Human papillomavirus is one of the most progressive diseases. This is the scourge of our time, and this disease is on a par with HIV. More than 70% of the planet's population is already infected with it, and every year the number of infected people increases by tens of thousands. The virus itself is dangerous only in certain cases. The main thing is, if you notice new growths on the skin, consult a specialist. Using HPV screening, doctors determine the type of virus and its degree. Only after such a high-tech analysis is the patient prescribed therapeutic therapy associated with the use of antiviral and immunostimulating drugs. The doctor also gives recommendations on how to remove tumors.
HPV screening shows the strain and concentration of the virus
What it is
Based on the studies conducted, it was revealed that in more than half of the cases, the development of cancerous tumors of the genital organs in women is due to the activity of pathogens from the papovirus family. Penetrating into the body, pathogenic flora can remain in an anabiotic state for years without causing the appearance of external signs of invasion.
Under the influence of favorable factors, for example, against the background of chronic diseases, a decrease in immune strength, the virus is activated, provoking the appearance of growths, warts, condylomas, and malignant neoplasms. Not all members of the family, which numbers about a hundred names, are dangerous. Only strains of the virus that cause cancer can provoke the growth of malignant tumors.
HPV screening is used to detect the presence of papillomavirus, as well as determine the carcinogenic risk of HPV. Everyone needs to know what it is, since this diagnostic method is the only one that will help identify infection in the early stages of development. HPV screening combines three main diagnostic methods, which, in addition to the above factors, make it possible to determine the amount of virus in the body and the resistance of pathogenic flora to certain drugs.
The screening procedure begins directly with the collection of biological material for research in the laboratory. Cervical mucus, amniotic fluid, blood, urine, saliva, and scrapings of the epidermal layer can be used for diagnosis. After the study, not only the presence of the virus and its type is determined, but also the risk of developing a malignant tumor.
What to do with screening results
As soon as a person receives his results, he needs to consult a doctor. The analysis form contains 2 scales (with negative and positive results). The specialist looks in which column the result for a particular type of virus is located, makes a diagnosis with an accuracy of 99% and determines a treatment method suitable for a particular case.
Treatment usually involves removing the external manifestations of HPV (papilloma). This is carried out using a laser, cryodestruction, radio wave method, and electrocoagulation. Papillomas are practically not removed with a scalpel due to the high level of trauma to the skin and the possibility of the formation of a large amount of scar tissue. Surgical removal of papillomas using a scalpel is performed only in case of their large growth or tendency to malignancy.
IMPORTANT! Human papillomavirus is not as safe a disease as it seems at first glance. It not only causes aesthetic discomfort in the form of warts, but can transform into cancer. Unfortunately, no way has yet been invented to completely destroy the virus or prevent its appearance. Even the use of barrier methods of contraception will not protect against the penetration of the virus. Only regular screening and strong immunity will help suppress the development of HPV.
HPV screening should be performed on every person under 30 years of age at least once. If the result is positive, then the procedure will need to be carried out regularly. This is necessary in order to promptly recognize the tendency of affected cells to become malignant and thereby prevent cancer at an early stage or prevent the virus from degenerating into an oncological disease.
Is screening reliable?
HPV screening is a complex procedure that combines several options for laboratory tests, the combined use of which makes it possible to determine the presence of pathogenic flora in the body, the type of infection, as well as the viral load. To obtain more informative results, a double application of this diagnostic procedure is required.
If, after the initial examination, the papilloma virus is detected in significant quantities in the patient, appropriate treatment is possible. After therapeutic procedures, repeat HPV screening is required. If the infection is detected again, there is a possibility of developing a malignant tumor; of course, this is only possible against the background of invasion by strains of the virus with high oncogenic activity.
Features and classification of HPV
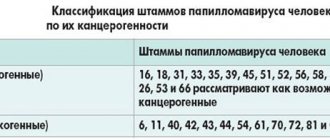
No one is immune from getting HPV into the body. People who often change partners and have a promiscuous sex life are at risk. A mother with HPV is more likely to infect her baby during childbirth. Visiting swimming pools, saunas and baths can also cause infection. The virus can have a benign and malignant course. There are more than 40 species, which in turn are divided into 3 groups.
Non-oncogenic
These include HPV types 1, 2, 3, 5.
With a low oncogenic risk level
These include types such as 6, 11, 42, 43, 44.
High-risk HPV
These are types 16 and 18. HPV type 16 leads to cancer in 40-50%, integrating into the DNA gene and causing pathological degeneration of tissues. In 90% of cases, HPV becomes the impetus for the development of cervical cancer, in 40% of cases it leads to cancer of the vagina, vulva and penis. In 15% of cases, infection can cause cancer of the larynx or oral cavity. Women are 300 times more likely to develop cancer from papillomas than men. Sometimes the presence of HPV can be disguised as various diseases, which does not always allow timely treatment to begin. Therefore, when papillomas are detected, it is necessary to conduct an HPV screening to obtain reliable information about the patient’s health status.
A screening examination allows you to identify individuals who are at risk in order to timely diagnose precancerous and cancerous pathologies.
Indications
Due to the prevalence of the HPV viral infection, screening is increasingly acquiring the status of a preventive diagnostic procedure, which everyone needs to undergo once over several months. Persons with an active, promiscuous sex life, women over forty years of age, as well as people suffering from chronically weakened immune systems are recommended to undergo examination at least once every six months.
Today, HPV screening is prescribed more often against the background of existing manifestations of papilloma virus activity, for example, when growths and warts appear on the skin. Timely identification of pathogenic flora, determination of its type, as well as sensitivity to drugs will allow timely detection of infection and prevent negative consequences through timely treatment.
What is HPV screening and how is it done?
This is a special medical strategy that aims to identify cancers associated with HPV. The main goal is a massive study for early detection of the presence of a virus in a person and timely control of it. For this purpose, special diagnostic techniques have been developed, which, if the patient consults a doctor in a timely manner for diagnosis, can reduce the risk of developing cervical cancer by a thousand times. Using certain developments, it is possible to identify a carcinogenic type of virus and prevent its further development.
The most effective is PCR testing. Studies are carried out on women after 25-27 years of age, and then repeated tests are carried out every 5 years. If, in the presence of the virus, no signs of pathological changes in tissue are found, then there is no need for treatment of cancer. After a year, re-screening is required. If the virus remains in the body and multiplies vigorously, the doctor prescribes appropriate treatment.
Preparation before screening
In order to obtain informative objective results of HCR HPV screening, it is necessary to follow certain rules for preparing for this type of research:
- You should not use suppositories or douching solutions that have antibactericidal properties at least one day before the scheduled procedure.
- The study is required no earlier than three days after the completion of the active phase of the menstrual cycle.
- If the study is carried out on a man, the patient should avoid going to the toilet at least two hours before the collection of biological fluids.
- Three days before the start of the research, it is important to stop eating spicy, fatty, spicy foods, exotic foods, and alcohol.
Immediately on the day of the procedure, you should refrain from using any intimate hygiene products.
How can you become infected with HPV?
The main route of infection is sexual. You can become infected through vaginal, oral and anal sex. Therefore, the presence of human papillomavirus in one partner requires examination of the other.
There is also a contact and household route of infection. This route of infection is possible through contact with the personal belongings of the patient or carrier. People often become infected when visiting public places: swimming pools, public transport (holding handrails), public showers and toilets.
Another route of transmission of HPV is vertical - from mother to child. The placenta tissue is permeable to the virus, so it easily penetrates through the bloodstream into the fetus. Also, a child can become infected during natural childbirth while passing through the birth canal.
Types of screening
HPV screening includes a whole range of laboratory tests, the combined use of which allows one to obtain informative results about the presence of the virus in the body, the viral load, and the type of infectious flora. The main methods used in this study are:
- PCR method.
- Extended HPV screening.
- PAP test.
In some medical institutions, along with the above methods, HPV screening also includes the use of the Daijin test. This method is one of the most modern, informative and reliable. A significant disadvantage of this method is the high price, as well as the possibility of performing it only in large medical centers.
Pap cytology test
The cytological pap test is a method that is used to identify atypical, that is, degenerated cells of epithelial tissues in the obtained samples of biological materials. For the study, tissue is collected from the cervix, which is pre-cleaned to obtain the highest quality samples. The tissue collection process is quite unpleasant, but painless.
A cytological pap test involves the visual determination of changed cells in a laboratory after applying liquid samples to special glasses. This technique allows you to determine the presence of atypical cells and viral organisms in tissues. However, the method is not very informative for determining the strain of viruses.
Advanced Screening
Extended HPV screening involves determining not only the presence of the papilloma virus in the blood, but also the infectious load on the body, assessing the likelihood of barely existing growths degenerating into malignant formations, that is, the oncogenic nature of the pathogenic flora. From a medical point of view, the technique is especially valuable, since in addition to the above, it allows one to determine the level of sensitivity of pathogenic flora to a number of drugs.
PCR analysis
If HPV is detected in samples of biological materials, the patient is prescribed to undergo a test called polymerase chain reaction.
What it is?
This method is one of the most informative if the goal of the study is to identify the virus strain, infectious load, and oncogenic affiliation of HPV. In addition, this method allows you to obtain data on the sensitivity of the detected HPV to the action of certain medications.
Papillomavirus screening and basic investigations
Diagnosis is an important measure that allows you to identify HPV in the early stages of infection of the body. Modern high-tech tests can show whether there is a tendency to develop malignant tumors. Doctors recommend regular examinations. This is especially true for women. Screening is carried out once - before the age of 30 years. If the result is unsatisfactory, it is recommended to undergo a repeat test.
Even if a person undergoes a therapeutic course of treatment and gets rid of the problem, he still needs to systematically visit a specialist for diagnosis. Typically, such manipulations take place once every 3 years.
Screening for HPV
Screening is an integral part of diagnostic procedures related to preventing the development of cancer. For women, the analysis is taken by collecting biological material - a smear from the surface of the cervix. This operation is not dangerous and painless. The only thing that needs to be provided is the days suitable for analysis. The procedure cannot be performed during menstruation. Thanks to modern medicine, the analysis result is almost 100% accurate. There is no need to re-screen. If, according to the results of the analysis, the presence of at least one type of HPV is confirmed, the doctor will prescribe additional studies of a narrower profile.
