascular diseases and infections that weaken the immune system;
- have weight problems.
In addition, those men who have mycosis of the feet are at risk. Often inguinal athlete's foot appears in athletes. Athletes' feet constantly sweat, a fungus may appear, and then spread from the feet to the groin area.
This disease is dermatological. Infection with the fungus occurs due to close contact with the infection. The causative agent of the fungus Pityrosporum orbicualre begins to spread throughout all organs if it is not treated in a timely manner. Due to the impact of negative factors on this component of the body, it actively reproduces.
Causes
Lichen versicolor on the scrotum is a dermatological disease of an infectious nature. Infection can occur through contact with a sick person or through the use of his personal belongings containing contaminated particles of epithelium and hair on the surface, as well as through an infected animal. However, the likelihood of infection is low, and the disease is not highly contagious.
The causative agent of pityriasis versicolor is the pathogenic fungus Pityrosporum orbiculare. It is part of the normal microflora of human skin, but when exposed to unfavorable factors, it begins to actively multiply and lead to testicular fungus in men. The colonies of the fungus are round, smooth, and cream-colored.
Provoking factors:
- Increased sweating in humans, due to which the disease has a seasonal nature - it is more common in spring and summer;
- Genetic predisposition;
- Changes in sweat structure due to medication or food intake;
- Chemical production workers;
- Frequent exposure of a man to ionizing radiation (a radiologist or a man receiving radiation therapy);
- Neglect of personal hygiene rules.
Pityriasis versicolor does not occur in older people or in children under 7 years of age . The risk group includes people with tuberculosis, diabetes mellitus, cancer, hormonal disorders and acquired or congenital immunodeficiency conditions. The increased risk of pityriasis versicolor on the scrotum due to hormonal imbalance explains the incidence of the disease in young people during and after puberty.
Main features
If any traces of fungus occur, it is better to contact a specialist; he will prescribe the necessary medications that should be taken only according to his prescription. It is very easy to identify the fungus, since yellow spots immediately appear on the scrotum. They differ from the color of the skin, so they can be seen with the naked eye.
Typically, infection occurs in crowded places, so you need to be as careful as possible in places such as a swimming pool, bathhouse or sauna. Always take personal hygiene products and use them both before entering the establishment and after leaving. When a fungus occurs, the following signs appear:
- unbearable itching;
- acute pain;
- peeling of the skin.
Already based on these symptoms, there should be a suspicion of the presence of the disease. If a fungus appears on a man’s scrotum, he immediately panics.
Disease prevention
Prevention of this pathology must be carried out on an ongoing basis, trying to eliminate all factors that could contribute to the relapse of the disease. So, here’s what a person who wants to get rid of this disease once and for all should do:
- strictly follow all the rules of personal hygiene, including trying to combat excessive sweating;
- restore the previous level of metabolism and even improve it. In this case, you need to be examined by a specialist;
- take a shower once or twice a day;
- change underwear daily;
- use powders to reduce sweating;
- use personal hygiene products.
If you come into contact with things that have fungal spores on them, or with an infected person, you should wash your hands thoroughly with soap. It's even better to take a shower. This will give you a better chance of avoiding illness.
To prevent this problem, you must first observe the rules of personal hygiene.
Treatment for this problem can only produce results when the medications recommended by the doctor are taken as prescribed.
Types of pathogenic microflora
Dermatologists identify 3 types of pathogenic microflora that affect the groin area:
- The yeast species is the causative agent of candidiasis (this infection is better known as “thrush”). The disease affects the area of the scrotum, penis and genitourinary canal.
- The class "epidermophytons" causes dermatomycosis, which manifests itself as lichen. It occurs most often in men who play sports or lead a very active lifestyle.
- Pityrosporum are pathogenic fungi and appear on the scrotum as pityriasis versicolor. It occurs most often against the background of hormonal changes or problems with the amount of progesterone.
An important fact is that the fungus on the scrotum, caused by all three types, looks very similar. Therefore, only a doctor can identify the type of pathogen and the cause of the infection. And the quality of treatment will depend on the effectiveness of diagnosis.
Symptoms of inguinal athlete's foot
Inguinal fungus in men can be mistaken for infection with the herpes simplex virus or even Treponema pallidum, although the signs of these infections still differ.
Symptoms of the disease:
- At the beginning of the disease, a rash appears, the causes of which can be determined by the results of scraping. When analyzed, threads of mycelium are found in the tissue.
- The rash appears as pink or red spots of varying sizes, usually about 1 cm in diameter. If the fungus is not treated, the rash grows and increases in size, merging into a large red spot the size of the palm of your hand.
- A typical manifestation of symptoms is itching in the groin area. In this case, the pubis and anus area itch, but the itching does not affect the penis.
- In severe cases, fluid-filled blisters appear on the affected area. The patient scratches the sore area, so sores and ulcers appear on the skin. Cracks form. Wrinkling and peeling of the skin occurs.
- Healthy skin on the border with the fungal-affected area turns red and becomes dry.
- Darkening of the skin is noticeable on the scrotum, pubis and transition to the thigh area. Redness can turn into pigmentation. The affected area turns brown or reddish-brown.
- If you don't fight the fungus within 2 weeks, painful sores will appear and may require hospitalization.
Athlete's inguinal dermatitis is treated in the same way as mycosis - with antifungal drugs. Most antifungal ointments also have an antibacterial effect.
Source
How to treat fungus on the scrotum?
Whichever method you choose, follow these rules:
- Before applying any antifungal product, wash your intimate area with soap and water.
- Apply the medicine not only to the affected areas, but also to healthy areas of the groin skin.
- If you do not feel better in ten days, tell your doctor.
- Wear loose panties made of natural material and change them daily.
- Wash the hair in the groin with antifungal shampoo, or better yet, remove it for a while.
- If you use pharmacological drugs for dermatitis, strictly follow the instructions.
- Change bedding every day.
- Keep your groin dry by using talcum powder or powders.
- You can be treated with both medicines for the fungus and folk remedies.
You can purchase the following drugs:
- Regular cream or ointment against fungus: Ketoconazole, Clotrimazole, Terbinafine. Effective in the early and middle stages of the fungus.
- Antifungal ointment for skin with anti-inflammatory effect: Triderm, Miconazole. They help in advanced cases.
