Black spots on the legs can be a sign of several dermatological problems. These are the consequences of ingrown hair, if they are found on the shin and plantar warts, if there are black spots on the heels.
Black spots on the legs - a signal to get checked by a specialist
Causes of warts
Skin neoplasms in the form of plantar warts are a common disease that is considered benign. It affects 10% of the world's population.
All warts, without exception, have the same nature - they are caused by the human papillomavirus (HPV). The virus spreads exclusively through contact. Most often, people become infected in swimming pools, bathhouses, and gyms, since a humid and warm environment is ideal for the virus to develop through household items. Infection can occur through contact with a sick person and when walking barefoot.
It is the person who is the carrier of the infection. The virus can exist without a host for several months and thus remains infectious for a long time. It exhibits resistance to both high and low temperatures.
The plantar form of warts, which accounts for 1/3 of all cases, is caused by HPV type 1. People in the age group from 20 to 45 years are more susceptible to it. Children rarely get sick.
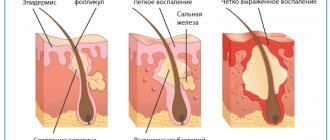
If a person’s immune system is strong, then it provides adequate resistance and the virus remains in a latent state, not manifesting itself in any way. This period can be 6 months or more. The virus is located in the deep layers of the dermis and actively multiplies in the place where it has penetrated. This area is deformed, but so far the process is not visible in any way. But when, due to various reasons, the immune system weakens, the virus enters an active state, begins to spread both horizontally and vertically and manifests itself in the form of neoplasms with roots extending deep into the dermis. In the affected area, rapid keratinization of cells occurs, and neighboring areas are compressed. Therefore, the papule has clear boundaries and does not damage neighboring areas. But due to the fact that nearby areas are compressed, a feeling of pain occurs.
There are many factors that can cause blackheads to appear.
Provoking factors for the development of warts are:
- loosening of the epidermis due to increased sweating of the feet;
- dry skin on the feet;
- uncomfortable shoes that squeeze your feet;
- diseases such as flat feet, arthritis, osteoarthritis;
- systemic diseases leading to disruption of the nutritional processes of skin cells and tissues (diabetes mellitus, varicose veins, etc.);
- immunodeficiency conditions caused by chemotherapy, HIV infection, long-term use of cytostatics, which is accompanied by the fact that the skin loses its ability to act as a barrier to the virus;
- mechanical and chemical damage to the skin (abrasions, cuts, inflamed areas around an ingrown nail, broken callus, etc.).
Already existing tumors can infect neighboring areas of the skin and thereby form entire clusters on the feet.
How to treat ingrown calluses?
The main thing you should know is no self-medication! Such formations are strictly not allowed to be cauterized, cut out, steamed, or treated with caustic compounds or “magic” ointments. All methods not recommended by the doctor often lead to skin damage, which will lead to the dynamic growth of deep calluses. First a dermatologist, then treatment. Only a doctor can determine the dynamics of the course and development of the pathology, the depth of germination of the rod. Depending on these factors, treatment will be determined and medicinal, surgical or traditional methods of treatment will be prescribed.
Important! A viral fungal infection, which is typical in the presence of a black callus with a dot, can quickly spread to healthy areas of the skin if self-medicated. Curing the disease will become much more difficult.
Signs of illness
When a hard, cavity-free element is found on the plantar surface of the feet, rising 1-2 mm above the skin, this is a sign of a plantar wart. Other forms of tumors protrude significantly above the surface. This intradermal location is due to the fact that the foot is constantly under pressure when walking and standing. Under such conditions, the compaction simply does not have the opportunity to grow.
Most often, one wart appears
The shape of the growth is round. The size can range from a few millimeters to 2 cm. The color of the skin in the affected area often does not change, but may become pink or light brown.
More often, single papules appear, but if there are too many compactions, they merge into plaques, which are called “mosaic warts.” And this suggests that the virus is highly active.
The tendency to “reproduce” is also explained by the ability of the virus to spread horizontally and penetrate other areas when the integrity of the cover is violated or other warts are improperly removed. The maternal tumor is larger in size than the scattering of newly appeared compactions.
A newly formed papule has a smooth surface, which gradually becomes rougher. Over time, the surface becomes rough to the touch and changes color to yellow-gray, which makes the formation look like a dry callus. The top layer can be either smooth or have a depression in the center, similar to a volcanic crater.
This lesion hurts when walking. When you remove the surface layer, open it, or simply look closely, you can see black or dark brown dots. They arise as a result of injury to capillaries that bleed, resulting in the formation of compactions of dried blood - blood clots. This punctate mosaic is a hallmark of plantar tumors.
Another characteristic feature that distinguishes warts from calluses is subjective sensations. The callus hurts with direct pressure, such as when walking. If a wart occurs, it hurts when the skin area shrinks, i.e. without direct pressure. Obvious discomfort is felt when wearing shoes. That’s why it is so often compared to a heel spike and called a “spike.” When a rough papule is injured, bleeding begins, which can easily be stopped by squeezing the tissue or treating it with an antiseptic.
Warts can be found anywhere on the sole, but most often appear in the supporting areas where the most pressure occurs on the foot: the heel, balls of the feet and toes.
In 30% of cases, the compaction resolves on its own and leaves no trace on the skin. In this case, the virus is gradually removed along with dead cells during the process of natural skin renewal.
But in most cases, treatment is required, since constant friction and pressure cause serious discomfort and pain and prevent the papule from going away voluntarily. In addition, if the virus remains in the deep layers of the dermis, relapses of the disease are possible. Even if the wart has disappeared without a trace on its own, this does not mean that such tumors will not appear again, since the body is not able to develop immunity to HPV.
Medicines and drug therapy
A callus on the toe or sole can be treated with pharmaceutical preparations based on salicylic acid. The preparations are applied only to the affected area; it is prohibited to apply the preparations to healthy skin. The following medicinal formulations are best suited:
- Super Anticallos is a drug for removing growths, containing the active ingredients urea and lactic acid.
- Balm Karavaeva (Vitaon) with herbal extracts. The product is very effective and can be used to treat deep root germinations.
- Nemozol is a cream containing concentrated salicylic acid and has already proven effectiveness.
- Sto-corn is a liquid substance packaged in a bottle with a dispenser. Ease of use is a big plus, but the therapy will be long, but regular use provides very good results.
Advice! If the dermatologist determines the presence of a fungus or viral infection, antifungal drugs such as Acyclovir, Penciclovir, Lamisil will be prescribed.
The Salipod plaster is a good way to combat calluses. An effective remedy rarely fails to treat growths caused by a fungal or viral infection. Application of the patch is incredibly simple:
- Apply a patch to a dry and clean lesion;
- Secure Salipod with a regular plaster;
- Do not remove the bandage for 3-4 days, then remove the bandage;
- Steam the foot and remove the rod.
If the rod part has gone deep enough, you should repeat the procedure again with wearing a bandage for 3 days. After removing the rod, a deep wound remains, which must be lubricated with an antiseptic and protected from dirt. In addition to this type of patch, pharmacies offer quite a few other identical products and their use is the only cases when piercing the growth is allowed, and then only after preliminary steaming in hot water.
Advice! Orthotics should be worn during medication treatment to relieve pressure on the foot or heel.
Medicines are not the only option; in some cases, doctors prescribe more modern methods for removing ingrown calluses:
- Laser removal is effective in very advanced cases. The laser beam burns the core base and removes all pathogenic bacteria, minimizing the risk of inflammation after the procedure.
- Hardware drilling (removal) is the process of removing a deeply embedded rod. After the procedure with a special device, the doctor puts an antibacterial agent into the wound to prevent relapses and infection of the affected area.
- Cryodestruction with liquid nitrogen is a proven method of burning out a seal with a central rod. The efficiency and painlessness of the operation, as well as the absence of the risk of secondary germination, are the advantages of the procedure.
- The radio wave ablation method is a painless operation in which radio waves evaporate water from abnormal cells, destroying the formation. Pros: no impact on adjacent healthy tissue.
- Electrocoagulation – removal of growths by exposure to alternating current. A protective crust remains at the site of burning, which acts as a biological bandage. After 10-12 days, the crust disappears on its own, leaving clean skin.
All treatment methods are prescribed only after examination by a dermatologist. It is strictly forbidden to use medications for self-medication due to the possibility of developing a fungal infection in the callus. Even a safe patch can lead to the proliferation of bacteria and the rapid development of the disease. In this case, the lesion will increase in area and depth, but it will be much more difficult to cure it.
Diagnostic measures
Only a dermatologist can accurately determine that a lump on the leg is caused by HPV. Externally, the formation is very similar to a callus, but does not have a skin pattern on the surface. The doctor will scrape the upper layer of the epidermis and a black dot found on the leg will serve as a sign of a plantar wart.
It is important to consult a doctor immediately to determine the cause of the disease
In most cases, a visual examination by a specialist is sufficient to make a diagnosis. But to confirm the presence of HPV, a polymerase chain reaction or PCR is prescribed. Today this is the most accurate way to identify the pathogen. The method is based on the detection of viral DNA fragments.
It is possible to prescribe an ultrasound to determine the depth of the root of a skin tumor.
Differentiated diagnostics are carried out to exclude dermatoses characterized by disruption of the process of keratinization, mainly of the palmar and plantar surfaces and cutaneous manifestations of syphilis.
If dark spots on the heel and foot hurt when walking
If rounded black attributes are found on the legs, go to the hospital; the elements may indicate the presence of pathological HPV formations:
- core calluses;
- plantar warts.
A black spot on the foot or heel is eliminated using complex treatment, which includes therapy to increase the body’s immune defense, removal of plantar formation using cryodestruction, laser beam, and medicinal burning with drugs.
Therapeutic measures
Despite the low level of transition of education into an oncological form, it is not recommended to fight it on your own and use traditional medicine.
Plantar wart, unlike other varieties, has long roots that are located deep in the skin. This makes its removal significantly more difficult.
Nevertheless, modern dermatology knows a large list of treatment methods:
- electrocoagulation;
- cryodestruction;
- laser technique;
- radio wave method;
- surgical intervention.
There are several ways to remove a wart on the leg
Electrocoagulation is a method of applying electric current to a growth. Under the influence of high temperatures, the wart falls off, and the blood vessels are sealed and do not bleed. The procedure is performed under local anesthesia. The most effective use of current is for papules that lie in the superficial layers of the epidermis. If you use this method more deeply, there is a risk of scarring.
Cryodestruction is a method of exposure to liquid nitrogen, the temperature of which is almost minus 200 degrees. Nitrogen freezes viral agents. But this method shows the greatest effectiveness if the growth is young (up to six months). If the seals are old, then only in 30% of cases will nitrogen help remove them.
This method is quite sensitive to the skin. May leave redness and swelling. After the procedure, a bubble filled with liquid forms at the site of nitrogen exposure, which then dries to form a crust.
Liquid nitrogen eliminates the formation of scars after removal, does not require anesthesia, and the duration of manipulation is no more than 2 minutes. On the other hand, the method of superficial exposure does not guarantee that relapses will not recur. Cryodestruction provides for a rehabilitation period: treatment with an antiseptic 2 times a day, protection from external factors during the healing period.
The most common way to get rid of blackheads is using a laser. The beam removes keratinized cells layer by layer, thereby ensuring control over the depth of exposure. At the same time, the vessels are sealed and bleeding is prevented. There are several types of techniques, but the most effective is the pulsed dye beam. It is effective in 95% of cases.
The method not only eliminates growths, but also stimulates local immunity. The laser beam leaves small dried crusts after exposure, which fall off the skin on their own without requiring additional care. The laser is safe for neighboring tissues and the likelihood of relapses from its effects is reduced to zero.
The only downside may be the cost of the procedure.
If there are large areas covered with warts, surgical excision of the plaques is resorted to. It is performed using a scalpel under local anesthesia.
Treatment
In 90% of people, a wart on the foot or palm goes away without treatment at an early stage, and in 30% of cases - in the first 3 months. The immune system suppresses the virus and heals the skin. The time of self-healing depends on the stage of the process: from 2 weeks to 1.5 years.
When should a spine be treated?
When the body itself cannot cope with the disease and needs help:
- if it hurts a lot,
- if it interferes with walking,
- if it has grown to a large size,
- if subsidiaries appear nearby.
How and with what to treat?
Removal is a treatment method that is successful in 98% of patients.
1) Removal with drugs
For these purposes, locally necrotizing agents are used.
- Solcoderm (detailed article about this drug - link),
- Vartox (read in more detail - link),
- duofilm (instructions),
- Collomak (instructions),
- super clean,
- verrukacid, or feresol (read instructions) - acts more gently, efficiency is good,
- lapis (read about lapis pencil) - effective with long-term use.
Most of these products contain acids or alkalis. Removal of plantar warts (spikes) occurs through a chemical burn of the skin. The wart dies. And in this place there remains an inconspicuous scar.
Treatment time in most cases for drugs is: 1 - 5 weeks (on average 14-20 days).
Also, to prepare for removal procedures, you can glue the Salipod callus patch to the wart (2 days), or cut off the spine with nail scissors.
2) Instrumental removal.
a) Soft laser. (read more) Your wart will evaporate under the action of the laser. You will have a deep wound at this location. The wound will heal in 10-14 days.
Here is a video of laser wart removal:
Here are the reader reviews: link
b) Liquid nitrogen. (more about this method) Deep freezing of tissue occurs. A bubble forms. It will be soooo much and then it will hurt!! Heals in 14 days.
Here is a video of cryodestruction of a wart on the foot with liquid nitrogen:
And here are the reader reviews: review 1 and review 2
c) Radio wave radiation (Surgitron apparatus and others). (read more) The same effect as from a laser - evaporation of tissue. And all that will remain of the wart is a deepening wound.
Here is a video of the removal of a plantar wart using a radio wave with a loop tip (watch from 40 seconds):
Here's a reader's review: link
d) Surgical removal of the wart with a scalpel. It is performed under local anesthesia. Stitches are applied. It is used very rarely, since laser or radio waves are much more convenient, simpler and less traumatic.
d) Electrocoagulation. The wart is burned out with an electrocoagulator. This is the same scalpel, only electric. It is now rarely used in large clinics.
Prevention
The main preventive measure for plantar warts is to prevent infection with the human papillomavirus. To do this, you should use exclusively individual shoes in public places such as a swimming pool, bathhouse. Cosmetic care for the soles is of great importance: pedicure, removal of dead cells (peeling), and people who have problems with the shape of their feet need to use orthopedic insoles. If you have hyperhidrosis, you need to choose shoes made from natural materials, maintain hygiene, change socks frequently and use antiperspirants for your feet. If the soles are prone to dryness and cracking, be sure to use moisturizing creams and baths.
If the pathogen has already been detected in the body, then secondary prevention is required, which consists of the use of antiviral drugs and drugs that stimulate the immune system.
Associated symptoms
Among the accompanying signs, the following symptoms are often noted:
- increased oiliness of the skin;
- the skin takes on a rough appearance and becomes bumpy to the touch;
- hair follicles become inflamed (due to ingrown hairs);
- red dots appear;
- redness and soreness of the skin are observed.
Most often, the disease occurs in women. In most cases, it is associated with improper shaving, as well as foot care before and after the procedure. Hormonal imbalances are mainly observed in the young population. Therefore, when the first spots appear, you should consult a doctor and begin treatment of the pathology at the initial stage of development.
Diagnostics: where to go and what tests to take
You should definitely visit a doctor if you know that black spots on your feet and calves are not caused by improper shaving, staining from shoes, or low-quality cosmetic products. You should consult a dermatologist for help and then undergo the necessary tests. It is difficult to discover on your own what it is and why it appeared. The spots are not a separate disease, but only indicate disorders in the body.
A specialist may prescribe a general blood test to identify possible inflammatory processes or weakened immunity. Often, just an examination and scraping from the affected area is enough. Such procedures are necessary to exclude or confirm skin diseases.
Darkening of the toenails
There are many more reasons for the formation of dark spots under the toenails than may seem at first glance. One of the most common is damage (or subungual hematoma) to the plate. If you pinch your finger or lightly accidentally hit it, then after a while a black spot will form on your leg. They are explained by rupture of capillaries and accumulation of blood in one place. Apart from this, the reasons that cause a black spot on the toe are:
- Pigmentation disorder. Some people are dependent on external conditions: water quality, sun intensity, frost or heat. Subtle defects often appear on the skin, hair and nails. Various rashes, dark grooves and dots are more of a concern seasonally, so tracking down the provoking factor is not so difficult.
- Insufficient liver function. In some diseases of the gastrointestinal tract, the pigment is not excreted from the body and accumulates in the skin. The nail plates also change in color to a more yellow or brownish color.
- Fungal infection. Mold fungi often affect fingers and nail plates. Not only do blackheads form on the toenails, but almost the entire nail changes. It becomes brittle, yellow (in some cases greenish or gray), begins to exfoliate and collapse.
- Oncological disease. With a large accumulation of metastases in the body, neoplasms of various colors may appear on the skin. You need to pay attention to your general health and immediately consult a doctor.
Poor-quality varnish or cosmetic product can cause specks and black spots under the nails. After identifying a defect, the first thing to do is to abandon any means that could cause the problem. If it does not disappear (or does not become less noticeable) within a few days, then consultation with a specialist is required.
The easiest way to remove spines
There is a wonderful folk method to get rid of spines. Great because it's very effective and simple. True, it is suitable mainly for children and young people. It is at this age that the skin on the heel has not yet lost its softness and has not acquired corns (dense layers of keratinized skin). The method involves walking barefoot for a long time in the summer.
It doesn’t matter at all where the walks take place: on grass, earthen paths, forest paths or a sandy shore. Due to abrasion of the skin, warts disappear imperceptibly, especially on the heel.