The results of the screening form the basis for the treatment recommended by the doctor.
Types of screening
The screening itself can be carried out in several ways:
- Cytological PAP test (liquid type),
- Extended view screening,
- Chain reaction (PCR analysis).
The exact type of screening that a person infected with HPV needs to undergo is determined by the doctor. Papillomavirus has more than 130 varieties. Each individual type of study allows you to indicate the tendency of cells to transform into a malignant tumor.
PAP test
Pap test - what is it? This is an analysis of biological material - cervical scraping. After it is collected, the material is placed in a special liquid. This combination of skin cells and transport medium gives more accurate results than the conventional cytological method.
The advantage of the liquid method is the number of possible tests that can be performed using one biological material. This is achieved due to the special composition of the liquid medium. It is this method that makes it possible to identify and detect HPV at the earliest stages of its existence in the human body. The analysis itself is carried out using the Bethesda method. The result of this is an assessment by which the doctor determines further actions, further diagnoses or prescribes treatment. This method is used only in some countries, such as the USA and Great Britain, mainly in women over 30 years of age.
Pap test, cervical scraping analysis
Advanced Screening
Advanced screening determines oncogenic HPV types and the number of infected cells in the body. About 50 of these are known. And HPV HCR cervical screening identifies 15 dangerous types of the virus. Domestic medicine does not have the appropriate equipment, so the IF indicator in our country is 12. If the test results for the presence of the virus are negative, this does not mean that the person is healthy. His body may be susceptible to the remaining three types of IF. The viral load is determined from a combination of indicators of all types of HPV, so this indicator will not be accurate. What is very important is that there is a high carcinogenic risk of cancer from complex types of the disease. Therefore, doctors often advise undergoing another screening test.
Polymer chain reaction assay
PCR analysis is a completely different study. Diagnosing HPV using this method allows you to test biological material for the presence of all types of the virus, without any specific exception. The polymer chain reaction does not require the detection of antibodies of the causative agent of the disease, but immediately identifies the virus. Thanks to this method, PCR results are more accurate than with a conventional cytological test.
The very principle of the study of a polymer reaction is to mix the cells of the pathogen and the reagent. Due to the reaction of the liquid to the nucleic acid, the test result will be 100% accurate.
DNA polymerase increases the number and volume of microbial microorganisms. At the same time, the number of polymers is increasing. Such operations are performed until the virus can be seen through a microscope. Such studies are inexpensive and simple, so they are carried out in many laboratories of domestic medical institutions. To carry out such an analysis use:
- DNA Matrix,
- elements connecting the ends of the biological material used,
- DNA polymerase
- chemical excipients,
- solution to create the required conditions for analysis.
The study itself consists of three main stages: elongation, denaturation and annealing. The analysis is performed in a circular manner up to 35 times, depending on the factors of a particular case.
In addition to detecting HPV, microorganisms of other diseases can also be determined in this way: chlamydia, candidiasis, HIV infection, mycoplasmosis, etc. The results are 100% accurate.
PCR analysis allows you to see the virus under a microscope
Advantages of the polymer chain reaction method
If we compare the polymer reaction method with other types of research, we can highlight the following advantages:
- Highly efficient. The polymer reaction assay is highly sensitive. Even a poorly taken sample will show a 100% high-quality result.
- Any type of biological material is suitable for polymer chain reaction research. To detect HPV, you can use: saliva, genital secretions, a drop of blood or skin cells. Most often, scraping of the damaged area of the epithelium is used.
- Quick results. When testing material for the presence of HPV, the result will be known within 4-5 hours after the end of the procedure.
- High accuracy of indicators.
- Possibility of determining several types of HPV from one biological sample. Such a study allows you to save not only time, but also money spent on diagnostics.
- Even a comprehensive polymer chain reaction examination has an acceptable cost.
- Availability. Such studies can be carried out in almost every medical laboratory.
Polymer chain reaction analysis is the most advantageous option for testing for the presence of HPV in the human body. This is due to the accuracy of the result and the ability to identify all types of the virus.
To test for PCR, it is enough to donate blood
How to do HPV screening: sampling rules
To avoid distortion of results, a number of rules are followed when collecting material for examination. When taking a smear from the cervical canal, a special instrument is used - a soft small brush. Previously, the Volkmann metal spoon was widely used, but now it is practically not used. The doctor inserts the brush into the cervix and makes several rotational movements. Next, the brush is carefully pulled out and placed in a sterile container to be sent to the laboratory.
What is HPV screening in gynecology? Sampling for histological examination is a more serious procedure. In essence, it is a microscopic surgical intervention.
Therefore, after histological detection of HPV, physical activity, swimming in the pool or sea, and excessive exposure to the sun are prohibited. Also, immediately after the examination, you should not take blood thinning medications (Heparin, Warfarin), or any medications in the form of vaginal tablets, suppositories, gels, or ointments.