- Tablets "Fluconazole", "Nystatin", "Itraconazole". They are used only with a doctor's prescription.
- Antihistamines, for example, Suprastin.
If for some reason you do not want to use pharmaceutical drugs, try homemade treatment recipes. It is important to understand that their effectiveness against groin fungus in men is questionable and depends on a huge number of factors. Many patients waste time trying to get rid of the disease with folk remedies, and the infection progresses. At home you will be able to prepare medicines for rashes and inflammation.
Varieties of the disease are based on the bacteria that provokes the disease, thus there are:
- The yeast type is the previous stage of candidiasis or the so-called thrush. The disease affects the area of the scrotum, penis and even the genitourinary canal.
- Epidermophytons are a provocateur of dermatomycosis or, more simply, lichen. Most often, this disease affects men who lead an active lifestyle. There are often cases when athletes face exactly this problem, since they sweat significantly in the groin area, thereby providing two fundamental factors for the disease: a humid environment and high body temperature.
- Pityrosporum is a pathogenic fungus that manifests itself in the form of pityriasis versicolor. The main cause of this problem is a change in hormonal levels and is much less likely due to the amount of progesterone in the body.
Reddish spots that itch and cause discomfort
By type of skin manifestations:
- Pityriasis versicolor - middle-aged people encounter it, while children under 7 years of age and elderly people are practically not susceptible to it. The risk of encountering this disease increases during periods of hormonal imbalance. This type of disease is especially dangerous during puberty. The provocateur of the testicular fungus of this group gathers in colonies, thus, smooth cream-colored bulges are observed in the groin.
- Lichen versicolor is a dermatological disease of an infectious nature and infection occurs through contact with a patient or his personal belongings (touching a sick animal is also true). At the same time, this group of fungus is characterized by low contagiousness, thereby posing an immediate danger to the skin of the scrotum.
Most often, the fungus does not cause serious complications and can be cured with prescribed treatment. However, in order to dispel men's panic, it is necessary to undergo an examination by a specialist. The attending physician needs to tell you in as much detail and accurately as possible about your condition and point out the location where the unwanted fungus appears.
Kinds
There are several types of fungi. The classification below is based on the bacteria that causes the disease.
Table No. 1. Types of fungus
Attention: The internal data of table “72” is corrupted!
Fungus can be different, which means a special approach is needed for each type
There is another classification, different from the first. It is based on the types of skin manifestations.
Table No. 2. Second classification
Attention: The internal data of table “73” is corrupted!
Routes of infection
Any disease just won’t come out of nowhere. Localization of the fungus on the scrotum occurs due to several factors. Sometimes mycelia can be picked up somewhere, and in some cases they appear on their own when an environment favorable for their manifestation has formed.
Humidity is the most suitable condition for the manifestation of the disease. In a humid climate, constant sweating, poor hygiene and high ambient temperatures, the scrotum will immediately be affected by fungus. All of the above factors disrupt the carbohydrate-fat metabolism of the body, which causes mycelium to grow. This is most often found in hot countries, which is why they rank first in this disease.
A fungal infection begins to spread quickly if you have unprotected sex or use other people's hygiene products or underwear.
To become infected with a fungus, it is enough to just touch a surface once that contains at least a few small particles of the epidermis of the infected person. When the skin of the scrotum comes into contact with an infected object. This happens when hygiene rules are not followed. For example, when using a shared towel or when going to a public bathhouse or sauna.
And also, in addition to everything written above, you should maintain personal hygiene and often change your intimate area care products.
What does pathology look like and where does it come from?
There are many scenarios for the development of the disease, and knowledge of them helps to quickly identify the problem. Let's start with the first reason for the appearance of peeling skin in the scrotal area in a man - ignoring all the rules of individual hygiene.
- For example, a man should reconsider his underwear - it may already be worn out or was initially of poor quality. It's also worth checking how hard it presses.
- Another option is to check all shampoos, shower gels, etc. They may simply not be suitable for a man.
- It is also worth considering whether a man is doing epilation correctly, because if something went wrong during the shaving process, this may well be the reason for the appearance of inflammation in the scrotal area.
Fungus is not a picky phenomenon, because it can appear from anywhere.
Also, for infection with mycosis on the scrotum, which will develop in the future, at least one external factor is needed. These include the following.
- Humidity of the environment. It is caused by increased sweating, specific or strenuous activities, and poor personal hygiene.
- Increased change in ambient temperature. African countries take the lead in this regard. The heat there contributes to a significant spread of mycosis on the scrotum among the inhabitants of this continent.
- Failures in lipid metabolism in the body of a sick man (also called carbohydrate-fat metabolism).
The infection process itself begins to act after contact between the skin in the scrotum area and an object on the surface of which there are fungal spores. That is, we are talking about a contact route of infection.
Note! To become infected, a man just needs to neglect personal care and stop using common hygiene items (washcloth, bath towel, etc.).
There are many factors that contribute to the appearance of fungus on the scrotum
Now let's move on to another topic - risk zones. For a fungus to occur, you need not only an object, but also a “favorable” background that will contribute to the development of the disease. Such places include:
- sauna;
- bath;
- hospital facility.
In the last place, infection occurs as follows: a man comes into contact with his scrotum with a hospital duck, which at that time contains mycosis spores.
Let's move on to the appearance. Anyone can easily figure out what's going on just by looking at the fungus itself. As a rule, when it spreads, affected areas appear that become yellow.
Fungus is a pathology, the development of which can be seen with the naked eye
If you look at the skin under a microscope, you can see entire colonies of mycelial fungi in these areas.
Possible fungal diseases
Skin peeling on testicles photo
All the pathogenic fungi listed above can cause various diseases that have a similar symptom in the form of peeling skin on the testicles. Among these keratomycosis:
- candidal inflammation in the groin;
- athlete's foot inguinal;
- pityriasis versicolor;
- complications of mycoses.
In addition to localization on the testicles, the disease can simultaneously or gradually appear on all genitals, inner thighs and in the inguinal folds. Several factors contribute directly or indirectly to the occurrence of these unpleasant problems:
- overweight men, which leads to sweating and even diabetes;
- improper hygiene of the genitals and the whole body;
- untreated or chronic forms of skin, foot or nail fungus;
- wearing underwear with a high synthetic content or a narrow cut.
Poor nutrition, a sedentary lifestyle and severe stressful situations greatly weaken the immune system and provoke an increase in fungi. At risk are residents of areas with high air humidity and hot climates. This is why most fungal diseases recur in the summer. Most often, the skin on the testicles peels off in the summer, during the holidays.
If peeling skin on a man’s testicles was caused by pathogenic fungi, a dermatologist may recommend treatment with special broad-spectrum antifungals. In the absence of complications, you can limit yourself to local creams or ointments, liquid solutions. The most effective and common are:
- Clotrimazole;
- Lamisil;
- Terbinafine;
- Ketoconazole;
- Nystatin.
Cream Lamisil for fungus
If the condition is neglected, peeling moves to the genitals and inguinal folds, Triderm and Miconazole will help relieve inflammation and irritation. These are drugs with an enhanced formula that not only destroy fungi, but also soothe the skin and promote its healing.
Peeling often causes itching, which can be relieved by antihistamine drops or Claritin or Suprastin tablets. If fungal inflammation is difficult to treat or has become chronic, a short course of Fluconazole or Itraconazole is added to local treatment with ointments.
Daily treatment with iodine, streptocyte or sulfur ointment helps eliminate peeling skin on the testicles and suppresses the growth of fungus. Such procedures should be carried out for at least two weeks. This will prevent recurrence of mycosis and restore comfort in the groin area.
Peeling skin on the testicles
Inflammatory processes on the skin are often accompanied by peeling, itching, and discomfort.
Having discovered similar symptoms on the testicles, many men assume a wide variety of, sometimes terrible, diagnoses, delaying a visit to a specialist. But in addition to sexually transmitted infections, there are many external or internal causes of this problem, among which fungal diseases stand out separately. If you find that the skin on the testicles is peeling, there is no need to panic, but rather consult a specialist. Peeling skin on the testicles
Diagnostics
If a man notices an incomprehensible rash in the perineal area, he should consult a dermatologist, he will prescribe the necessary examination and treatment. In order to determine what disease the patient has, the doctor conducts the entire course of examinations; for this you need to take a skin analysis from the site of the lesion. After this test is completed, the doctor carefully examines the outer skin. While the test result is being prepared, the patient needs to undergo the following examinations:
- The patient needs to go to the laboratory and have the outer part of the skin analyzed there.
- The doctor must examine all affected areas using a special lamp. It allows you to examine all areas of the skin.
- Pass a special test using iodine.
- The last stage is taking a culture to check for the fungus that has affected the skin of the sick man.
After the full range of examination has been carried out and all tests have been taken, if a certain type of fungus is confirmed, the doctor will prescribe the necessary treatment. This will help get rid of this disease. It is worth remembering that the main factor ensuring effective treatment of this disease is timely contact with a specialist in this field. Because if the correct treatment is not applied, the disease can become chronic, and it will be very difficult to cure.
The diagnosis is made based on the patient's complaints about rashes on the scrotum characteristic of pityriasis versicolor. To confirm, a test with iodine is performed, which in medicine is called the Balzer test. In the absence of an alcohol solution of iodine, aniline dyes can be used. Besnier's sign is also detected. It is determined by scraping the stain with a fingernail, as a result of which it begins to peel off.
If there are hidden stains, they can be revealed using a mercury-quartz lamp in a dark room. Pityriasis versicolor spots fluoresce brown.
https://www.youtube.com/watch?v=3gBSQBxbi3c
To detect the pathogen, scales containing the mycelium of the fungus are used. Identification is carried out by inoculating the test material on a Sabouraud nutrient medium to which an antibiotic is added. This method is called cultural.
Lichen versicolor is similar in clinical symptoms to other skin diseases, so it is necessary to carry out differential diagnosis with the following diseases:
- Syphilitic leucoderma. With it, the spots do not have a pale color and they are located in the form of nets. They also don't merge.
- Syphilitic roseola. There is no peeling with it. The color of the spots is pink. If you press on the stain, it disappears.
- Imbricated mycosis. It is common in the tropics. The rash has peeling, but the spot takes the shape of a ring. Characterized by rapid progression. Within a few weeks, the damage to the scrotum spreads to the entire surface of the skin.
Diagnostic features
Many symptoms of fungal diseases are similar in appearance to some sexually transmitted infections. Therefore, a visual examination by a dermatologist alone may not be enough to make an accurate diagnosis. The patient must undergo the following tests:
- scraping of exfoliated particles from the epidermis of the testicles;
- material for sowing into a nutrient medium;
- general and clinical blood tests to assess health status;
- Ultrasound if inflammation of internal organs is suspected;
- examination of the testicles under a special lamp.
Signs indicating the occurrence of a fungus
It is necessary to carefully examine this area of the body in men. The affected area becomes covered with pink spots, which later change color to yellow.
If timely treatment is not started, they will grow. The fungus can cover the entire scrotum, cover the groin and gradually affect the skin between the buttocks.
Can appear:
- Unbearable itching.
- Feeling pain.
- Peeling of the skin, which will cover the entire area and the egg as well.
After a certain time, the area affected by the fungal infection begins to turn red, and characteristic symptoms appear:
- Cracks form on the skin.
- These areas become dry and the protective properties are impaired.
- The skin begins to peel off not only in those places where there is a lesion, but also where healthy skin comes into contact with the affected area.
Main symptoms of mycosis
Pityriasis rosea on the testicles
Almost any fungal disease in the groin begins with peeling of the skin on the testicles. It resembles small powdery grains, which many men mistake for an allergic reaction to detergents. With pityriasis versicolor, such exfoliated particles are larger in size, resembling grains of ground wheat bran.
With the further development of fungal infection and inflammation on the genitals, more unpleasant and even painful symptoms may appear:
- the area affected by the fungus becomes red and swollen, the skin may have a bluish tint;
- debilitating itching appears, the skin is very itchy, sometimes there is a burning sensation;
- the skin in the groin area and testicles becomes dry and tight;
- A small or large red rash may appear.
Peeling skin on the testicles
With athlete's foot inguinal, the disease does not affect the penis, but the skin on the testicles peels off, affecting the inguinal folds. With pityriasis versicolor, large spots with a yellow tint appear, which merge into large ones, gradually turning pale and leaving severe peeling.
Most mycoses that cause peeling of the skin on the testicles are not characterized by fever and other complex symptoms. But with insufficient treatment or interruption of therapy, any fungal disease can cause serious complications in the genitourinary area and provoke inflammation of the prostate or bladder.
Signs of mycosis
Despite the fact that cutaneous mycosis is quite problematic in treatment, its manifestations are not long in coming. The problem is that the disease is prone to relapse after incorrect treatment. The disease can manifest itself in a variety of ways, but in the early stages the following occurs:
- small cracks appear on the skin in the scrotum area (on the inside of the thigh) (painful sensations depend directly on the characteristics of the body and the individuality of the case);
- the formation of bubbles is possible, due to which the skin becomes rougher and denser;
- over time, the pain may quickly pass, the skin will soften, return to its normal color and begin to peel off;
- under the condition of bacterial infection, in any case, the blisters will transform into ulcers.
All of the above signs are extremely general, but the following factors cannot be excluded: fungi on the testicles cause a feeling of itching, along with peeling off areas of the skin. Next, diaper rash appears, reddish spots appear, actively growing in size. Periodically, the spots begin to itch, causing discomfort, and all standard ointments for inflammation or disorder do not help. They only partially relieve inflammation and stress on the affected area, while the disease only temporarily stops progressing.
If left untreated, the fungus spreads to neighboring areas
Possible diseases and provoking factors
In second place after hygiene in terms of the frequency of occurrence of pathology are factors associated with infectious diseases.
Unfortunately, not every person has time to pay attention to the genital organ and the places nearby. However, in the area where the scrotum is located, the skin tissue is constantly soaked with liquid (this process is called maceration), as well as sweating. All this creates an ideal environment for the proliferation of fungi and various infections.
Below you can see diseases that can provoke the development of fungus.
Diseases that provoke the development of fungus
We should not forget about hair removal as one of the root causes of various types of rashes in the scrotum area. The skin in that area is “delicate”, and hair removal can cause irritation there, which often leads to peeling and constant itching. The allergen in this case is either aftershave cream or a razor.
Medications
As a treatment for fungus on the scrotum, the doctor usually prescribes Fluconazole. This drug is quite effective in treating fungus and various types of infections. If a person comes with an advanced disease, preventive medications and serious treatment are prescribed. In this case, the following ointments for fungus on the scrotum act as drugs:
- "Clotrimazole".
- "Miconazole".
- "Terbinafine".
Most often, ointments are prescribed as a means of preventing and treating fungus, which should be used only with the prescription of the attending physician, since self-medication can lead to the development of infection.
Types of fungal infections
Doctors identify several types of mycotic pathogens that lead to infection of the scrotum. They are divided into groups presented in the table.
| Name | Description |
| Yeast fungus | If it is detected, genital candidiasis is diagnosed. With such a pathogen, not only the scrotum is affected, but also the penis and the genitourinary canal. |
| Fungus of the species Pityrosporum | Leads to the development of pityriasis versicolor. This form of lesion is the least common. Typically, the appearance of fungus is associated with hormonal problems and increased levels of testosterone in the body. |
| Epidermophytons | Because of them, a man suffers from dermatomycosis, which looks like lichen or athlete's foot in the groin. Typically, this disease affects people who lead an active lifestyle. |
All groups of fungi that infect the scrotum are characterized by similar symptoms. So it is possible to distinguish a certain type of pathogen only through laboratory analysis.
Treatment of groin fungus in men
Redness in the groin in men
Attention! The information presented in the article is for informational purposes only. The materials in the article do not encourage self-treatment. Only a qualified doctor can make a diagnosis and give treatment recommendations based on the individual characteristics of a particular patient.
If a rash and ulcer appears in the groin, how to treat the disease? External fungal ointment helps in the fight against lichen. Treatment of inguinal dermatitis consists of several measures. In the early stages, antifungal and antibacterial ointments are sufficient, but if the disease is advanced, more serious measures will be required.
How to cure mycosis in the groin:
- Use antifungal ointment or cream. External remedies remove peeling, eliminate redness on the testicles and pubis, relieve itching, dry out the abscess and kill the fungus. The ointment is applied in a thin layer to thoroughly dried skin. The affected area is treated, including areas of healthy skin. This is necessary to avoid the spread of fungi.
- Take a course of antifungal drugs.
- Allergy medications will help with itching.
- Strengthen the immune system.
- Treat your pubic hair with an antifungal shampoo twice a day.
Antifungal ointments for the intimate area:
- Clotrimazole; Clotrimazole
- Miconazole;
- Monistat;
- Triderm;
- Mikatin;
- Zalain;
- Lotrimin;
- Lamisil;
- Terbinafine;
- Ketoconazole;
- Tinedol.
After applying the cream, the skin can be treated with zinc ointment. It will protect the skin from friction and excess moisture.
As prescribed by your doctor, you should take antimycotics in tablet form.
The doctor may prescribe:
- Fluconazole; Fluconazole
- Nystatin;
- Terbinafine;
- Griseofulvin;
- Intraconazole;
- Ketaconazole.
Inguinal athlete's foot causes unbearable itching, so you can take antihistamines:
- Suprastin;
- Zodak;
- Zyrtec;
- Diazolin.
Antifungal shampoos with the active ingredient ketoconazole are used to treat hair:
- Keto plus;
- Mycozoral;
- Nizoral;
- Sebozol;
- Akrikhin Mikozoral.
If the cause of tinea groin is a bacterium and not a fungus, the doctor will prescribe antibacterial drugs:
- Clindamycin;
- Erythromycin;
- Metronidazole;
- antibacterial soap Hibiclens, Lever 2000 and analogues.
For a serious bacterial infection, your doctor will prescribe antibiotics:
- Minocycline;
- Cephalexin;
- Doxycycline;
- Erythromycin;
- Dicloxacillin.
Types of fungi
The most pressing problem causing peeling of the skin on the testicles is various types of mycosis. Under this diagnosis, dermatologists suspect various diseases caused by pathogenic fungi of several types:
All of these types belong to the opportunistic environment of microorganisms that are present on the skin of men of any age. They end up on many hygiene and household items, remaining active for several weeks. Therefore, you can become infected with such pathogenic fungi:
- visiting public places for swimming and active recreation;
- through bed or underwear, towels;
- during sexual intercourse;
- if hygiene is not observed after visiting a public toilet or other contaminated places.
The structural features of the male genital organs do not protect or hide them from contact with an infected surface. In the groin, body temperature is physiologically higher, and sweating is common during intense movements or sports. Therefore, peeling on the testicles and mycosis are a common reason for visiting a dermatologist.
Recommendations for therapy
Before performing the prescribed procedures, the following recommendations must be followed:
- Before applying ointment to the affected area, it is necessary to thoroughly disinfect it; this requires washing the area with soap.
- The ointment must be rubbed into the affected areas of the skin, as well as areas nearby.
- The products should be used as prescribed by a doctor after reading the instructions.
- Treatment takes place within two weeks. If during this time the condition has not improved, then you need to contact your doctor again so that he can prescribe another treatment.
- It is necessary to change clothes and bedding every day, as the disease may remain. And the treatment will not come.
- If there are many affected areas, then it is necessary to treat each area so that the infection does not spread throughout the body.
The appearance of fungus can be prevented by starting treatment on time. The drugs should be used only as prescribed by a doctor and after reading the instructions. Self-medication can only worsen the situation and increase the risk of spreading the disease. It is also necessary to practice daily hygiene, which includes washing, changing clothes and bed linen.
Diagnostic methods
The doctor will not be able to select an adequate treatment for the patient without knowing what kind of fungus is affecting his scrotum. Therefore, the patient initially needs to undergo diagnostics. During the appointment, the dermatologist should carefully examine the skin that has been infected with the fungus. Afterwards, he directs the patient to carry out the following diagnostic measures:
- Laboratory analysis of scrapings from the site of epithelial damage;
- Examination of the scrotum using a Wood's lamp, which can highlight problem spots;
- Balzer test, which uses iodine;
- Culture inoculation on active medium.
Only a complete and thorough diagnosis will help a specialist correctly identify the causative agent of the infection and select an effective treatment to combat it.
Treatment
When the skin of the scrotum is affected by a fungus, patients are offered treatment, the action of which is aimed at destroying the infectious pathogen, restoring the damaged epithelium and increasing the body's defenses.
There are several effective methods of treating fungus on the scrotum, which can quickly and painlessly eliminate the signs of infection. They differ from each other in the method of application and the nature of the effect. For treatment to be effective, the patient must adhere to a number of rules and recommendations of the doctor:
- Medications with an antifungal effect should be applied only to those affected areas of the body that have previously been washed and dried with a towel;
- It is necessary to treat not only rashes, but also healthy areas that are located next to infected lesions;
- If within 10 days from the start of the treatment course neither the doctor nor the patient see obvious results of therapy, then other drugs will have to be selected;
- It is advisable to regularly wash hair that grows in the groin area with antifungal shampoo. Although it is usually recommended to get rid of them during treatment;
- Medications must be taken strictly according to instructions;
- The intimate area must be kept dry in order to deprive the fungus of the opportunity to feel comfortable in the place where it actively reproduces;
- Traditional therapy, which was suggested by a doctor, can be combined with traditional treatment if desired.
Garment processing
When the treatment is over, all clothes must be boiled and ironed. As for underwear, you need to throw it away. A man should also wash his scrotum with salicylic alcohol (2%) for 2 months. These preventive measures help to avoid recurrence of the disease. Additional measures in the fight against scrotal fungus are to strengthen the patient’s immune system. It is very important.
Judging by the reviews of those who have cured a fungus on the scrotum, a photo of which is not attached for aesthetic reasons, we can conclude that if all recommendations are followed, the disease will recede quickly.
Why does the disease appear?
A pathogenic fungus can develop its active life activity in any part of the human body. In men, it most often occurs in the groin area, since ideal conditions are created for it here. The fungus successfully activates in places where there is high humidity and heat. This is how one can characterize the constant environment in the scrotal area.
Mycosis of the scrotum in most cases is diagnosed in men aged 20-60 years. This type of epidermophytosis is encountered by those who have a predisposition to this disease due to the following unfavorable factors:
- Severe sweating at the genital area;
- Working conditions that involve being in a hot room;
- Having excess body weight;
- Disturbance in the process of carbohydrate metabolism;
- Lack or insufficient compliance with the rules of personal hygiene in the genital area.
The fungus loves a moist and warm environment, so excessive sweating increases the risk.
Infection with the fungus occurs through household and contact routes. To get sick, it is enough to touch the scrotum to an infected surface. This often happens to men who like to regularly visit saunas, baths and other similar public places.
For a long time, the fungus in the scrotum area may not show itself. The following violations help speed up its activation:
- Decreased immune system;
- Diabetes;
- Hormonal disbalance;
- Cardiovascular diseases;
- Stress.
Heavy physical work also acts as a factor that accelerates the activation and proliferation of fungal microflora on the genitals and scrotum. Such a problem cannot be avoided by a person who neglects to regularly wash the intimate area and also constantly wears tight underwear made of synthetic materials.
Herbal treatment
Additionally, herbal remedies can be used in the treatment of inguinal athlete's foot. Herbs are used in complex therapy.
Herbal medicinal preparations help relieve itching on the testicles and the front of the thighs. Herbs have an anti-inflammatory and healing effect, so they are used if the skin is cracking and inflammation appears in the skin folds.
In the treatment of inguinal epidermophytosis, herbal decoctions are used:
- strings,
- violets,
- eucalyptus leaves,
- birch trees
- oak bark,
- poplar buds,
- chamomile flowers,
- yarrow,
- St. John's wort.
Herbs are used in the form of baths or lotions. After using the herb, you need to let the skin dry.
Treatment of scrotal fungus
The treatment period for a disease such as inguinal fungus is two months, but it is possible to completely safely speed up this process. Recommendations:
- purchase and wear loose underwear, changing it daily;
- use medicinal ointments only after taking a bath and washing the genitals with baby soap;
- treat infected and near-infected areas of skin with ointments;
- to avoid genital friction, use special talcum powder;
- shave your groin hair;
- avoid sexual intercourse during therapy (this is not only to protect yourself, but also your sexual partner).
Usually effective therapy is prescribed by doctors. It includes medication and the use of special ointments. The ointment is selected solely based on the type of disease and stage of development (volume of affected tissue).
Some people decide to use folk recipes to combat groin fungus, which, in principle, only gives the desired result in 20% of cases, especially if you have not consulted a doctor.
Manifestation of the disease
The infection will begin to appear within a month from the date of infection. The onset of the disease is accompanied by a rash that looks like spots that tend to grow.
The fungus manifests itself in this way:
- the man experiences severe itching in the affected area, which only intensifies over time (sometimes even pain appears);
- the skin in the groin becomes covered with red or pink spots, which have fairly clear outlines and can change color as the disease progresses;
- the skin peels off, small cracks begin to appear on it;
- the area of the scrotum that has not been infected becomes very dry and dark;
- If a man is prone to increased sweating, then the skin on the testicles begins not only to get wet, but also to sweat.
If the disease is not treated correctly, the area of infection will begin to increase. The spots will begin to grow, gradually merging into one large spot, which can even reach the buttock area, become covered with purulent discharge and bubble.
It is important! Since the infection cannot cause inflammatory processes, body temperature and the condition of the lymph nodes remain unchanged.
Symptoms
Symptoms of fungal infection of the scrotum in men begin to appear 14-30 days after the patient is infected.
The main symptom of the disease is rashes that appear in the form of spots. Fungal rash has its own characteristics:
- Color. The fungus can be yellow, brown or brownish-pink (as the pathology develops, the rashes become colorless).
- The affected area peels off and cracks may appear over time. If peeling does not appear on the surface of the skin, then an iodine solution (5%) is applied to this area. Infected areas of the skin quickly absorb iodine, so the spots become easy to distinguish from healthy skin.
- Itching. With this disease, men experience severe itching in the groin area. This symptom can become painful over time.
- The anal area may also itch.
If the patient does not begin drug treatment for this disease in time, the fungal spots can greatly increase in size, and their entire surface will eventually become covered with ulcers with liquid. Treatment generally lasts about 2 months, and if a man is not fully treated, there is a high probability of a relapse.
Prevention
People with excessive sweating and cases of the disease in the family are prone to lichen versicolor. Therefore, they should adhere to a number of rules:
After the course of treatment is completed, all the patient’s clothes are boiled and ironed with a hot iron. It is recommended to change underwear to new ones. Also, the scrotum must be wiped with 2% salicylic alcohol for two months. These measures serve to prevent relapse of the disease. It is imperative to strengthen the immune system through hardening and taking vitamin complexes.
Despite the fact that testicular fungus is a low-contagious disease, to prevent transmission of infection, a sick person should use separate hygiene products and not share their clothes with others.
Source
Nail fungus. Vinegar, egg as treatment methods
Onychomycosis is a disease that causes a person a large number of problems and troubles. The disease mainly affects the feet, and therefore if you have nail fungus, vinegar and eggs will become your helpers in the fight against the disease. Today in the pantry of traditional medicine recipes there are many that are based on the use of eggs and vinegar.
Treatment of onychomycosis with vinegar
Standard methods of treating nail fungus may not always bring the patient the desired result. In addition, the disease is simply insensitive to many medications, and therefore all efforts may be in vain. Meanwhile, the nail will remain the same and will not look aesthetically pleasing. Another important fact is that medications are allowed to be used for a certain amount of time so as not to cause harm to health.
The main recipes against nail fungus based on the use of vinegar include:
- Foot baths - 0.5 liters of 9% vinegar should be heated, poured into a basin and lowered the feet there. To ensure that the damaged area is completely covered with liquid, place the basin on a slope. Keep your limbs in vinegar for at least 15 minutes. You can wear socks at night, or better yet, if they are soaked in wine vinegar.
- Apple cider vinegar mixed in equal proportions with iodine has a good effect in the fight against onychomycosis. This mixture should be applied to the damaged area twice a day until healthy nails grow back.
- Apple cider vinegar with vegetable oil - these two components are mixed in equal parts and a cotton swab is soaked in the resulting product. Then it is applied to the affected nail plate and sealed with an adhesive plaster. All this is secured with a sock and left overnight. Repeat sessions until complete recovery.
- Vinegar with carrots - mix carrot juice and vinegar essence and smear the skin and nail plate. Vinegar has a destructive effect on the fungus, and carrots restore the epidermis.
- Vinegar with egg - take 2 tbsp. vodka and vinegar essence, as well as 3 proteins. Everything is thoroughly mixed in order to lubricate the nails with fungus twice a day until the plate is renewed.
- Vinegar with dimethyl phthalate - mix 1 tbsp. dimethyl phthalate with the same amount of vegetable oil, 1 egg. The resulting mixture is added to 2 tbsp. essences. The product should be lubricated on the affected areas in the evening. After the mixture is applied to the nail, a bag and socks are put on top.
I would like to note that therapy using vinegar is allowed only if there are no abrasions, open wounds or lesions of the epidermis. If acid penetrates the wound, it will be at least unpleasant.
In this case, slight tingling and tingling is allowed, which will mean that the vinegar is working and the infection is dying. In addition, different skin reacts to these components in its own way - sometimes it peels and turns red (especially when using concentrated acid solutions).
Preventive measures
To prevent infection with onychomycosis, you need to pay attention to some rules of prevention:
- actively combating sweating of the feet;
- daily change of socks and tights;
- washing hands and feet every day with soap (preferably laundry soap);
- having light, replaceable shoes at home and at work;
- going to public baths, swimming pools and beaches only with your own slippers;
- After taking a shower, you need to dry your feet/hands well.
If you notice the first symptoms of the disease, immediately begin its treatment, since it poses a danger not only for you, but also for others.
https://youtube.com/watch?v=3gBSQBxbi3c
Drug therapy
When treating genital fungus, it is important to follow some rules to avoid complications that are so undesirable in this case:
- before applying the ointment, the skin should be thoroughly and gently washed with soap, if possible antibacterial;
- when treating mycosis of the inguinal folds, external agents should affect not only the affected areas, but also the area around them;
- recommendations in the instructions must be strictly followed;
- after two weeks, the condition of the skin should improve significantly; if this does not happen, you need to visit a dermatologist, he will prescribe additional medications, in particular, internal ones;
- during treatment of groin fungus, preference should be given to loose-fitting underwear made from natural fabrics (cotton, bamboo), which should be changed daily;
- since the fungus between the legs loves moisture, it is necessary to maintain dryness in this area with the help of powders and talcs;
- if there is hair on the intimate area, it must be washed using an antifungal shampoo.
To treat inguinal fungus, antifungal agents are used, such as Clotrimazole, Ketoconazole, Terbinafine. Inguinal fungus in advanced form requires intensive therapy, since the inflammation is pronounced.
Prevention of fungal infections
The most common infections this pool and heat season are dermatophyte infections, which only affect areas with keratin, such as hair, nails and the surface of the skin; Athlete's foot is the most common of all, presenting, like other types of mushrooms, various signs such as desquamation, maceration, blisters or blisters, sores or whitish areas, cracks, itching, bad odor or even pain.
Folk remedies for fungus
If proper hygienic conditions are not maintained, fungi can remain or grow in chlorinated water despite poor survival in them. The next minimum hygiene standards are to prevent the development of dermatomycosis. To prevent a yeast infection, follow these tips.
The following tools are suitable here:
- glucocorticoid ointments with anti-inflammatory effect - Clotrimazole, Triderm, Miconazole;
- drugs for internal use with antifungal action - Nystatin, Itraconazole, Ketoconazole, Fluconazole.
It is strictly prohibited to prescribe medications to yourself; the prescription should only be carried out by the attending physician after consultation.
Always use flip-flops or rubber sneakers to isolate your foot from moisture or groundwater, as this is where fungi are most likely to grow. This action removes most microorganisms from our skin. Dry after bathing. With special care in the folds of the skin and the spaces between the fingers.
Excessive sweating increases the likelihood of developing fungi. You can use special products that reduce moisture caused by sweating, such as talcum powder. Do not exchange textiles or shoes with other people. There are people who may be carriers of fungi and do not know it because they have no symptoms or signs.
As for the duration of therapy, fungus in the groin area is treated for two months, no less. Untreated mycosis will definitely return after some time. Control tests should confirm the absence of infection in the body.
Treatment
Self-medication of versicolor versicolor is contraindicated. Before carrying out a course of therapy, you must visit a doctor and make sure that the diagnosis is true.
Treatment can be carried out either at home, provided that all recommendations of the dermatologist are followed, or in a hospital.
When the process is localized only on the scrotum, therapy is carried out locally. The scrotum must be wiped with one of the following preparations:
Wiping is carried out for two weeks. Along with them, keratolytic agents are prescribed. The most effective drug is Arievich ointment, which contains salicylic and lactic acids. The basis of the ointment is Vaseline. It is used in the form of an occlusive dressing, which is sealed and prevents the penetration of air.
If the disease is severe, the Demyanovich method can be used. It consists of alternately rubbing a 60% sodium thiosulfate solution and a 6% hydrochloric acid solution into the skin of the scrotum. Despite the fact that this method was developed for the treatment of scabies, it is actively used for lichen versicolor. In addition, benzyl benzoate is rubbed into the skin of the scrotum (also used to treat scabies).
General therapy is prescribed when local drugs are ineffective. The patient should take ketoconazole 1 tablet per day (Be sure to get individual instructions from the doctor! Do not calculate the dosage yourself). The course of treatment is also two weeks. After a two-week course of therapy has been carried out, physiotherapy - ultraviolet irradiation - is prescribed to eliminate the spots.
The entire course of treatment must be accompanied by general measures:
Factors influencing the occurrence of the disease
The onset of the disease may be influenced by any of the following factors:
- Increased sweating, failure to comply with personal hygiene rules. In other words, a humid and warm environment.
- Disturbance of the metabolic process in the body.
You can become infected through contact with an infection, that is, after sharing a washcloth or towel in public.
In addition, infection awaits a person in crowded places, such as a swimming pool, bathhouse, sauna, or hospital. In the latter case, the risk of disease is associated with the use of a hospital duck.
It is easy to determine the occurrence of an infection; spots appear on the scrotum that differ in color from normal skin. They have a yellowish tint. If you examine this area under a microscope, you can see that the testicle is covered with entire colonies of fungi.
Diseases of the groin area of a non-fungal nature
Intertrigo (diaper rash)
Mechanical dermatitis or diaper rash appears as a result of friction, pressure, heat, etc. Diaper rash can appear in all folds of the human body.
The skin is damaged by skin secretion products, which is manifested by diffuse redness with areas of maceration and the formation of blisters. The upper layers of the epidermis are involved in the process. The lesion has no clear boundaries. In advanced cases, areas of skin damage and cracks appear. Pain and itching occur. Diaper rash can be complicated by bacterial and fungal infections. Rice. 20. Diaper rash in the groin area.
Rice. 21. Diaper rash in the groin area.
Rice. 23. Colonies of Pseudomonas aeruginosa.
Rice. 24. Pseudomonas diaper rash.
Rice. 25. Pseudomonas diaper rash.
Rice. 26. Pseudomonas diaper rash.
Erythrasma
A bacterial disease caused by Corynebactcrium minutissimum.
The trigger is increased sweating or frequent washing with soap, which weakens the “acid mantle” of the skin, increased ambient temperature and humidity. Erythrasma looks like red-brown spots with jagged edges and peeling. The itching is minor. With excessive sweating, the spots become red, swelling and blisters appear. Rice. 27. Erythrasma of the inguinal region.
Rice. 28. Erythrasma of the inguinal region.
Psoriasis
A disease with an unknown nature of the occurrence and development of the pathological process.
Very rarely it affects the groin area and genitals. Rice. 29. Psoriatic lesions of the genital organs.
Pemphigus
A disease with an unknown nature of the occurrence and development of the pathological process.
The disease is believed to be caused by retroviruses. Autoimmune processes occurring in the body lead to the destruction of the spinous layer of the epidermis. When the process is localized in the groin area, short-term blisters appear. After their disappearance, painful erosions and fragments of epithelium remain. Rice. 30. Pemphigus. Bullous pemphigoid.
Rice. 31. Pemphigus. Chronic benign familial pemphigus Hailey-Hailey.
