Causes of shingles
Herpes zoster is a sporadic disease that occurs as a result of activation of the latent varicella zoster virus and is characterized by inflammation of the dorsal roots of the spinal cord and intervertebral ganglia, as well as symptoms of general intoxication and the appearance of vesicular exanthema along the sensory nerves involved in the process.
Shingles was known back in ancient times, but it was considered as an independent disease. For a long time, lichen together with chickenpox was often mistaken for smallpox, despite the fact that the clinical differences between these two infections back in the 60s of the 18th century. established and described by the famous English physician W. Heberden. The first suggestion about the connection between shingles and smallpox was made in 1888 by the Austro-Hungarian doctor I. von Bokay, who observed chickenpox in children after contact with patients with shingles. In 1943, the German physician and biologist G. Ruska, using electron microscopy of vesicles of chickenpox and herpes zoster, observed identical ultrastructural viral particles.
The relevance of the problem of herpes zoster at the present stage is due to an increase in the number of patients due to the aging population and an increase in the number of people with cellular immunosuppression. The incidence of the disease among people aged 60-80 years ranges from 5 to 10 cases per 1000 people, and in the general population this figure is 1.3-4.8 per 1000 people. 30% of patients with herpes zoster experience complications, and 20% have long-term symptomatic post-zoster neuralgia.
The causative agent of herpes zoster belongs to the genus Varicellovirus, subfamily Alphaherpesvirinae, family Herpesviridae. This virus is not stable outside the human body; it is quickly inactivated by disinfectants when it dries out and the temperature rises above 60 ° C, but is well preserved at low temperatures.
The cause of shingles is considered to be viral carriage, which is activated under the influence of certain unfavorable factors. The source of infection in herpes zoster and chickenpox is the patient, who becomes dangerous to others at the end of the incubation period (6-7 hours before the appearance of the rash) and up to the 5th day from the moment the last elements appear. A patient with herpes zoster produces significantly less virus than a patient with chickenpox.
The mechanism of transmission of the pathogen in chickenpox is airborne. Despite the weak stability of viruses in the environment, the possibility of their spread from the air outside the room where the patient is located, through an open door, ventilation system, etc., has been proven. Thus, the possibility of infection can spread throughout the entire house.
The weakening of virus-specific cell-mediated immunity, which occurs as a result of aging or with the development of diseases, causes immunosuppression; when using immunosuppressive drugs, it increases the risk of developing herpes zoster. Therefore, the disease mainly affects elderly and senile people. In this case, the trigger for the occurrence of herpes zoster may be contact with a patient with chickenpox, as well as:
- taking drugs that reduce immunity;
- chronic stress and exhausting work;
- oncological diseases (lymphogranulomatosis, malignant tumors);
- consequences of radiation therapy;
- patients with HIV infection in the stage of transition to AIDS;
- organ and bone marrow transplantation.
The incidence rates of herpes zoster are elevated among people with immunodeficiency conditions, primarily with HIV infection. There is an opinion that herpetic viral infection acts as a cofactor of HIV infection, since it increases the sensitivity to HIV of seronegative individuals.
In the international classification of diseases, viral infections characterized by lesions of the skin and mucous membranes include:
- herpes zoster with encephalitis,
- herpes zoster with meningitis,
- herpes zoster with other complications of the nervous system,
- herpes zoster with ocular complications,
- disseminated herpes zoster,
- herpes zoster with other complications,
- herpes zoster without complications.
Depending on the damage to a particular ganglion, gangliocutaneous, ear, ocular, gangrenous (necrotic) herpes zoster, with damage to the autonomic ganglia, are also clinically distinguished.
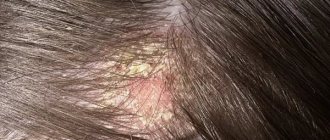
Symptoms of herpes zoster depend on the clinical form. Gangliocutaneous herpes zoster is the most common. It starts off sharp:
a few days before the appearance of the rash, patients note
- fatigue,
- headache,
- itching,
- hyperesthesia,
- paresthesia,
then a sharp burning pain develops at the site of the rash
then body temperature rises and erythema appears
- a group of papules appears,
- bubbles and bubbles grow,
- merge with each other
- rash is one-sided,
- the contents of the blisters may become cloudy due to the loss of fibrin, the ingress of pyogenic flora, and then they turn into pustules,
the process ends with the formation of crusts, after which they fall off leaving scars.
With the appearance of the rash, the pain along the nerves intensifies, sometimes becomes unbearable and can persist for months after the elements disappear.
According to the localization of the pathological process, they are distinguished:
- spinal cervical is manifested by a herpetic rash on the head and burning pain in the hand, spreading to the entire affected limb and accompanied by swelling and trophic changes;
- chest is accompanied by a rash and severe pain along the intercostal nerves, which can imitate coronary heart disease;
- lumbosacral - a rash appears on the skin of the lumbar region, buttocks and lower limbs;
Herpes zoster with encephalitis or meningitis is relatively rare, but in such cases it is characterized by a severe course and high mortality. It begins with gangliocutaneous manifestations followed by the addition of symptoms of meningoencephalitis (ataxia, hallucinations, hemiplegia, meningeal symptoms, coma). All of the above localizations may be accompanied by damage to the autonomic ganglia with the development of other complications both from the nervous system and other organs (vasomotor disorders, Horner's syndrome, urinary retention, bowel dysfunction). In severe cases of the disease, the blisters are filled with hemorrhagic contents, and then deep skin necrosis develops and scars with pigmentation form (gangrenous or necrotic herpes zoster). This is more often observed in people who have been receiving glucocorticosteroids for a long time, X-ray therapy, and who have an immunodeficiency status.
Disseminated herpes zoster is characterized by the onset of a normal lesion along the course of a certain nerve and ganglion, followed by the spread of the process (including a rash) throughout the body.
Herpes zoster occurs without a rash. One of the leading symptoms of the disease is pain. The pain is usually intense, burning, and the area of its distribution corresponds to the roots of the affected ganglion. The pain syndrome intensifies at night and due to various irritations, and is often accompanied by vegetative-vascular dystonia of the hypertensive type.
Diagnostics
For a qualified specialist, making a diagnosis is not difficult. The doctor will examine the patient's skin, ask about how long the rash has appeared and whether there are other symptoms. In cases where the picture of the disease is unclear or there is a risk of complications, laboratory tests are performed:
- Blood and urine analysis. Helps prevent damage to internal organs.
- PCR (polymerase chain reaction). Used to determine the type of viral infection.
- Serological studies. They detect the body’s reaction to the virus and help determine the cause of the disease.
- Sowing. Prescribed to determine strains of pathogenic microorganisms and their response to treatment.
How to treat shingles?
Treatment of herpes zoster is predominantly symptomatic. For herpes zoster, acyclovir, valacyclovir and famciclovir are prescribed. Early use of these drugs (no later than 72 hours from the onset of the disease) produces a full effect:
- reduces acute pain,
- reduces the duration of existence of skin rash elements,
- promotes the fading of the rash,
- prevents dissemination to other parts of the body,
- prevents the development of postherpetic neuralgia,
- generally improves the quality of life of patients.
Acyclovir is used intravenously or prescribed in tablets (for adults) up to 5 times a day. It is also recommended to lubricate the affected area with acyclovir ointment. The course of treatment is 5 days. In people over 50 years of age with a high risk of postherpetic neuralgia, glucocorticosteroids can be used for a short course in moderate doses under the cover of acyclovir.
To eliminate the pain syndrome of herpes zoster, analgesics are used (for severe pain, sometimes even narcotics), lidocaine blockades, ointments with capsaicin, gabapentin, and amitriptyline.
If a bacterial infection occurs, antibiotic therapy is indicated.
In most cases, the prognosis of the disease is favorable. When severe complications occur and in persons with severely impaired immunity, the prognosis is unfavorable.
Lifestyle recommendations
Patients with herpes zoster need to eat a balanced diet. The patient's daily diet should include proteins, at least 150 grams. It is better to get them from broths, pates, dietary white meat - rabbit, chicken, turkey. The total calorie content of the diet is 2000-2500 kcal.
You should avoid fatty meats and give preference to vegetable oils.
To reduce pain and itching, compresses are made at home. To do this, pieces of ice are placed in a sealed bag. Wrap it in several layers of thick cloth and apply it to the rash. Body lotions with essential oils and sea salt baths also help relieve the condition.
What diseases can it be associated with?
Complications of herpes zoster develop with inadequate treatment, in old age or in patients with an immunodeficient status. This:
- bleeding,
- gangrene,
- meningoencephalitis,
- cerebrovascular accidents,
- loss of vision,
- glaucoma,
- Ramsay-Hunt syndrome (a combination of auricular herpes zoster with hearing impairment, nystagmus, facial paralysis, changes in taste sensations),
- paresis, etc.
Postherpetic neuralgia, which occurs after regression of the rash in more than 50% of untreated patients, is a major complication in older age.
Symptoms
Most people experience other symptoms in addition to pain and rashes:
- Feeling numb. It occurs on the side where the rash appears.
- Fever. It is observed only in the acute period of the disease. After the bubbles break through, the temperature drops.
- Headache, sensitivity to light. Symptoms are more likely to occur if the herpes has affected the neck or face.
- Fatigue, weakness and other signs of a cold. These signs appear in people with weakened immune systems.
What medications are used to treat herpes zoster?
Antiherpetic drugs
- Acyclovir - 0.015-0.03 g/kg is divided into 3 single doses and administered in 150 ml of isotonic sodium chloride solution;
- Valaciclovir - 1000 mg every 12 hours with a creatinine Cl of 30-49 ml/min or once a day with a creatinine Cl of 10-29 ml/min and 500 mg once a day with a creatinine Cl of less than 10 ml/min;
- Famciclovir - 500 mg every 8 hours for 7 days
Painkillers - used as needed
- Amitriptyline,
- Gabapentin,
- Capsaicin ointment,
- Lidocaine.
Features and types of herpes
Among the variety of herpes viruses, there are 8 main types:
- Type 1 – the simplest and most well-known to everyone. It is characterized by a rash on the lips, cheeks, and nasal mucosa and appears in the form of blisters with liquid. Accompanied by itching, swelling, malaise, muscle pain, headache, and sometimes fever.
- 2 types – “genital”. The symptoms are the same as those of herpes simplex, with localization on the genitals and buttocks. Women get sick more often. They experience exacerbation mainly at the beginning of the menstrual cycle.
- Type 3 – Varicella Zoster virus – chicken pox. Herpes type 3 often causes shingles. Having been ill once, a strong immunity is developed.
- Type 4 – Epstein-Barr virus causes mononucleosis. Infection by contact, sexual and airborne routes. It affects the nasopharynx, lymph nodes, kidneys, and spleen. Young people under the age of 25 often suffer from this disease.
- Type 5 – cytomegalovirus. “Target organs” – liver, kidneys, eyes. It is dangerous when pregnant women are infected, causing death or pathology of the fetus.
- Type 6 - there are two types: 6a (causes multiple sclerosis), 6b (pseudo-rubella in children, which most often affects children under 2 years of age). It appears as pink rashes and high fever.
- Type 7 – affects monocytes and t-lymphocytes (promotes cancer of lymph nodes). May cause chronic fatigue and negative effects on the brain. Characterized by sleep disturbances, depression, decreased memory and attention.
- Type 8 - affecting blood cells, can cause Kaposi's sarcoma and other cancers.
Treatment of herpes zoster with traditional methods
Treatment of herpes zoster is a painstaking process, which often involves folk remedies. The use of these does not eliminate the need to use antiherpetic pharmaceutical drugs, but may have an analgesic or healing effect. It would be a good idea to discuss following the advice of traditional medicine with your doctor; you can take note of the following recipes:
- 1 tsp dried wormwood herb, pour 100 ml of ethyl alcohol, leave for a week in a dark, cool place, shaking occasionally; use as a compress for 20 minutes, then lubricate the skin with castor oil;
- combine dried wormwood and tansy herbs in equal proportions, 2 tbsp. Brew the resulting mixture with a glass of boiling water, keep in a water bath for 15 minutes, and when it cools down, strain; take ½ glass orally before meals three times a day;
- burdock infusion weakens the effect of the virus - herpes zoster goes away faster and is easier;
- 2 tbsp. Brew the resulting peppermint with a glass of boiling water, keep in a water bath for 15 minutes, and after another 45 minutes, strain; use the resulting decoction to rinse the affected areas or add to the bath (for a standard bath you need 3 liters of mint decoction brewed with 200 grams of mint);
- crushed dried burdock leaves, 1 tbsp. pour 100 ml of water, place on low heat and boil for 3 minutes from the moment of boiling, cool, strain; use as a compress every night;
- Grind fresh cinquefoil leaves to a paste and use as a compress every night.
Complications
A common complication of lichen is postherpetic neuropathy. This is a condition in which the patient experiences pain after the blisters have disappeared. This complication is caused by damage to the nerve at the site of the rash.
A person may experience depression, anxiety, and insomnia for some time after treatment.
Other consequences of the disease include:
- Poorly healing wounds. Appear when a bacterial infection occurs.
- Decreased visual acuity. Occurs if the rash is around the eyes.
- Loss of hearing and taste, facial paralysis, dizziness. Complications arise in atypical forms of the disease when the cranial nerve is affected.
- Pneumonia, hepatitis or other infections. They develop if internal organs are affected.
Treatment of herpes zoster during pregnancy
The mild course of herpes zoster does not require specific measures during pregnancy. In severe cases of herpes zoster, acyclovir is used, but in the second and third trimesters and only in very severe cases - already in the first trimester.
The introduction of specific WZ-immunoglobulin during pregnancy is carried out both for the purpose of passive immunization, and for the purpose of preventing such severe complications of chickenpox and, less commonly, herpes zoster.
Vaccination is prohibited in pregnant women, but accidental administration of the vaccine to a pregnant woman is not an indication for termination of pregnancy.
How long do manifestations last?
The incubation period can last several years. Even if a person is a carrier of herpes, shingles does not always develop. The main symptoms of the disease begin to subside within 6-8 days. In place of the blisters, yellow or brown crusts form, which eventually fall off and leave a pink or white area of the skin.
Article on the topic: Anxiety-depressive disorder
The course of uncomplicated herpes zoster lasts 3-4 weeks. Severe forms are treated for several months.
Treatment of other diseases starting with the letter - o
| Treatment of obstructive bronchitis |
| Obesity treatment |
| Treatment of burns of the larynx |
| Treatment of adrenal tumors |
| Treatment of tracheal tumors |
| Treatment of ARVI |
| Treatment of orchitis |
| Treatment of osteoarthritis |
| Treatment of osteomyelitis |
| Treatment of osteoma |
| Treatment of osteoporosis |
| Treatment of osteochondrosis |
| Treatment of osteochondropathy |
| Treatment of acute abdomen |
| Treatment of acute intestinal failure |
| Treatment of acute mesenteric ischemia |
| Treatment of acute renal failure |
| Treatment of laryngeal edema |
| Treatment of otitis media |
| Treatment of pityriasis versicolor |
The information is for educational purposes only. Do not self-medicate; For all questions regarding the definition of the disease and methods of its treatment, consult your doctor. EUROLAB is not responsible for the consequences caused by the use of information posted on the portal.