Pearlescent papules are neoplasms of a transparent or white color and small in size. Pearly papules form on the genitals. Most often men suffer from this. To date, the exact cause of the development of the disease is not known. The formations are benign, but cause not only physical discomfort, but also psychological discomfort. The diagnosis is made based on examination by a specialist.
You cannot remove papules on your own. Representatives of the stronger sex need to regularly visit a urologist for preventive purposes.
What is a papule
The papule is represented by a rash that can appear on the dermis and mucous membranes. If one pimple appears, don't worry too much. But when a lot of pimples form, it not only causes discomfort, but also causes emotional stress. The papule is represented by a vesicle that has a diameter of 1–3 mm. This bubble is sharply defined and dense.
It is slightly elevated above the dermis. Papules on the dermis are like dense nodules that are like small balls that appear on the surface of the dermis.
These suppurative pimples are usually accompanied by swelling and suppuration of the dermis. When pressing on the papule, a change in its color is noted. It becomes not so red, but rather a pink, pale color.
The formation does not show a white, inflamed head (as on a pustule). Most often, the formation of these pimples occurs from comedones (closed). If the papule has formed from an open comedon, a dark plug and an enlarged mouth of the hair follicle can be seen. A papular rash can leave cosmetic defects (scars) on the dermis. But this is usually with a severe form of the rash.
What causes warts?
Our readers successfully use Papilite to treat papillomas.
Seeing how popular this product is, we decided to bring it to your attention. Read more here... The cause of warts on the human body lies in the papilloma virus (HPV). It is quite common. Almost every adult is infected with some type of HPV, but most often several at once. In addition, in many countries the prevalence of this infection is steadily increasing and there are many variants of what causes warts to appear.
This virus infects mucosal cells and epithelium. Modern medicine is familiar with 118 types of papillomavirus. Each of them is associated with a particular disease. It has been established that about 60% of types provoke skin diseases, and approximately 40% of the rest cause diseases of the mucous membranes, most often affecting the genitals.
The likelihood of contracting the papilloma virus depends on several factors:
- how active the virus is in the person from whom the infection occurs (more on this below);
- intensity and nature of contact;
- How strong the immune system is of the infected person.
The papilloma virus affects only the skin and mucous membranes. The virus cannot enter the bloodstream; it does not affect other organs. It is important to determine the type of illness in time, because there is also a human papillomavirus with a high carcinogenic risk.
In order to get a complete understanding of the characteristics of HPV, you need to know what structure human skin has. And it consists of two large layers: the epidermis is the upper layer, the dermis is the lower. The epidermis, in turn, is also divided into layers (listed from top to bottom): horny, spinous, shiny, granular, basal. In the basal layer, cells divide.
Over time, epidermal cells move from the lower to the upper layer. This process is accompanied by the maturation of epidermal cells. The stratum corneum of the epidermis, which is located at the very top, gradually gets rid of dead cells. Peeling of the skin occurs.
Why does the author of the article pay such attention to the structure of the epidermis? It's very simple, the development cycle of HPV completely depends on the development of epidermal cells. HPV multiplies within the basal layer of the epidermis, located at the very bottom. The virus cells mature and move along with the epidermal cells to the upper layers. The moment HPV reaches the stratum corneum of the epidermis, the virus becomes infectious.
Features of HPV include the ability of the virus to exist in two states:
When inactive, the virus is located in the basal layer of the epidermis. In this case, cell division occurs slowly. But this virus is not contagious because it does not rise to the surface of the skin. HPV can remain in this state for a very long time.
The active state is characterized by the rapid proliferation of virus cells. It almost always reaches the surface of the skin and is dangerous to others.
If a person becomes infected with HPV, the virus remains on his skin and mucous membranes throughout the patient’s life. For many infected people, the virus can remain in an inactive state for years without revealing itself in any way.
This is why most people infected with HPV show no signs of infection. In some cases, the virus becomes active. Usually this transition is associated with a decrease in immunity. Active HPV immediately becomes contagious and can cause warts to appear on the body.
It becomes clear that warts on the skin appear when the virus becomes beyond the control of the immune system. Although the opposite situation is also possible: already formed warts under the influence of general and local immunity are capable of self-resolution. Such resolution occurs in 20% of all cases within two months; 30% of cases resolve within the first three months; 50% of approvals occur within two years.
Warts on the body of children are more likely to resolve on their own. In adults with reduced immunity and with a long course of HPV, spontaneous resolution is extremely rare.
The disease can occur in a variety of ways. Here are two options for the possible course of the disease: with HPV treatment and without treatment.
Variants of the behavior of warts in the absence of treatment:
- warts increase in number and size;
- warts remain unchanged for a long period;
- warts disappear on their own.
Options for the behavior of warts during treatment:
- warts disappear completely on their own already at the first stage of treatment;
- warts disappear gradually as the treatment process progresses;
- Warts, despite intensive treatment, are resistant and do not change at all.
Here you need to understand that the process of existence of warts is very different from the course of many diseases. If most diseases begin to progress without appropriate treatment, and when receiving the right treatment, a significant improvement or complete recovery is observed, then in the case of warts the situation is different.
Even the most progressive treatment for warts may be ineffective and, conversely, warts may disappear without any treatment; sometimes a pink spot may remain on the skin after the wart.
Returning to the question of the unpredictable behavior of warts, we need to remember the likelihood of relapse after complete recovery. Unfortunately, none of the current treatment methods can eradicate HPV.
Only the warts themselves are eliminated, while the virus hides in the depths of seemingly healthy skin. During activation of the virus, a relapse occurs and the warts return again. The probability of relapse of the disease is 30%.
70% of such formations are simple warts, they are also called vulgar. This type occurs mainly among schoolchildren. The sizes of round papules vary from a pinhead to a large pea. The surface of the wart has uneven edges and a keratinized layer of flesh-colored, grayish or brown color.
Flat or juvenile warts are much less common. This is only 4% of the total. They appear mainly in children, adolescents and young adults. These are small papules, flesh-colored, with a smooth surface. The shape of juvenile warts can be round or polygonal. Such warts live in families and are localized mainly on the back of the hands and feet, face, and oral mucosa. In addition, they can appear in the rectum, on the skin of the penis and cervix.
Filiform warts appear as soft papules. Their color can vary from flesh to dark brown. Often these warts are pedunculated. Most often they can be found on the neck, eyelids, groin, under the mammary glands and in the armpit area. They are usually small 1-4 mm, but in some cases their sizes can reach 3 cm.
A pronounced tendency to self-infection (autoinoculation) confirms their viral origin. The connection between warts and hormonal disorders of the body is eloquently demonstrated by their appearance during menopause, obesity, diabetes, and pregnancy.
Palmoplantar warts most often appear in young and old people. The percentage of these warts from the total number is 34%. These are dense formations with horny layers. Plantar warts are difficult to diagnose because in appearance they are very similar to calluses and horny syphilitic papules. Read more in our article - Plantar warts: quick treatment, main causes and photos.
Palmoplantar warts can appear on the pressure area of tight shoes and cause unbearable pain while walking. People with excessive sweating of the hands and feet suffer from the rapid spread of warts, which are very difficult to treat.
[youtube.player]
Papules and plaques.
Mostly papules are benign in nature, but they are also observed in some infections. The papule also manifests itself in the early stage of cancer, before it becomes ulcerative.
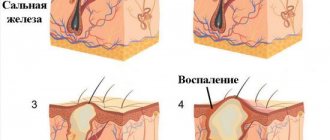
• Quite often normal hair follicles and sebaceous glands appear as papules on the penis, especially its ventral surface. The sebaceous glands are clearly visible as small yellow homogeneous nodules accessible to palpation, located more or less symmetrically. They are often regarded as Fordyce spots. Hair follicles typically produce hair. In contrast, genital warts are inhomogeneous, similar to cauliflower inflorescences, and molluscum contagiosum papules are fleshy, round, with umbilical depressions in the center.
• Pearly papules are multiple, small (1-3 mm in diameter), millet-like, do not differ in color from the skin and are located around the circumference of the penis along the coronal sulcus. They are found in 10% of men 20-40 years old, mainly in uncircumcised men.
Although they are often confused with condylomata acuminata (as mentioned, they are inhomogeneous, cauliflower-like and unevenly distributed), pearly papules are not associated with infection and do not cause discomfort. They do not require treatment. These are the sebaceous glands of the foreskin, apparently producing smegma. They are still sometimes called tyson glands (after the name of Tyson, who described them). • Fordyce spots. • Lichen planus and psoriasis. • Molluscum contagiosum. • Genital warts. • Secondary syphilis.
In most cases, these are typical papules and plaques, mainly around the circumference of the glans penis, red-violet or white, round, often similar to candidiasis. Unlike other manifestations of lichen planus, they are rarely accompanied by itching. Wickham's mesh and erosive elements of rashes on the penis are rarely observed.
For psoriasis, as for lichen planus, manifestations on the penis are atypical, due to the moistening and maceration of this area of the body. Peeling characteristic of psoriasis is rarely observed, mainly in uncircumcised men. Psoriasis appears as thick, red papules or plaques with clear borders. They are rarely accompanied by inflammation.
Psoriasis usually affects other parts of the body (particularly the knees, elbows, and scalp); sometimes its first manifestations appear on the penis, usually on the glans and foreskin. Such cases must be differentiated from syphilis.
A widespread benign viral infection of the skin and mucous membranes. Children usually become infected with it from peers, adults - through sexual contact. On the penis and scrotum it manifests itself as multiple small soft hemispherical papules, often with an umbilical depression or plug in the center. When pressed, curdled contents are released from them.
Papules are easily removed by cryodestruction or cauterization, but disappear without treatment. Their very appearance indicates that the patient does not use a condom and is indicated for HIV testing.
The disease is quite common, and its prevalence is increasing, especially among sexually active young people. Condylomas acuminata are pointed, branched formations that are caused by the human papillomavirus (in contrast, condylomas lata in syphilis are flat). They look more like warts than ulcerations.
They are located mainly on moisturized areas (in particular, on the coronary sulcus), but sometimes on the tip and shaft of the penis, the scrotum, in the anus and on the oral mucosa. Genital warts are small, single or grouped, with a shiny surface, fleshy, similar to cauliflower inflorescences. Human papillomavirus infection is very contagious, but, like herpes, it can occur hidden. While remaining asymptomatic, the infection is often accompanied by viral shedding.
The most common non-oncogenic types of human papillomavirus are 6 and 11; oncogenic types 16 and 18 are less common, causing precancerous changes and malignant neoplasms, including squamous cell carcinoma of the penis, anus and cervix. Sometimes genital warts look like pearly penile papules.
This is a manifestation of secondary syphilis - multiple flat papules (less often nodules), soft, with a smooth surface, weeping or macerated, reddish-brown or gray. Eventually they merge into large plaques, often resembling cauliflower inflorescences. The differential diagnosis of condylomata lata includes nonulcerative papules of psoriasis, lichen planus, scabies, squamous cell carcinoma, which initially appears as a firm, painless nodule but later ulcerates, and Reiter's syndrome, which may also be accompanied by nonulcerative rashes on the penis.
[youtube.player]
Pearly papules on the glans penis occur in 10-48% of men aged 15-35 years. They are normal and should not cause concern. This is not a disease. This type of papulosis is not contagious and does not require treatment. However, you need to make sure that these are pearlescent papules and not pathology.
Signs of pearly papules
Almost half of the male population of the planet exhibits pale flesh-colored nodules, 1-3 mm in diameter, smooth and shiny, encircling the head of the penis.
These nodules (papules) are dense, painless, of the same size and shape, located in one or more rows. The similarity of papules with pearls gave rise to calling them “mother-of-pearl ring” and “pearl necklace”. Normally, these are absolutely harmless formations; they do not itch, do not bleed, or cause any inconvenience. Fears about the transmission of papules to a sexual partner or their spread throughout the reproductive organ are also unfounded.
Expert opinion
Sakania Luiza Ruslanovna
Dermatovenerologist, cosmetologist, trichologist
Ask a Question
Sometimes papules still occur on the head of the penis, on the scrotum, at the base of the penis, located in groups and individually. Papules appear during intense puberty and may decrease in size as they age.
In blacks, these formations are detected much more often than in men of other races. A predisposition to the appearance of papules in “uncircumcised” representatives of the stronger sex has been noted.
Differences from other types of rashes
Pearlescent papules are safe and do not cause harm to health. But there may be other rashes on the penis (molluscum contagiosum, condylomas). They are a sign of pathology.
Unlike pearly papules, these formations are of unequal size and shape. Condylomas grow on a thin stalk. With molluscum contagiosum, the formations have an umbilical depression in the center and cheesy contents inside. Diagnosing pearly papules is quite simple.
This does not require extensive laboratory testing. Diagnosis can be made by simple examination or use of a dermatoscope. In rare cases, papules can become infected. A biopsy of the affected area of skin may then be required.
Causes of pearly formations in men and whether they are contagious
A theory has been proposed that papules on the penis in the form of mother-of-pearl pearls are a deviation from the norm. This feature is inherent at the genetic level. This is confirmed by the high frequency of occurrence in the population - up to 48% of all men.
The formation of pearly papules is influenced by the following factors:
- circumcision - the frequency of detection of nodules in persons who have undergone surgery is much lower;
- disruption of the sebaceous glands;
- changes in hormonal levels in adolescents and increased cell proliferation against this background provoke pearlescent formations;
- lack of personal hygiene and the associated aggressive effect of smegma on the mucous membrane of the penis.
Years of observation have made it possible to establish that mother-of-pearl pearls are not caused by an infectious factor - in epidemiological terms, complete safety is guaranteed.
They pose no danger to the owner and do not affect the genital area or urinary system. There is a misconception that papules in the area of the head of the penis are caused by the human papilloma virus. This theory is incorrect; the histological structure of pearls does not correspond to papillomas with HPV. Pearlescent nodules are often confused with genital warts. Such overdiagnosis is justified. HPV is widespread, and some types of the virus pose a cancer risk. Inexperienced doctors can easily confuse visible pearlescent small papules with condylomas and prescribe irrational treatment.
The presence of HPV may be indicated by:
- the appearance of a papular rash on the foreskin and head of the penis at the same time;
- color change from pearlescent to purple;
- the appearance of a burning sensation, pain and erosion.
There are methods of screening studies that can reduce the likelihood of error to zero.
Causes of pearly papules
Doctors express different opinions about the causes of “pearl necklaces” in men.
Existing hypotheses can be roughly divided into three groups: Papules are vestigial remains of spines on the penis, preserved in other primates. Chimpanzees are considered the closest “relatives” of humans. Male chimpanzees have small spines on their penis. They help increase the sensitivity of the penis and reduce sexual intercourse, which is an important requirement for survival in the wild. In humans, everything happens exactly the opposite, and unnecessary thorns have disappeared in the process of evolution.
However, “wild” genes sometimes reward their carriers with a “mother-of-pearl ring.” Papules are the result of the proliferation of epithelial cells of the excretory ducts of the glands located on the penis. Intensive synthesis of male hormones during puberty increases the secretion of the glands of the head of the penis.
Expert opinion
Sakania Luiza Ruslanovna
Dermatovenerologist, cosmetologist, trichologist
Ask a Question
The secretion released in large quantities (smegma) irritates the mouths of the glands and provokes the proliferation of epithelial cells. Other scientists suggest the development of papules directly from the epithelial layer of the head of the penis. When, under the influence of hormones, individual sections of cells begin to rapidly divide and form characteristic nodules.
The 2nd and 3rd hypothesis is supported by the fact that papules are diagnosed mainly in “uncircumcised” men, in whom smegma accumulates in the skin fold (prepuce) covering the head.
Etiology
Mother-of-pearl or pearly papules are small neoplasms up to 2 mm in size that can appear on the foreskin of the male penis, forming a ring around the crown of the glans. This disease is not one of those diseases that are transmitted through sexual contact. This feature eliminates the risk of infection of the sexual partner.
Young men of adolescence are likely to develop papules, but as they approach the age of puberty, they disappear. According to experts, papules indirectly confirm the presence of increased sexual activity in a man.
There is also an assumption that papules arise due to blockage of the sebaceous glands located on the head of the penis. But the statement that pearly papules are formed due to promiscuous sex life or insufficient hygiene is erroneous.
Papules should not be removed on your own, as this can cause an infection of the penis. If the papules cause itching or any discharge is detected, you should immediately consult a venereologist to diagnose or exclude the possibility of a sexually transmitted disease.
If the condition remains unchanged, pearly papules do not require any treatment.
Developmental symptoms
Pearly penile papules develop asymptomatically.
They are a small growth of tissue surrounding the head of the penis, which has a tuberous base. The papules are hard to the touch, can reach several millimeters in size, and appear close to each other. The surface has a shiny matte color, resembling small pearls in appearance. Typically, papules grow in the form of a ring, usually in several rows. The owner of a skin defect may not even notice this phenomenon in himself.
If we also turn to statistics, then rapid growth of papules is observed during puberty, when a teenager experiences frequent secretion of secretions from the glands of the penis. After puberty, at age twenty-five, the rash decreases significantly.
Removal methods
There is no need to remove the papillary crown, because it is not hazardous to health and does not cause physical discomfort. But many men consider this a defect and want to get rid of it. Some young people even try to do this on their own, which is strictly prohibited.
Self-medication can result in many complications. When plucking with tweezers, tissues are injured. Infection easily penetrates into wounds. Treatment with remedies for papillomas and warts leads to inflammation and swelling. As a result, the head loses sensitivity. Dermatological reactions sometimes occur.
If a man is determined to get rid of white papules on the head, he should resort to one of the following methods used in medical institutions.
The most effective and painless method. The tissue of the growths is broken down at the molecular level. Neighboring cells are not damaged. Recovery occurs quickly, no scars remain.
Point exposure to radio waves. As a result of irradiation, free radicals are released that destroy the cells of the papules. Shallow scars may form.
A high-frequency current dries out the growths, after which their remains are removed surgically. Scars often remain after manipulation. The procedure requires anesthesia and subsequent painkillers.
Burning with liquid nitrogen. After the procedure, the treated skin turns white, then a painful blister forms in this place. Over time, it is replaced by a crust. Complete healing occurs within 1.5-2 weeks, but a pigment spot may remain. The procedure is dangerous because it affects adjacent tissues and deep layers of skin.
Regardless of the method chosen, you need to be prepared for the fact that hirsutoid papillomas will reappear over time. This is a physiological feature that cannot be eliminated. True, in some cases, circumcision of the foreskin helps solve the problem forever.
Pearly papules on the head are completely harmless. Doctors are inclined to believe that there is no need to remove them even for cosmetic purposes. A mother-of-pearl necklace should not be considered a disadvantage. Small growths are almost invisible, but large ones can be useful. Many women note increased sensations during sex with a partner with this feature due to additional stimulation.
[youtube.player]
Small nodules are localized on the circumference of the head of the genital organ of many men. Such formations quite often frighten representatives of the stronger sex; they can be mistaken for a rash of venereal origin. But such nodular formations are called pearlescent papules and are considered, in fact, a normal phenomenon.
Diagnostics
Pearlescent papules in men require diagnosis only for the purpose of accurately identifying them and eliminating the likelihood of developing other sexually transmitted diseases. As a rule, a specialist conducts only an external examination. Doctors rarely resort to deep analysis.
What diseases do purple papules resemble:
- Genital condyloma, papilloma - the arrangement of the heads of papillomas on a sharp stalk, in a scattered form (and not in rows, like papules). The rash varies in size.
- Costagious molluscum is a viral disease related to smallpox. It differs from papules in that it has a funnel-shaped depression. It can also affect mucous membranes. At the same time, when pressing on such a rash, a curdled mass may appear.
How to distinguish condyloma from papilloma?
- 1 What are neoplasms?
- 2 What are the types of condylomas?
- 3 What are the different types of papilloma?
- 4 How to distinguish between women and men?
- 5 Are there significant differences in treatment methods? 5.1 Surgical removal
Every person needs to know the difference between papilloma and condyloma, in order to be armed with these concepts and understand that to diagnose and, as a result, not be scared, not harm others, make the right decision about getting rid of it or preserving it, just be informed and knowledgeable, it is possible to help people in advice on this problem.
The main difference between papilloma and condyloma is the localization of growth.
What are neoplasms?
By papilloma we mean a benign formation, which looks like a small tubercle of flesh-colored or pink color, has a large number of shapes and is attached to human skin with the help of legs of various sizes. The growth is soft and springy to the touch. Often formations occur in the following areas of the body:
- hands;
- neck;
- armpits;
- face;
- legs.
The formation of such growths indicates the presence of human papillomavirus. It can be present in the human body and not manifest any special signs.
If the protective mechanisms of the human body are violated, then papilloma will definitely make itself felt. If papillomas and condylomas occur, you should not stay in the area of intense sunlight. The appearance of a growth is provoked by the following factors:
- bad habits;
- alcohol;
- smoking;
- promiscuity of sexual life.
Papillomas in men cause discomfort and lead to the development of cancer. In any case, this neoplasm gives a person a feeling of discomfort and disgust. From a medical point of view, condyloma is an inflammatory formation that tends to appear on the skin or mucous membranes of internal organs. In addition, this formation is prone to grouping, ultimately leading to the combination of small condylomas into one large one. It is transmitted to other people through sexual intercourse or through sharing personal hygiene products. From the moment of infection with the virus until the appearance of the lump, it takes from 7 days to 6 months.
Condylomas can be broad or pointed and can be caused by syphilis or HPV infection. Return to contents
What are the types of condylomas?
The following varieties are distinguished:
- Wide growths are characterized by a spacious base for attachment to the skin. They follow secondary syphilis, and sometimes have a malignant nature when they occur on the mucous membrane of the cervix in women.
- Condylomas acuminata are a thin formation with a narrow stalk necessary for attachment. They are not at all dangerous if they are not inflamed and healthy. But experts recommend getting rid of them through surgery, since they cannot be cured by other means.
Return to contents
What are the different types of papilloma?
Based on their nature, they are divided into 5 types:
- Simple papillomas are the most common among all known. The peculiarity of this type is that the neoplasms from the very beginning are tiny in size and not noticeable, but soon they grow and become rough and hardened.
- Flat in the shape of an oval or circle, not very noticeable on the body due to the light shade, they tend to appear in groups and do not protrude much above the skin level.
- Pointed ones affect the mucous membrane of human organs.
- Thread-like with a characteristic thin stalk inherent specifically to this species. They form from a yellow spot and affect delicate areas of the body of people aged 40 years and older.
- Internal papillomas cause serious problems, since they cannot be recognized by their appearance. They can grow inside a human organ.
Condylomas and papillomas differ in shape, routes of transmission and place of growth. Return to contents
How to distinguish between women and men?
Although both formations appear with HPV, they are caused by different types of HPV - this is the main difference between them. There are other differences that are characterized by slightly different aspects. The conditions that determine the difference between papilloma and condyloma are simple:
- Papillomas look different from the outside. They are presented in the form of a figure, but condylomas have an arbitrary shape.
- The locations of the neoplasms also differ. Papillomas prefer to appear on the skin, while condylomas prefer to appear on the mucous membranes, most often on the penis in men and in intimate places in women.
- Papillomas are not sexually transmitted, unlike condylomas.
- The difference is that they are different in appearance. Condylomas look unaesthetic.
- Papillomas are harmless and are not accompanied by the need to use any surgical actions than condylomas, which are dangerous because they often become infected and require prompt removal.
Return to contents
Are there significant differences in treatment methods?
Condylomas and papillomas will require complex treatment, but the methods for their removal are different.
Treatment of growths in intimate places has certain peculiarities, since the mucous membranes of the genital organs are sensitive. Therapy depends on the degree of neglect. First of all, you need to treat by using a medicine as prescribed by a specialist that will effectively resist the virus, increase human immunity and destroy the structure of the growth. If it is not possible to get rid of the tumors in this way, then they resort to the surgical method.
It is strictly forbidden to wipe the growths with solutions containing salt and independently follow the advice of traditional medicine.
The methods of treating these two formations, on the one hand, differ only slightly, but on the other hand, they are somewhat similar. That is, there are no significant differences in the treatment. Basic stages of therapeutic actions:
- Fighting the virus. A pharmaceutical drug is prescribed, the task of which is to destroy and weaken the virus.
- Increasing the protective functions of the human body. At this stage, a drug is prescribed to improve immunity.
- Surgical intervention by mechanical action.
- Preventive therapy of formations, which involves taking medications to prevent the occurrence of growths.
- Virus surveillance and preventive measures.
For papilloma, the latter procedure is largely not performed. The operation is necessary only if the patient complains of physical inconvenience and moral contradictions. As for condylomas, the question of their removal is clear, since they pose a threat to human life - they contribute to the development of tumors.
To remove papillomas, due to their “delicate” localization, the most painless methods should be used. Return to contents
Types of treatment for pearly papules
Despite the harmlessness of papules, almost 40% of their carriers want to get rid of them. Modern medicine offers three ways to solve the problem:
- Cryodestruction of papules is carried out by local exposure to extremely low temperatures. Before the procedure, a local anesthetic is injected. The freezing effect is achieved by instant cooling with liquid nitrogen. Nitrogen is applied pointwise to the papule using a cryo-tip of the required diameter. Ice crystals form in frozen tissue, cell membranes are destroyed and the cell dies. Blood circulation also stops. After the procedure, redness and swelling, mild pain, and tingling occur. On the first day, an inflammatory reaction develops on the treated surface and lasts up to 2 weeks. At this time, dead tissue is sloughed off and the healing process begins. Cryodestruction is performed without lengthy preparation, has a low risk of infection, and does not leave scars or scars.
- Electrocoagulation of benign neoplasms is carried out with an electric knife, which excises tissue and at the same time coagulates blood vessels. The operation takes place under local anesthesia. A thin crust forms in the excision area, which heals within 10 days without scar formation.
- Laser coagulation is the most effective and safe method for removing pearlescent papules. The procedure is performed under lidocaine anesthesia. Carbon dioxide-based laser equipment literally “burns out” the papules. One row of mother-of-pearl ring is removed in the first procedure. If there are papules in several rows, subsequent procedures will be required.
After all three types of procedures, the head of the penis needs to be looked after. Within 2 weeks the wound will heal and the crust will dry on it.
Expert opinion
Sakania Luiza Ruslanovna
Dermatovenerologist, cosmetologist, trichologist
Ask a Question
The wound is treated daily with a 5% solution of potassium permanganate. You can’t peel off the crust; it should fall off on its own.
Sexual activity is also contraindicated during treatment. Unfortunately, there is no treatment method that will get rid of pearlescent papules forever. Once removed by any means, they may reappear.
Is it necessary to remove papules on the penis?
Since such neoplasms do not cause any harm, but only cause cosmetic discomfort, specialists do not force the papules to be removed. But if the patient is concerned about their presence, then there are several ways to get rid of unwanted formations.
- The first method is cryotherapy. This procedure involves exposing skin cells to cold, which promotes the death of unwanted formations.
- The second method is electrocoagulation. With this method, the skin is exposed to a direct electric current, which causes dissonance of the salts contained in the skin and interacts with the ions in the system, which leads to the deposition of helium.
- The third method is laser coagulation. Used in eye surgery, but also used in other areas. The tissue is exposed to microwaves. With this method, the patient can undergo surgery without loss of blood, since microwaves penetrate the blood vessels, coagulating the contents. Human tissue is heated, for example, gentle heating (no more than 100 degrees).
This procedure is one of the most common used in modern cosmetology conditions. The field of influence on the pearly skin of the laser, imperfections are reduced, small crusts remain at the site of the defect, which disappear after a certain period of time.
- The last option is cosmetic surgery. It is one of the branches of plastic surgery. The purpose of this intervention is to eliminate skin imperfections and defects.
It is worth noting that after any of the above operations, it is necessary to protect yourself from any sexual contact for the period of tissue restoration.
If there is not enough money for removal operations, there is a way to get rid of the shortage at home. But it is worth noting that the result will require patience and regular repetition of therapy, while the deficiency will not be completely eliminated, but only masked.
Recipe for a remedy for removing papules: 50 grams of bee honey, 1 teaspoon of aloe, sea buckthorn oil for the eye and 1 gram of mumiyo. Mix all this and apply to the skin of the penis every evening before bed. The mass should have the consistency of sour cream.
Sakania Luiza Ruslanovna
Dermatovenerologist, cosmetologist, trichologist
Ask a Question
As a result, the unwanted neoplasms themselves will only become smaller in size, but will not be completely eliminated.
Thus, pearlescent skin growths on the penis do not pose a serious danger to their owner. The disease is asymptomatic and does not cause any consequences. It can only bring cosmetic discomfort to the patient, which can be eliminated if desired using one of the methods available today: using exposure to low temperatures, nitrogen, electric current, laser removal, conventional cosmetic surgery, in general, there are a lot of ways. When choosing a removal method, you should consult your doctor. It is also worth noting that pearlescent papules are not a sexually transmitted disease and are not sexually transmitted.
Treatment of papules in women
These pearlescent papules are incurable.
Claims about their successful breeding are not considered proven. Jojoba oil and Retin-A are used as a deterrent to prevent the spread of granules. In addition, Fordyce granules can be removed using microcurrent electrocoagulation or laser. This procedure is painless and is performed by a doctor under local anesthesia. The patient returns to a normal lifestyle immediately after removal. Care after the procedure is simple, using special preparations.
After removing the granules from the genitals, it is necessary to observe sexual rest for two weeks. However, it should be noted that in 80% of cases the disease returns within 2 or 3 years.
Our specialists
- Sign up
- Sign up
- Sign up
Reviews
- The plastic surgery of the frenulum was performed by the doctor Mamedov Khalit. Thanks to the doctor and the clinic, everything went quickly and easily. I was preparing for a long time, I was afraid, but it turned out to be 10 minutes and it’s ready, thank you!
NovelApril 12, 2021 at 02:54 pm
- My husband suffered from Peyronie's disease. I had to take him to the doctors in Lazmed. Luckily they were able to help him. Many thanks to the doctors - they are experts in their field, excellent specialists.
Grateful wifeDecember 27, 2021 at 11:55 am
- Doctors at Lazmed Clinic helped me cure infertility. Thanks to their experience and the right treatment, I will soon become a father. I want to express my gratitude and deep gratitude!
PeterNovember 25, 2021 at 12:10 pm
- For medical reasons, I was prescribed removal of the foreskin. To be honest, I was worried about this operation. But I was reassured by the doctor, who explained how this happens and what to expect after the operation. Everything went perfectly.
VyacheslavDecember 25, 2021 at 11:00
- I would like to say a huge thank you to the urologist at the Lazmed Clinic. With his help and the right approach to treatment, it was possible to avoid complications from prostatitis and become a healthy, full-fledged man. The main thing is not to delay treatment of the disease.
DimaDecember 20, 2021 at 5:37 pm
- At the Lazmed Clinic he treated a well-known male disease - prostatitis. 10 sessions were enough for me to recover and forget about the painful nights with this disease! Laser treatment has proven to be undeniably effective.
AlexeiJanuary 11, 2021 at 01:56 pm
- Having turned to the Lazmed clinic for help in solving a delicate urological problem, I received qualified treatment, and most importantly, I was able to get rid of the disease in the shortest possible time. Many thanks to the doctors!
GennadyJanuary 20, 2021 at 4:22 pm
Small flesh-colored tubercles surrounding the head of the penis are often a reason to consult a urologist. Men consider pearlescent papules a sign of a sexually transmitted disease. Is this true, and in what case is it really necessary to visit a doctor?
Mother-of-pearl papules are nodules that do not have a cavity inside and rise above the surface of the skin. They have a cone shape and a diameter of no more than 3 mm. Their surface is smooth with a shiny tint, which is why they are called pearl.
The papules are absolutely painless to the touch; when pressed, there is no discharge from them. They are located at the base of the head of the penis, as if encircling it with a ring in one or two rows. In some cases, they form on the head itself.
Pearly papules appear in 10–45% of men. This depends on established national and religious traditions - men who have been circumcised have significantly less rashes.
The photo shows pearly papules on the glans penis
Why do they appear?
Doctors can only guess about the causes of the rash. There are several opinions:
- One of them is the increased work of the sebaceous glands and their blockage. Partial confirmation of this version is the rare appearance of papules in men with circumcised foreskin.
- Another theory for the formation of papules in middle-aged men is cell proliferation. Their increased reproduction causes similar harmless proliferation of the epithelium. The appearance of papules is completely unrelated to the orderliness of sexual life or insufficient hygiene.
- In adolescents, pearly papules are associated with hormonal changes and the secretion of smegma - sebum mixed with moisture and dead cells of the surface layer of the skin. It is formed in large quantities during the period of greatest sexual activity.
Rashes of similar localization are possible with primary syphilis, genital warts and molluscum contagiosum. A simple examination is enough for a specialist to distinguish a pearly papule from the manifestations of the mentioned diseases.
Syphilomas (primary syphilitic ulcers) are bright red in color, larger than the papule in size and differ from it in appearance. They have flat edges and a flat bottom, under which the seal can be felt. They are localized not only on the head of the penis, but also on other parts of it.
Genital warts are the result of infection with the papilloma virus. They are distinguished from papules by localization. They are located not only on the head itself and around it, but also at the base of the penis, on the frenulum, next to the anus and on the mucous membrane of the ureter.
You can distinguish a condyloma from a papule by its appearance. It is a skin growth attached to the surface of the skin with a thin stalk.
Molluscum contagiosum also does not have such a clear localization as pearly papules. Ball-shaped formations with a depression in the middle can appear on the genitals, pubic area, buttocks and inner thighs. When pressed, curdled contents appear from the formations.
But this does not mean that you should ignore the symptoms that may appear along with papules:
- itching and burning sensation in the genital area;
- pathological discharge with a foul odor;
- pain in the area where the papules are located;
- problems during sex.
Very rarely, pearly papules on the glans penis can become inflamed. But this happens due to infection when a man tries to get rid of them on his own.
An initial examination may be sufficient to make a diagnosis. Sometimes, to clarify it, a histological examination of the papule is carried out. Distinctive features of the papule:
- dilated thin-walled skin vessels;
- the presence of multinucleated fibroblasts or star-shaped cells;
- increased amount of connective tissue.
We suggest you familiarize yourself with how eczema differs from atopic dermatitis
Pearlescent papules are not transmitted through sexual contact.
Why do men want to get rid of pearly papules so badly?
Any cosmetic defect on the human body can cause the development of psychological abnormalities - isolation, shyness and unsociability.
The situation is much more serious with cosmetic defects located on the genitals. This can greatly affect your sex life. Expert opinion
Sakania Luiza Ruslanovna
Dermatovenerologist, cosmetologist, trichologist
Ask a Question
Even despite doctors’ statements that there is no need to remove pearlescent papules, more than 90% of men want to get rid of them once and for all. The worst thing is when they try to remove pearlescent papules on their own using cauterization with iodine or excision with nail scissors.
Under no circumstances should this be done, since each removed papule is an “open gate” for infections, and even complete sterility does not provide any guarantee that you will not harm your body. The only thing that really works effectively and does not leave open wounds is toothpaste for smokers.
But, its use is advisable only in cases where the rashes are not large in size and their number is no more than ten pieces. Small pink peas are spread with paste overnight for 7-10 days. If after this period you have not noticed a positive result, then it is better not to torture yourself and contact a surgeon for qualified removal.
Have you decided to remove this rash?
Doctors believe that removing papules is completely unnecessary. If they do not cause concern or cause painful feelings, then there is no danger to health. Note that doctors do not pay enough attention to the presence of these pearly tumors even during medical examinations.
The decision to remove pearlescent papules is usually made by the patient himself. He explains this by the desire to get rid of this cosmetic defect. But it should be taken into account that after the operation you will need a certain number of days of sexual rest. Removal is usually performed using local anesthesia.
The decision on how to remove papules is made by a urologist or cosmetologist. There are several ways to carry out this procedure. Some of them involve the use of a laser beam. Electrocoagulation with curettage or cryotherapy with aqueous nitrogen may also be performed. They are considered more effective and allow you to get a sustainable result. After surgery, a course of special medications is usually prescribed to consolidate the effect and regulate metabolic processes.
Many patients are concerned about the question: do pearlescent papules go away?
Having appeared during the ripening period, over time they may become less visible or completely disappear.
The latter usually occurs at the age of 30-40 years. The main thing is not to confuse them with the manifestation of another disease, since, for example, anogenital warts are a bit like pearly pimples. It is also necessary to exclude the possibility of Fordyce granules and manifestations of syphilis.
Clinical picture
Pearly papules under the head do not cause any symptoms or discomfort. However, when trying to remove these papillae or when they are injured, some discomfort may occur.
If a man experiences the following symptoms - rash, discomfort, burning, itching, pain, swelling or discharge, this indicates a high probability of having a sexually transmitted disease. In this case, you should definitely consult a doctor, establish an accurate diagnosis and carry out treatment.
You suddenly have a pimple on:
And you don't know what to do? Don't panic! In our unique articles you will definitely find answers to all these and many other questions. Are you wondering if acne is hereditary or what daily habits can cause acne?
Read, comment, ask questions. Together we will find a way to get rid of acne forever!
Treatment with folk remedies
How to remove papules at home? It is almost impossible to remove them on your own. The rash rarely goes away when using folk remedies.
How to treat and reduce formations? You can try the following homemade recipes:
- Aloe juice. To cure papules, you need to use the lower fleshy leaves that are more than three years old. The cut leaf of the plant should be placed in the refrigerator for three days. Pour the crushed leaves with cold boiled water in a ratio of 1:5. The mixture should sit for about an hour, then it should be boiled and strained. The resulting decoction is used to wipe the areas with papules.
- Shilajit mixture. In a container, mix 1 g of mumiyo powder and 50 ml of honey. Dissolve the mixture in a water bath, then cool. Add 1 tsp. aloe juice The resulting product should be stored in a cool, dark place. The finished ointment should be applied for ten minutes, then the residue should be cleaned with a napkin. The affected area is lubricated with sea buckthorn oil. The therapy consists of 15 procedures.
- Medicinal calendula. 1 tbsp. l. dried flowers are poured with 500 ml of boiling water. The broth is infused for about half an hour, then cooled. The resulting infusion is used to wipe the areas affected by papules.
- Tincture of calendula and honey. Pour 1 tsp into 250 ml of warm boiled water. calendula tincture and add 1 tsp. honey The thoroughly mixed mixture is applied for half an hour.
With regular use of the described remedies, pearly papules decrease in size. But there is no guarantee of their complete disappearance. If the rash continues to appear, it is best to consult a dermatologist.
Pearlescent papules are neoplasms of a transparent or white color and small in size. Pearly papules form on the genitals. Most often men suffer from this.
To date, the exact cause of the development of the disease is not known. The formations are benign, but cause not only physical discomfort, but also psychological discomfort. The diagnosis is made based on examination by a specialist.
You cannot remove papules on your own. Representatives of the stronger sex need to regularly visit a urologist for preventive purposes.