Inguinal rubrophytosis
Rubromycosis in 90% of cases is caused by the fungus red trichophyton (). The fungus got its name for its ability to form a red pigment when growing on Sabouraud's nutrient medium. The wide distribution of fungi in the environment is the cause of frequent human mycoses. Rubrophytosis affects the skin of the feet and hands, interdigital spaces and nails. The skin of the face, head, torso and groin folds is slightly less commonly affected. The infection is spread by the patient himself. It is also transmitted through his personal belongings. When a patient with rubrophytia appears in a family, all its members very quickly become ill. Rubrophytia is often called a “family disease.” Pathogenic fungi spread quickly in public places where it is warm and damp - in swimming pools and baths. Excessive sweating, obesity, diabetes, decreased immunity, wearing tight clothing, living in conditions of high humidity and long-term use of hormonal and antibacterial drugs are trigger factors for the development of the disease . The disease lasts a long time and often becomes chronic. The disease often takes a protracted, chronic course.
Skin manifestations of rubrophytosis
The disease manifests itself in the form of an erythematosquamous and follicular-nodular form. The erythematosquamous form is manifested by the appearance of large spots, on the surface of which papules (seals) and vesicles (bubbles with liquid) are visible. Dilated capillaries give the affected area a reddish color with areas of peeling. The affected area becomes covered with crusts over time. The lesion is surrounded by an intermittent ridge, on the surface of which papules and vesicles are visible. The boundaries are clearly defined. In the center of some lesions you can see the resolution of the process, which has a brown, yellowish or bluish color. The follicular nodular form of rubrophytosis is a continuation of the development of the previous form as a result of the lack of proper treatment.
Diagnostics
To diagnose the disease, it is necessary to make a scraping from the peripheral zone of the lesion, since this is where the fungi are found in large quantities.
Under microscopy, scrapings from the affected area reveal the mycelium of the fungus. Drop-shaped microconidia are located on the sides of the mycelium. When growing on Sabouraud's nutrient medium, Trichophyton rubrum deposits a red pigment. The infection usually spreads from the feet to the groin, as the fungus can travel in the hands or on a towel. Inguinal ringworm causes a rash of red, raised, and scaly patches that may blister and drain fluid. The patches are redder around the outside, with normal skin tone in the center, forming a ring with well-defined edges.
- The lesions cause a lot of itching.
- The edge of the rash may consist of a line of raised small blisters.
There is a risk of acquiring inguinal ringworm if.
Systemic treatment of groin fungus
Rigid underwear He is overweight He sweats excessively, which removes protective oils from the skin and makes it more susceptible to infection. Weakened immune system Suffering from other skin diseases such as atopic dermatitis. This is a man or a young teenager. . A doctor can usually diagnose inguinal ringworm simply by observing the rash. If the diagnosis is unclear, the doctor may take samples of the skin or infected area and send them to a laboratory for analysis.
Rice. 6. Under a microscope, the mycelium of red trichophyton is visible.
Rice. 7. Trichophyton rubrum colonies on Sabouraud nutrient medium.
Rice. 9. Microscopy. The mycelium of the fungus Malassezia furfur is visible.
Rice. 10. Colonies of the fungus Malassezia furfur on Sabouraud nutrient medium.
Rice. 11. Type of lesion in pityriasis versicolor.
Rice. 13. Microscopy. The mycelium of the fungus Candida albicans is visible.
Rice. 14. Candidiasis of the groin area.
Rice. 15. Candidiasis of the anogenital area.
Rice. 16. Candidiasis balanoposthitis.
Rice. 17. Candidiasis of the groin area. Along the periphery, areas of the exfoliated stratum corneum of the epidermis are visible.
Rice. 18. Candidiasis of the groin area. A mushy mass of exfoliated epithelium is visible, accumulated in the depths of the folds.
Rice. 19. Candidiasis of the groin area. Multiple blisters and pustules are visible.
How to carry out treatment correctly
During treatment of the disease in men, they need to follow certain recommendations, which will determine the outcome of treatment:
- Before applying antifungal ointment to the affected area, the scrotum and adjacent healthy area of skin should be washed with soap.
- The ointment should be applied to the area affected by the fungus and to healthy skin nearby.
- It is necessary to use medications after reading the instructions.
- If after fourteen days the fungus does not recede, contact the doctor again so that he changes the method of therapy.
- During treatment, you need to wear clean clothes and change bed linen every day.
- If the fungus affects not one area, but several that are not in contact, treat all foci of the disease, because it can eventually cover the entire skin.
If the disease is not treated, then over time, even if you have a normal level of immunity, it can develop into a chronic form, and will develop on the scrotum for several years.
Treatment of the disease
When the first symptoms of a fungal infection appear on the scrotum, treatment should be started as soon as possible. But before that, you need to visit a doctor so that he makes the correct diagnosis.
It’s easy for an experienced specialist to do the following:
A scraping made in men at an “interesting” place will help make an accurate diagnosis, and then decide on the method of therapy.
Treatment of such a disease usually occurs with the use of complex therapy. To do this, the doctor prescribes antibiotics and medications for internal use (tablets, capsules), as well as topical medications (creams, ointments, gels). In addition, medications are prescribed that can boost and strengthen the immune system. All this must be strengthened by regular hygiene of intimate places.
It is important to understand that the entire course of therapy must be completed, even if the symptoms have disappeared. Some patients do not adhere to this advice and quit treatment at the first improvement. Such actions threaten new occurrences of the disease in men, and the fungus may become much more resistant to medications.
In general, the duration of treatment for the disease takes approximately two months. But in addition to treatment, you must adhere to some rules. For example, underwear should be made of natural material and be loose, that is, it should not tightly fit the groin area so that the scrotum does not sweat. Because humidity is a favorable environment for the proliferation of fungal spores.
Recommendation. You can avoid moisture and diaper rash in the scrotum by using talcum powder or powder, which have an antifungal effect.
Your doctor may prescribe fluconazole as a medication; this drug is most often used to treat fungus. In addition, it is effective against almost all types of infection.
The doctor also prescribes anti-inflammatory drugs to relieve redness in this area. If no ulcers or pustules appear during the development of the disease, you can treat the affected area with an iodine solution. But you shouldn’t get too carried away, because you can get burned. Treatment in this method can be carried out as follows: for a week, iodine must be applied twice a day, and then an antifungal agent for another five days.
If the patient seeks help with an already advanced disease, medications are prescribed that can quickly relieve inflammation. Basically, these are ointments: