- When strange acne sores appeared
- Strange acne sores on the body and face: causes of appearance
- Symptoms of strange acne diseases
- Strange pimples on hands
- Strange pimples on legs
- Strange pimples on neck
- Strange pimple sores with a stick
When strange acne sores appeared
Strange pimple sores with or without a stick can appear on the skin when the pores become clogged with the maximum possible amount of oils and impurities and then become infected with a certain set of bacteria. Acne sores, otherwise called acne pustules, are often filled with pus, painful to the touch and have bright or early stages of the appearance of a weakly defined core on the pimple sore.
Despite the fact that there are many creams and remedies against such severe inflammations, the effect of their use is often more negative due to the use of strong chemical ingredients in their composition, which can greatly irritate already immuno-weakened skin. However, acne sores can be effectively treated using certain natural alternatives that can clear the skin without causing damage for especially painful acne.
Hard pimples: Treatment, prevention and causes of the disease
Most types of pimples form when dead skin cells, oil, or bacteria block the pores. Hard pimples, such as nodules or cysts, are often deeper and more inflamed.
In this article, we will talk about how to treat and prevent the formation of hard pimples. We also look at the different types of acne and their causes.
Reasons for appearance
Pimples appear due to the production of excessive amounts of sebum by the glands.
It clogs the excretory ducts of the pores and inflammation begins.
The reasons that stimulate increased work of the glands can be different:
- heredity;
- allergy;
- hormonal imbalances;
- unbalanced diet;
- diseases of internal organs;
- experiences, stress;
- poor skin care;
- incorrectly selected cosmetics.
What are there
Whether you can squeeze a pimple depends on its type:
- The subcutaneous one does not have a purulent head, and its contents are deep. It looks and feels like a small ball. The internal pimple may become inflamed, as evidenced by its redness.
- Purulent is determined by the presence of a white head. A ripe purulent pimple is ready for removal, but an immature pimple should never be crushed. It’s better to wait until it ripens on its own, or you can speed up this process.
Medicine against furunculosis
As mentioned above, internal acne can not only be a consequence of poor (or non-compliance with) personal hygiene, it may well be a symptom of more serious disorders in the body. Therefore, it is extremely important to understand the reason for their occurrence in your particular case.
Only a specialist after an examination can draw clear conclusions on this matter.
But if no serious violations are detected, doctors recommend using ointments (usually Vishnevsky or Ichthyol ointment). They cause rapid maturation of the boil and relieve inflammation.
How to tell if a pimple is ripe
Before getting rid of a pimple, it is important to understand that it has already matured.
- Squeezing out pus located deep under the skin will not produce results.
- In addition, this will lead to severe damage to the integument and even greater inflammation, which does not go away for a long time.
- After violent manipulation, scars and noticeable scars may remain.
There are two sure signs, the combination of which will help identify a ripe pimple:
white head formation
- Presence of a white head. This indicates that the pus and sebum that clogged the lumen have entered the surface layer of the skin towards the exit.
- No inflammation or redness around the formation.
If a white head appears, but the redness does not subside, then you should not touch such a pimple. You need to wait until it finally ripens.
What does our skin say?
Scientists have long proven that the skin is an external signaling device. It can tell a lot about a person’s state of health. And if we talk about the occurrence of acne on the skin, then you can also use them to navigate the direction of the disease and identify the problematic organ.
Frontal part
The appearance of acne in this area indicates intestinal problems. This can be caused by stress, weakening of the body, and depression. If these symptoms are ignored, colitis or dysbacteriosis may develop.
Eye area
The eyes and the area around them are closely related to the functioning of the kidneys. Therefore, if problems are found in this area, a consultation with a urologist is necessary. In addition to acne, swelling may form. This is also a signal that the normal functioning of the kidneys is disrupted; they cannot cope with the removal of fluid.
Inner eyelid
Signal of an eye problem. Be sure to consult an ophthalmologist (ophthalmologist). It is quite difficult to answer unequivocally what exactly the problem was, due to the fact that there are several of them. Don't risk your eyesight in vain.
Cheeks
Acne in this area indicates a disruption in the functioning of the kidneys, liver and gastrointestinal tract. These three organs are closely related to each other and are responsible for cleansing the body.
As a result of failures of them (or one of them), the removal of toxins from the body slows down, resulting in their accumulation in the area of the sebaceous glands and, as a consequence, the occurrence of inflammatory processes.
Such disorders can also be caused by poor nutrition, excessive consumption of salty, fatty foods and all kinds of canned foods.
Oral cavity
It's time to see a dentist. Such pimples signal the onset of diseases such as candidiasis or stomatitis. In turn, their appearance can provoke a weakening of the immune system.
Strange acne sores on the body and face: causes of appearance
Poll: When did your acne appear? (Number of votes: 4295)
I've been suffering all my life
It's been a couple of years now
About a few months
Recently
To vote, click on the desired answer. results
No qualified dermatologist can tell you the 100% exact reason for the appearance of strange acne sores, but hormones called androgens play a certain important role in the cause of their appearance on both the face and body. When you are a teenager, androgens increase at a colossal rate that causes changes in your skin that can lead to clogged pores and acne. In women, hormone changes can be caused by menstrual cycles, pregnancy, menopause, or a condition called polycystic ovary syndrome.
If one of your parents had severe cystic acne, the symptoms of which are pronounced white streaks, you are 70% genetically more likely to get it again as a teenager or even an adult.
Strange acne sores can especially develop when hair follicles become infected with bacteria or fungus and become blocked by a plug of oil, dead skin cells and potentially other debris, leading to inflammation and bacterial overgrowth in cystic acne.
All severe forms of acne that are accompanied by sores are inflammatory, and when inflammation appears around the sebaceous glands, it causes the area of inflammation on the face or body to swell and the skin to produce more sebum, which ultimately leads to what usually leads to serious complications and the increasing spread of pus-filled acne sores. For both different and similar reasons, this type of acne can appear both in the face and body, including the arms, legs and quite often also the neck and central areas of the face.
Symptoms
When a patient complains of strange pimples, this does not mean that they are actually special. It’s just that a person has never encountered such rashes before and considers them something incomprehensible. This may apply to acne with the following characteristics:
- Which are not squeezed out, but remain under the skin.
- With serous contents (clear liquid).
- Accompanied by the formation of erosions and ulcers (“wounds” or “sores”).
- They are localized not only on the face, but also on other parts of the body.
- They cannot be cured on their own.
If something in the development of acne goes beyond what a particular patient would expect, he may call it strange. But to the doctor, the rash will not appear as such, since he knows the probable variants.
Acne
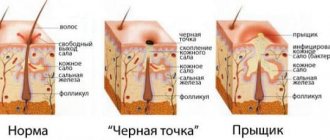
When sebum production is disrupted and follicular canals become keratinized, acne (blackheads) develops. They may be of the following nature:
- Open or closed comedones.
- Papules (small nodules).
- Pustules (with a purulent core).
- Dense subcutaneous nodes.
First, when there is only a blockage of the excretory ducts of the sebaceous glands, comedones are formed. They are called open when the plug is located near the surface and is easily removed. Closed comedones often take on the appearance of blackheads, and when squeezed out of the pore, the thick sebum clogged there (pimple core) comes out.
The addition of an infection leads to the development of inflammation - then comedones turn into all other elements (papules, pustules, nodes). Often acne can merge with each other, forming dense conglomerates with a bumpy surface. Microabscesses sometimes form in the center of some acne, which heal with scarring once opened.
Acne is a fairly common phenomenon that many young people experience.
Milia
If the pimple is difficult to squeeze out and looks like a small millet-like white nodule, then most likely it is milia. Many such rashes are called millet. In most cases, the elements are located around the eyes and on the cheeks. Milia are accumulations of keratin in the surface layer of the skin, that is, they are peculiar small cysts.
It is very difficult to squeeze out these pimples, but if you succeed, what comes out is not a thick mass in the form of a rod, but a small amount of white soft substance. In addition, rashes disappear on their own during the process of natural skin renewal, which once again distinguishes them from comedones.
Pyoderma
Pyoderma involves an inflammatory process with the formation of pus. If it is of staphylococcal origin, it is characterized by damage to the hair follicle, ducts of the sebaceous and sweat glands. In this case, the element (pustule) has a conical shape with infiltration at the base. When opened, thick yellow-green pus comes out, and in the center there is vellus hair.
Streptococcal pyoderma is accompanied mainly by superficial skin lesions. Flat blisters with a flabby tire (phlyctena) are formed, and their contents are serous-purulent in nature. Such elements are prone to peripheral growth and fusion.
Herpes simplex
Another example of acne that does not fit into the patient’s usual understanding is herpetic eruptions. And although they occur in many people (the rate of infection of the population with the virus is almost 95%), not everyone understands how herpes simplex manifests itself.
First, at the site of future elements - mainly on the lip or nose - itching and burning appear. Soon bubbles appear there, filled with serous contents resembling water. The vesicles burst and transform into superficial erosions, which become crusted.
With herpes simplex, the vesicle turns into erosion, which becomes covered with a crust and heals without a trace.
Allergic diathesis
Strange pimples of an allergic nature also occur. In children they have the form of diathesis, and in adults we are talking about neurodermatitis and atopic dermatitis. Elements on the skin of the face are distinguished by polymorphism: spots, papules, vesicles. In children, typical lesions are located on the cheeks and are accompanied by weeping and peeling. At this time, fatty yellowish scales (gneiss) form on the scalp.
In adults, the body's sensitization to the allergen is more pronounced. Characterized by redness, swelling of the skin, papules and vesicles. All this is accompanied by severe itching, which causes scratching and may result in a secondary infection (pyoderma). In neurodermatitis, the lesions are located predominantly on the flexor surfaces and are accompanied by increased skin pattern and peeling.
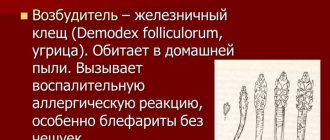
Demodicosis
If a Demodex mite has settled in the skin, strange rashes may appear on the face. Conventional anti-acne medications do not have an effect; instead, acne spreads more strongly and sebum secretion increases. If red dots and papules appear first, then later they turn into pustules. Often the eyelids are affected, where inflammation occurs (blepharitis) and eyelashes fall out.
Symptoms of strange acne diseases
The easiest way to differentiate between a regular pimple and a pimple that seems strange is to pay attention to the warning signs. For example, if you feel a tingling or burning sensation before the spot appears, this is one of your body's ways of telling you that a new phase of the development of a cold pimple sore is beginning. "Often you may feel tingling, itching or burning in completely different areas of the skin of the body or face until blisters with a pronounced core or cyst appear,” explains Sejal Shah, a dermatologist from New York and founder of Smart Skin Dermatology. In dermatological circles, this phase of acne development is more is known as the prodromal phase of the herpes simplex virus, when people experience changes in themselves (such as said inflammation) but have not yet acquired the clear symptoms of developing cystic acne.
Strange pimples on hands
As a rule, strange pimples on the hands are symptoms of certain internal or external skin diseases. In the case of internal ones, these may be allergic reactions to certain foods or drugs. In the case of external ones, this may be a skin reaction to some chemical or cosmetic products. Red pimple sores can be caused by infectious or chronic skin diseases, the main influence of which is exerted by intradermal parasites and “mites”.
Strange pimples on neck
Quite often, the main reason for the appearance of strange pimples on the back of the neck is a disruption in the functioning of the endocrine and digestive systems. To make a more accurate diagnosis, you will have to contact both an endocrinologist and a dermatologist. It is also not uncommon for the spread of strange acne sores on the neck to be a consequence of the introduction of infectious skin viruses or in the case of purulent cores of pathogenic microorganisms, which more often happens with a sharp weakening and decline of immunity.
Strange pimples with a stick
Strange pimple sores with a stick
How is this treated?
The creams and ointments we use to treat common acne often have little effect on stubborn acne. When diagnosed with severe acne like this, your dermatologist will likely recommend one or more of the following:
Oral antibiotics that help control the growth of bacteria and relieve the inflammation of the pimple sore in no time. Sometimes your acne may not respond to antibiotics. Or you may find that they stop working over time as addiction occurs over time.
Formulated creams, lotions, or gels with retinoid, a form of vitamin A, can help keep your pores from becoming clogged with oil and bacteria and help the antibiotics do their job.
Isotretinoin (formally known as Accutane, but now available as Claravis, Sotret, Myorisan, Amnesteem and Absorica) is quite effective in treating all types of acne, as well as other forms of severe acne. The recommended dosage for most of these drugs is to take 1 tablet alone or twice a day for about 5 months. For most patients with similar problems, this course of treatment clears the skin completely.
Spironolactone is a medicine that helps effectively get rid of cystic acne, especially in women.
Skin garbage is incomprehensible | Beauty | Medicine and health
- Has anyone had a similar experience and found a way to treat it? This takes a very long time. And it’s not a rash, but isolated painful sores. It’s as if there is a hole in the skin down to the “meat”, and the hole is filled with loose “rubbery” foreign tissue. When you pick it off, it feels like bubbles are bursting under your nail, like in the pulp of a watermelon. Or they may not burst, but, for example, feel like compressed bread crumb. And no matter what she does with it mechanically - she picks it out, for example - it’s as if there are roots in the skin, such a substance grows again and is covered on top with normal-looking skin, but inside this painful thing still lives on. When bathing in warm water, this substance loosens, becomes soaked, enlarges and is easily removed, leaving behind again a hole in the skin, bleeding and lined with white mucus, from which apparently the same foreign tissue then grows again. No ointments simply help. At school I had one of these on my head in my hair for about a year or two, then after school one of these appeared on my lower back near my spine - it probably lasted for about 10 years, after giving birth they began to appear one after another on my back along the spine, behind my ears, in my ears, on my neck. .. Over the past 4 years, I have been to 6 dermatologists (including in Artmed, KKB), all of them, with a slight glance, prescribed treatment for acne, they did not listen to my descriptions and did not prescribe any tests. What could be wrong with me? And let me add: I also get acne, I know what they are, and I can confidently say that these “sores” have nothing to do with acne. At sea in the sun, within two weeks, acne and pimples disappeared, and these “sores” only underwent constant renewal of contents - the contents were distributed in the salty sea, again there remained a bleeding hole with a white bottom, which again began
- Can you tell me where to go to get examined or something? Tired of wasting money on external examinations and prescriptions of anti-acne ointments, which are powerless in my case? The only time they stepped back from the external examination and took a scraping from my elbow to check for scabies mites, so I myself knew that there were none. I'm exhausted. I’m already 42 years old, and I’ve had sores on my face and neck all my life ((
- According to the description, everything looks exactly like mine, it doesn’t look like a mollusk, the curdled core is missing, I haven’t observed anything like that, but it’s like rubber, it looks like something, I assumed that it was something viral, maybe warts.. and began to smear it oxolinic ointment and laundry soap, only to 72%, and they begin to disappear, try, as soon as they appear, you need to smear them right away, I still have itching in the wound.
- I’ll say a seditious thing - try it on one, when it’s cleared of contents, spray it with belosalik according to the instructions
- By the way, about the scraping, the laboratory will take it from where you say, and not from a clean elbow.
- I also thought about it, as a child I had a lot of it in my arms, my mother somehow took it out. The holes remained on the hands, small ones.
- Can you tell me where to go? Directly to the laboratory? We need versions in advance of what exactly to look for? Thank you.
- I'll try and buy it tomorrow. Aren't new ones coming out? Otherwise, the problem is that new ones are still creeping out. Has everything worked out for you?
- I searched and dug into skin diseases, tried my own treatment for this mollusk, but it didn’t help. Or maybe I didn’t complete my treatment, maybe it took longer. Below they suggested about the laboratory, probably it will be necessary to be tested more specifically for mollusk.
- at least in vitro, at least hemotest, at least SMD...
- But I can’t tell you to find out what it is? Should I give them diagnoses that need to be checked? So far I have dug up molluscum contagiosum, herpes of some kind (although herpes, judging by the pictures, are solid large blisters, and in these swellings I have fleshy, flesh-colored flesh, which, when crushed, strains to burst like a watermelon pulp into small bubbles). Maybe they themselves will offer something else?
- Thanks for the advice anyway. I'll try to find out on my own in the laboratory.
- you need to see an ongolug surgeon) let them cut it out. First they’ll take a scraping
- my child had this diagnosis, I think dermatologists would have seen during a visual examination that the diagnosis was made. And this is where it differs from your story - the mollusk, after its contents (about the same as in your story, it is white) leaves “its little house”, the wound heals, and new ones may appear somewhere nearby, but not exactly in it. I am not a doctor.
- Maybe the contents are not completely extracted, so it still grows?
- Author, I had this happen. Transparent serous wells, how? This is pure psychosomatics... Google “serous well” - most likely, this is it.
- That is, you diagnosed the author with eczema?
- I read it and looked at the photo. There are some coincidences in the description, but overall it doesn’t seem like it. Especially the wells themselves - I don’t see them. that is, it’s like holes through which liquid oozes? there is no such thing. Thanks for the version. I don’t know if it can be tested in a laboratory. When suitable material “grows”, I will contact the laboratory directly and do tests for several versions. Now there is nothing to take from - I picked it out and cauterized it.
- I'm reporting. I tried oxolinic ointment as recommended above. But it only got worse. the sores softened, swelled, and conquered new territories around the edges - that is, they increased in area. There was no healing. It was as if the porridge was being cooked. I also read about types of struggle, for example, with molluscum contagiosum. I’m not sure that I have it, because judging by the descriptions, a molluscum body is clearly visible there, and I have a kind of diffusion of abnormal painful “rubber” tissue with normal skin tissue. So I came across in the descriptions cauterization with hydrogen peroxide. Peroxide was found in the first aid kit. Total: out of 8 active volcanoes, five of them were healed to normal skin, there was no pain when pressing (usually, if it was tightened, then from the pain I felt that something was continuing to ripen there and would soon grow again). the remaining three are covered with a crust, the pain is moderate, quite natural for an unhealed sore and less than what it was when it was brewing inside the “volcano”. I hope that they will end soon. She also cauterized any suspicious pimples that appeared; once they had crusted over, they stopped hurting and seemed to be finishing their development. I doubt that such details are of interest to people who do not have similar problems. But if someone also has similar problems, maybe hydrogen peroxide can also help. I’m not sure that my problems will end there, I think new outbreaks will still appear. I’ll try to fight it at the very beginning with the same peroxide. I haven’t gone to the laboratory yet, as advised above. Because we still need to “grow” the material for analysis, but now everything is “burnt.” If it continues in the future, I’ll do tests. Thanks to everyone who didn’t pass by.
- Just in case. Molluscum contagiosum is treated primitively. The blister is opened with sharp scissors, the contents are squeezed out and the wound is cauterized with iodine. All. This is exactly how the nephew was treated. No relapses.
- Then I’m definitely not contagious. the contents are not squeezed out that easily. there is no separable content as such. There is an incomprehensible painful tissue grown into ordinary skin.
- What rubbish! good luck with your treatment.
- Thanks a lot. I burn napalm with peroxide, this rubbish noticeably recedes. There is hope.
- Good luck and health! Let everything pass and be forgotten
- Thank you very much. Now more than ever there is great hope for this.
- Try tetracycline ointment. It heals the skin very well and has an antibacterial effect.
- I'm afraid that it will act like oxolinic acid. Now the hearth is drying very well and narrowing. I'll continue like this. but thanks for the advice anyway.
- these are two different ointments and do not act the same) you try it in one place, the ointment is inexpensive but it helped me a lot. Good luck
- okay I will try. Thank you.
Source: https://eva.ru/beauty/messages-3289150.htm