One of the most common dermatological pathologies is fungal infection of the interdigital areas on the toes.
The disease is characterized by the appearance of an unpleasant odor, cracking of the skin, peeling and constant itching, which is why every infected person wants to get rid of it faster.
You can eliminate the problem at home using effective folk remedies and pharmaceutical preparations.
Types of mycosis
Let's look at it below:
- what is fungus between the toes;
- what drugs are used for medicinal purposes;
- what are the consequences of a disease left to its own devices?
The disease is classified as a fungal infection, affecting the fingers and feet, and the main cause is considered to be a lack of hygiene; whether these statements are true is worth investigating.
The pathogen that causes the disease, like any fungus, is divided into:
- yeast;
- dermatophytes;
- moldy.
The areas most likely to become infected are public places with high humidity:
- swimming pools;
- shower in the gym;
- bath;
- visiting slippers;
- beauty saloon.
There is no exhaustive list of places, non-visiting of which is guaranteed to eliminate fungus between the toes from a person’s life.
You can become infected with the parasite even at home; one of the members of the family can get sick and, through skin that has fallen on the carpet, transmit toe fungus to others.
Even minor diaper rash can provoke the development of fungus, so it is extremely important to monitor hygiene.
The area between the toes is ideal for parasite activity: sweat, heat, inaccurate washing, all this makes toenail fungus between the toes the most common among all types of fungus.
Both traditional medicine and medications promise a quick cure, but not everything is so simple.
Why are the feet most often affected?
Various fungi are always present on the skin. Their reproduction is inhibited by beneficial bacteria and skin secretions. If there are disturbances in the functioning of the immune system, shifts in the composition of the skin microflora, a favorable time arises for fungi - they can multiply unhindered. Regular injuries can serve as entry points for infection:
- scratches;
- cracks;
- chafing.
Another cause of mycoses is edocrine disorders. When the endocrine glands malfunction, not only the balance of hormones changes, but also the functioning of the entire body. In particular, the composition of skin secretions changes, causing them to lose their bactericidal properties. Fungi can feed on them, which also promotes reproduction.
Other factors also contribute to the weakening of protective forces:
What to do if you have a fungus?!
Read more >> |
- nutritional exhaustion (malnutrition);
- avitaminosis;
- excessive physical and psycho-emotional stress;
- concussions;
- regular stress.
All of these are nonspecific causes of fungal skin lesions. Because of them, mycosis of the feet, smooth skin on the body or mucous membranes can develop.
In addition, there are special types of fungi (genus Trichophyton or Microsporum) - pathogenic (pathogenic). When they get into the skin or on its surface, they cause disease. In the case of feet, the disease is called rubromycosis. On the body, these pathogens form specific spots - lichens. You can get infected from a person or animal.
The skin of the feet is a special place for fungi. There are always a lot of dead cells here. Microbes are used for shelter and food. The growth of the fungus is promoted by sweating feet. In closed shoes, a moist environment rich in nutrients is formed on the feet - the “dream” of every fungus. If a person neglects foot hygiene, does not dry or disinfect shoes, the infection first multiplies in them, and then spreads to the “owner’s” feet. Poor-quality hygiene products, dryness, synthetic socks also contribute to the spread of fungal infection.
Stages of fungus
Fungus on the toe can remain dormant for months, and sometimes years, without entering the development stage.
From the moment of infection to the development of a full-fledged colony, the fungus goes through several stages. If at first treatment at home helps, then at the end you need to see a doctor and spend money on expensive drugs.
Each stage has its own symptoms that are worth paying attention to.
The initial stage of the fungus:
- small skin cracks;
- itching in the area of the thumb and little finger;
- peeling of the skin.
At the first stage, the symptoms are invisible, which is very dangerous; sometimes a person simply scratches his leg with his hand, without paying attention to it, and then scratches his hand or another part of the body, spreading the pathogen throughout the body.
Second stage of development:
- appearance of red and white spots;
- bubbles with clear liquid between the fingers;
- peeling of the skin is noticeable on socks;
- the appearance of corns;
- general coarsening of the skin of the leg.
The feet are constantly peeling and itching; if you scratch them, a second of relaxation is replaced by a painful burning sensation; sick people scratch the skin between the toes until the meat is raw, greatly aggravating the situation.
Last stage:
- wet fungus appears;
- places affected by the parasite are covered with purulent abscesses;
- the skin peels off on its own;
- my legs bleed and hurt a lot.
At the last stage:
- purulent blisters constantly burst;
- the area between the fingers rots;
- nails peel off on their own
- areas of the skin near the epicenter of infection are covered with a white coating.
If the disease has reached its climax, then it is too late to buy an ointment for the fungus between the toes from an advertisement; you must urgently consult a doctor so as not to lead to blood poisoning and gangrene, followed by amputation of the limb.
The manifestation of any of the above symptoms should alert a person; it is necessary to urgently consult a dermatologist for timely testing and accurate identification of the problem.
If doubts arise on the topic: “is there interdigital fungus on the feet,” the treatment of which is necessary, there is an old folk method for determining it:
- make a bath with a very weak solution of manganese;
- put your feet down there;
- healthy skin will turn pink;
- the affected skin, with the parasite, will remain white.
In 70-80% of cases, even an absolutely healthy person, with healthy skin color on his legs, discovers that he has a fungus when undergoing tests.
Hygiene
To avoid having to deal with this disease, follow a few rules:
- It is necessary to wash your feet with soap several times a day. Laundry soap is ideal for this, as it kills all germs;
- dry your feet with a disposable paper towel or use a hairdryer:
- use antifungal ointments periodically;
- wear new, clean socks every day;
- shoes must breathe;
- treat the inside of your shoes with vinegar.
As soon as you notice the first symptoms of fungal infection, immediately go to the hospital. A dermatologist will examine you and prescribe appropriate treatment. The sooner you contact a specialist, the easier the treatment will be.
Treating a fungal infection is not a quick process, so be patient. It can take up to a year, it all depends on how advanced the disease is. Do not delay treatment, as the fungus can spread to other parts of the body over time.
Treatment at home
Treatment of fungus between the toes at home is acceptable in the initial stages; when it comes to the later stages of development of the parasite, traditional methods are used as a concomitant treatment, but only after consultation with a doctor.
Treatment of the parasite takes a month or two, so patience will be the most important key to recovery.
Pediatric onychomycosis
Children are always special patients and fungus on the toes and its treatment in a child requires special care in procedures.
Fungus on a child’s feet develops very often, and there are many reasons for this:
- quickly growing feet, which makes shoes always tight;
- scratches;
- outdoor games;
- poorly maintained nails;
- weakened immune system;
- fungus in parents.
Oral medications are not recommended for children, therefore the remedy for fungus on the toes between the toes for a child can only be external. Most often, children are recommended:
- Terbinafine;
- Exoderil.
Both of these drugs are applicable from the age of two, the course of treatment is just as simple - it is necessary to alternate decades of use and a break until the legs are completely healed.
If the stage of the fungus is advanced and there is nowhere to go, and the drugs, according to pharmacologists, do not affect the liver, then the following are prescribed to children as drug treatment:
- Exifin;
- Mycoterbin;
- Terbizil.
But it is not worth taking it to the most advanced stage of treatment. The course of treatment will be up to 2 weeks, 1-2 tablets, it all depends on the stage.
It is strictly forbidden to resort to self-medication of a child using home methods without the recommendation of a specialist.
In pregnant women
Oral drugs
Applications (powders, tablets) cannot be used under any circumstances, only ointments and creams remain.
An ointment for fungus on the feet between the toes should be chosen after reading the contraindications; at the moment, only three ointments on the market do not have contraindications for pregnancy, these are:
- Lamisil;
- Exoderil;
- Clotrimazole.
If the price of Exoderil is too high, then use two other creams, they are inexpensive but effective.
During pregnancy, especially if you are allergic to the components of antifungal ointments, the most conducive to the use of traditional medicine are baths with salt and soda, as well as peroxide, potassium permanganate and other folk compounds, the main thing is not to use any of this “internally”.
Preventive actions
To avoid recurrence of pathology or prevent infection, dermatologists advise taking effective preventive measures . Several rules should be followed:
- Wash and change socks more often, and also disinfect shoes using special antifungal sprays.
- Wash your feet thoroughly every day in warm water and soap, paying special attention to the spaces between the toes.
- Avoid wearing tight shoes and socks made from artificial materials.
- Get pedicures regularly, using individual devices to treat the feet and nail plate.
- Do not share things or hygiene items with an infected person.
- Once a week, take preventative foot baths with a soda solution, adding iodine, salt or vinegar to the water.
- Lead an active lifestyle to maintain good circulation in the lower extremities.
- In public areas (saunas, baths, swimming pools, locker rooms) only wear slippers or flip-flops.
Antifungal drugs and folk remedies give noticeable results after just a few days of use, which indicates their high effectiveness.
However, it is important to remember that once you notice the first improvements, you cannot stop the therapeutic course. Treatment should be carried out for two weeks.
ethnoscience
Folk wisdom has given rise to a lot of health recipes, each of them, in the author’s opinion, deserves separate consideration, but it is worth focusing on several of the best options that explain how to treat foot fungus.
Salt
The simplest and most proven
method, the salt absorbed into the skin during the bath dries it out, eradicating the moist habitat necessary for the fungus to develop.
Take a bath every day, this will promote recovery, it is better to take sea salt, it softens the nails and skin and helps remove affected areas.
Iodine
Being an excellent antiseptic,
also suitable against fungus:
- you can simply smear the areas infected with the parasite;
- you can make baths.
Due to the aggressiveness of iodine as a reagent, its use has a number of restrictions:
- it causes an allergic reaction;
- in the later stages of development of the parasite, it is also not applicable, because the skin has burst, and iodine can harm the subcutaneous tissues;
- the maximum concentration of iodine in a solution used against fungus is 5%;
- the use of iodine leaves traces because when treating a fungus on the big toe, wearing open-toed shoes will not work.
Soda
One of the most effective
methods of treating fungus invented by traditional healers, the treatment procedure has many variations, requires special attention, and improper treatment leads to even greater problems with the skin.
Despite its disadvantages, soda:
- copes well with fungus between the fingers;
- can lead to long-term remission within a month of a properly maintained course of treatment.
In addition to the above methods, people popularly use:
- Kombucha for fungus;
- onion juice;
- decoctions of oak bark;
- glycerol;
- bromine and much more.
Drug treatment
Classical medicine has developed many means of combating fungus between the toes.
The most popular external preparations are creams and ointments, which include:
- terbinafine;
- miconazole;
- econazole;
- ketoconazole
Among the cheap ointments, Clotrimazole is quite effective.
Experts recommend tablets only in advanced versions, because:
- they have a strong effect on the liver;
- They generally have a large list of contraindications.
The most popular drugs in tablet form are:
- Lamisil;
- Mikosist.
Every two weeks, the course and medications need to be changed so that the parasite does not develop immunity to them.
All drug treatment has a lot of contraindications; only a specialist who has fully familiarized himself with the patient’s tests and thoroughly studied the disease has the right to prescribe a course.
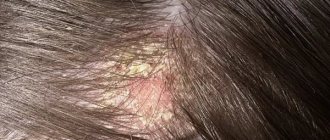
What does a skin lesion look like: description and photo
The fungus starts from the nail bed: its plate loses its transparency. The condition of the skin changes under the influence of external factors and some pathological processes in the body. Between the toes the skin is thinnest and most sensitive. The fungus destroys proteins in the dermis. It eats them, processes them and in return produces toxic products.
Scientists have found that men are more susceptible to fungal infections: they have higher levels of sweating. Among women, this problem is more common among athletes, as well as those who are too keen on pedicures, especially without proper treatment of the instruments.
In the following photo you can see what a fungal infection looks like: