How does ringworm infection occur?
Infection occurs only in the presence of predisposing factors:
- severely weakened immunity (chronic pathologies, recent severe infectious diseases, depression);
- HIV, cancer, AIDS;
- the presence of abrasions and other open wounds on the skin;
- other dermatological rashes on the epidermis;
- swelling of the skin as a result of frequent and prolonged exposure to a humid environment.
After the pathogen enters the skin, fungal spores begin to develop and multiply. When colonized in the hair follicle, the hair is destroyed along its entire length, followed by breakage or loss. Also, enzymes produced by the fungus have a destructive effect on the cells of the skin and nails.
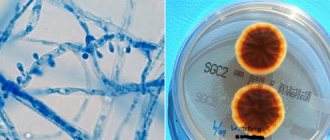
The figure shows a photo and description of the disease - ringworm in humans.
The pathogens do not penetrate into the deep layers of the epidermis and do not affect the mucous membranes.
Since fungal spores multiply more actively in a humid environment and at a temperature range of 20-30 degrees, the peak occurrence of the disease occurs in the summer. It is important that with a strong immune system, the disease does not develop, and the infected person only becomes a carrier of the infection.
Causes of development of ringworm
Ringworm in humans (the photo allows you to determine the danger of the disease) develops under the influence of the following reasons:
- personal contact with the carrier of the pathogen (human, domestic or street animal);
- general use of items used by the patient (comb, towel, bed linen);
- contact with objects of an infected animal (collar, toys, bedding);
- visiting cheap hairdressers where instruments are not disinfected;
- staying in public places, especially in swimming pools, saunas, baths. And also in schools, kindergartens and sports sections;
- neglect of water procedures, especially after visiting crowded places;
- working with soil without gloves. Fungal spores survive in open ground for up to 3 months;
- service workers (police, medical and social workers) who regularly come into contact with low social strata of people.
Infection can occur from a person without symptoms of lichen (symptoms do not appear during the incubation period, up to 15 days, and in a person with a strong immune system). Children and pregnant women are more susceptible to infection, since they do not have strong immunity, and the skin predisposes the colonization of the fungus.
Pityriasis
This disease has more than one name. It is also called sunny, colorful and multi-colored. Its appearance is caused by a yeast fungus. The development of the disease begins due to suppression of the immune system and some other factors.
Among the causes of sun lichen, excessive sweating of the skin is also noted. That is why washing in this case is considered a preventive measure.
It is with this type of disease that it is strongly recommended to carry out water procedures regularly, but exclusively with the use of antifungal drugs. Affected areas should be treated with acidified liquid. Clothing and all linen must be disinfected.
Symptoms and signs of ringworm
Symptoms of the disease manifest themselves differently depending on the type of pathogen and the area of localization.
Signs of disease depending on the type of fungus:
| Differences | Microsporia – caused by the fungus Microsporum | Trichophytosis - caused by the fungus Trichophyton |
| Incubation period | Symptoms appear after 5-10 days. | Lasts 7-15 days. |
| Localization zones | Mainly on the scalp near the crown. | It can affect any part of the body, including the nail plates. |
| Forms of rash | The diameter of the spot reaches up to 5 cm. | The spots can occupy an area up to 10 cm in diameter. |
| Characteristics of the spot | The affected skin is white due to severe peeling. An inflammatory process gradually develops with swelling and redness of the damaged area. There are small red spots along the edges of the spot. | The infected epidermis has a gray-pink color and peeling is present. It is possible to develop papules (elevation of the affected skin area above the main one) containing pus. |
| Hair condition | The hair becomes severely damaged and breaks. Root loss does not occur. | The hair breaks near the base and cannot grow back through the damaged area of skin due to the presence of a crust formation. |
| Therapy | The disease may subside on its own, without drug treatment. | Difficult to treat. Without the use of medications, a transition to a severe or chronic form with baldness of the affected area of the skin is possible. |
Itching and burning at the location of the spots is characteristic of both types of pathogens.
Also, the signs of the disease depend on the form of its course:
- superficial. The fungus can affect the skin on the head and the entire body. The nail plates are not affected. This form can go away on its own or become chronic without proper treatment;
- deep. The follicles are damaged, so this form is more typical for the scalp. It is possible that suppuration may develop in the area where the fungus is located. Difficult, but treatable;
- chronic. Observed predominantly in females, the fungus affects the smooth and hairy skin and nail plates. Treatment with hormonal drugs may be required.
The difference in symptoms depends on the location of the fungus.
Ringworm on the head and face
On the scalp, ringworm can appear in all 3 forms.
| Form of lichen | Description of features |
| Superficial |
|
| Deep |
|
| Chronic |
|
In men, the fungus can affect the beard area, sideburns and mustache.
Ringworm on the body
On the body, ringworm appears in only 2 forms.
| Form of lichen | Description of features |
| Superficial |
|
| Chronic |
|
With a long course of the disease, scar formation on the epidermis is possible.
Ringworm on nails
On the nail plates, lichen is expressed mainly in a chronic form.
Characteristic signs of pathology are:
- the nail becomes cloudy and acquires a grayish tint;
- the nail tissue becomes fragile and may thicken or thin;
- peculiar grooves are marked on the nail plate;
- the skin near the nail is inflamed and hangnails form.
In advanced forms, the nail may detach from the skin. The pathology is difficult to treat.
Stages of disease development
Ringworm in humans (the photo shows the effect of the fungus on different areas of the skin) goes through 4 stages of development:
- Incubation period. Fungal spores enter and are gradually activated without reproducing. There are no symptoms at this stage.
- Beginning of symptoms. As a result of the start of the pathogen’s multiplication, an inflammatory process begins to appear on the skin, accompanied by redness of the affected area and swelling. Next, round or oval spots from pink to red are formed, which protrude above the main layer of the epidermis. A clear, convex edge gradually forms on the affected area. Hair on the scalp breaks and falls off. The roots where the hair fell off are covered with a white-gray coating. The spots gradually spread throughout the body. Itching and burning appear.
- Peak of the disease. The spots grow in size, the edges acquire a color from burgundy to lilac. Inside the lesion, the skin peels off and has a gray-yellow tint. Secondary circles may appear inside the spots. And also, due to infection, purulent papules may form. There is an increase in temperature and enlargement of lymph nodes. The itching and burning become unbearable. The affected area is painful to the touch.
- Recovery. The spots stop spreading across the skin. Purulent formations are opened with the subsequent formation of crusts in their place. The swelling goes down. After removal of the cortical formations, the skin gradually returns to normal. The itching goes away after the crusts are removed.
Depending on the treatment, the peak of the disease can last up to several months and gradually become chronic. Medications and folk remedies are allowed to be used after examination and identification of the type of pathogen. Self-medication is dangerous due to the development of complications.
Diagnosis of the disease
Diagnosis of ringworm is made by a dermatologist. The examination process consists of the following stages.
Collection of verbal data about the patient and symptoms:
- how long have the rashes been noted on the body;
- to identify the possible source of the pathogen, the places visited 7 days before the onset of symptoms or with whom there were contacts are specified (data is important for children's, school and sports institutions, to prevent the further development of the influx of infected people);
- presence of pets;
- the state of the immune system is determined (whether there have been any recent infectious diseases or long-term use of antibiotics, as well as the presence of chronic pathologies);
- What symptoms are present other than rash and hair loss?
Patient examination:
- determination of the spot localization zone;
- identifying the presence of peeling and suppuration.
- Scraping the upper layer of the epidermis to identify the type of pathogen.
- Damaged hair follicles may need to be examined.
- Taking tests to determine the general condition of the patient.
- Illumination of the affected skin with a Voodoo fluorescent lamp. In the presence of lichen, the illuminated area acquires a green tint (with the pathogen Microsporum) and a bluish tint (with the pathogen Trichophyton).
During the examination, it is necessary to distinguish lichen from similar skin pathologies, including baldness (if the scalp is affected).
girdling
The cause of shingles is the herpes virus, which also causes diseases such as chicken pox. Until recently, doctors were categorical about washing in case of this disease. It was generally accepted that when such a procedure was carried out, the infection spread and rashes appeared on other parts of the epithelium.
At the moment, doctors have a slightly different opinion about whether it is possible to swim with lichen. Most of them allow the implementation of water procedures, but a number of restrictions are taken into account:
- swimming is allowed only if the body temperature is normal;
- Swimming in the bath is not allowed; you can wet the affected areas only with the help of a shower, and then only for a short time;
- the use of ordinary gels and soaps is allowed;
- It is strictly forbidden to rub the affected areas with a washcloth or towel;
- you cannot visit public baths, saunas and swimming pools;
It is recommended to use gels and liquid soaps as an alternative to regular soap. When carrying out water procedures, you must be as careful as possible so that the blisters of the rash are not damaged, as this may lead to re-infection.
Hygiene measures when in contact with a sick person
Ringworm can be treated with medication. With timely diagnosis of the pathology and compliance with the specialist’s prescriptions, the disease is cured without the development of complications. Confirmation is provided by photographs taken after a person has been rid of the fungus. It is important not only to follow the rules of treatment, but also hygiene and prevention measures against this pathology.
Hygiene measures in the treatment of ringworm
If there is an infected animal or relative in the house, the following safety measures must be observed:
- avoid contact with an infected person. It is advisable to allocate a separate room for the patient;
- regular hand washing with laundry or tar soap;
- When washing your body, use soft sponges, as hard ones can injure the skin. You can also use tar or laundry soap as a detergent;
- after taking water procedures, wipe the body dry, as the fungus loves a moist environment;
- To prevent the development of fungus on the scalp, use antifungal shampoos;
- Wash the patient’s underwear and bed linen separately from the main linen using disinfectants;
- personal hygiene items and furniture should be treated with special compounds that kill the fungus and its spores;
- If possible, remove carpets and other soft things from the patient’s room;
- wash pets with antifungal shampoos, even if the carrier of the pathogen is a person;
- take medications that strengthen the immune system, since with a strong immune system, spores cannot reproduce.
To exclude the development of the disease, be examined by a dermatologist after 10-15 days, even if there are no symptoms. It is especially important in childhood, since the skin is sensitive to any infections. Timely diagnosis and treatment will prevent the disease from becoming severe.
Personal hygiene of a patient with ringworm
Rules of patient hygiene to speed up the healing process and prevent the spread of fungus to healthy areas of the skin:
- if the scalp is affected by a fungus, the patient should wear a cap or scarf made of natural fabrics to prevent the spread of spores with falling out hair and flaky skin;
- wear underwear also made from natural fabrics to prevent the development of allergies and increased itching from synthetics;
- change bed and underwear daily;
- water procedures should be carried out daily using special detergents;
- When washing, do not use sponges, as they can spread spores to healthy areas of the skin;
- if there are open or festering wounds, cover them with oilcloth while taking a shower;
- Cosmetic procedures are prohibited during the period of illness, as they can provoke a deterioration of the condition;
- creams, gels and shampoos that have come into contact with the infected area must be destroyed, as they may contain fungal spores;
- cut your nails as short as possible. If there is severe itching, try not to scratch the damaged area, as the pathogen may spread to healthy areas of the epidermis.
During the period of illness, do not visit crowded places and do not have contact with pets, as they can spread the infection throughout the apartment and to relatives.
Prevention of microsporia
- Children with microsporia should not attend schools and kindergartens until they have fully recovered.
- It is necessary to follow sanitary and hygienic rules, that is, use only individual hats, clothing, have a separate bed, towel, comb, washcloth and other personal items.
- Children should not be allowed to interact with stray animals. Kittens or puppies adopted into the home should be shown to a veterinarian. Don't let children take pets to bed.
- In case of contact with a sick animal, you must wash your hands with soap, lubricate scratches and abrasions with 5% iodine, change clothes, boil the removed items or iron them with a hot iron.
- Wash domestic cats and dogs with soap and water as needed, keep them free of fleas, and be sure to show them to a veterinarian at least once a year.
- If flaky spots or lesions appear on the skin or head, you should immediately contact a dermatologist.
Treatment of ringworm
Drugs to eliminate the fungus that causes lichen are prescribed by a dermatologist or sometimes by an infectious disease specialist. The type of drug (external or internal use), as well as the name, are determined individually by a specialist after a full examination. Oral medications are prescribed for chronic or severe forms of the disease.
Ointments for ringworm
Ointments have advantages over other medications in ease of use, long-lasting action and high efficiency, and also have a minimal list of side effects.
List of recommended ointments:
| Names of drugs | Age restrictions | Terms of use |
| Ciclopirox | After 10 years | Apply 2 times a day for 7-14 days. Can be used for preventive purposes |
| Mycospor | Use under medical supervision is allowed for up to a year | Apply once a day for 14 to 28 days |
| Lamisil | After 12 years | use 1-2 times a day for 7-14 days |
| Sulfuric | After 3 years | Apply 2-3 times a day for 5 days |
| Clotrimazole | No restrictions | Use 1-3 times a day for 7-21 days |
| Bifonazole | Use in children is not recommended | Apply 2-3 times a day for 2-3 weeks. Long-term treatment up to 4 months is allowed |
| Mycozolon | Apply 2-3 times a day for 2-5 weeks | |
| Sulfur-tar | Use with caution in children | Use 1-2 times a day for 5 days |
It is recommended to use the ointments in the evening (the skin must first be cleansed with furatsilin), and in the morning the affected area must be disinfected with iodine.
Gels against ringworm
Ringworm in humans (the photo allows you to independently determine the presence of pathology, but treatment can only be prescribed by a dermatologist after examination) can be eliminated using gels. They are quickly absorbed (therefore they do not stain underwear and bedding) and have a high concentration of antifungal components.
List of gels prescribed for ringworm:
| Names of drugs | Age restrictions | Terms of use |
| Exifin | After 12 years | Use 1-2 times a day for 14 days |
| Mycogel | Apply 2 times a day for 7-21 days |
Before applying the gel, it is necessary to treat the skin with iodine.
Solutions for the treatment of ringworm
Solutions are convenient for eliminating pathogens in the scalp, and are also used to treat the epidermis before applying ointment or gel.
List of recommended solutions:
| Names of drugs | Age restrictions | Terms of use |
| Vocadine (iodine) | Use in children is permitted under the supervision of a specialist. | Used 1-2 times a day for 7-14 days |
| Yoddicerin | Apply to the skin 2-3 times during the day for 3-5 days | |
| Nitrofungin | Has no restrictions | Use 2-3 times a day until the pathology is eliminated. Allowed to be used for preventive purposes |
| Fukortsin |
The drugs can independently destroy the fungus, only if the pathology is in the initial stage or in a mild form.
Tablets for the treatment of ringworm
Used only after prescription by a dermatologist and infectious disease specialist. Additionally, consultation with a therapist/pediatrician is required to check for hidden contraindications.
List of oral medications:
| Names of drugs | Age restrictions | Terms of use |
| Griseofulvin | Have no restrictions | The dosage and course are selected according to the weight and general condition of the patient |
| Orungal | Take ½-2 capsules for 7-14 days | |
| Lamisil | After 2 years | The course of treatment is from 2 to 12 weeks. Dosage is prescribed individually |
| Terbizil | After 3 years | The course and dosage are prescribed after examining the patient |
| Exiter | Have no restrictions | |
| Terbinafine | After 3 years | |
| Ketoconazole | ||
| Fluconazole | After 5 years |
Tablets are used in complex treatment with external agents. Individual selection of dosage and course is required.
Diet for ringworm
The causative agent of ringworm cannot develop in the presence of a strong immune system (the body copes with the fungus on its own), so specialists immediately prescribe a diet to strengthen the immune system.
The menu should be dominated by vitamins. Also, food should not cause digestive upset and should be easily digestible. Additionally, you need to avoid allergenic foods.
How to treat ringworm on the head?
Ringworm in humans (photos before and after using medications allows you to verify the effectiveness of therapy) most often affects the scalp. To eliminate the pathogen, experts recommend using antifungal shampoos and oral agents.
List of funds:
| Names of drugs | Age restrictions | Terms of use |
| Sebozol | Use with caution in children | Course up to 4 weeks. Use 2-3 times a week |
| Nizoral | Has no restrictions | |
| Dermazol | Use daily for 5 days, no more than 14 days | |
| Mycozoral | Use once a day for 3-5 days | |
| Cynovitis | After a year | Course 4 weeks. Use 2-3 times within 7 days |
| Sulsena | Has no restrictions | Allowed daily use until the disease is eliminated |
Shampoos are also recommended for use as a preventive measure in the presence of fungus on the body.
ethnoscience
The use of folk remedies is recommended for preventive purposes. When used simultaneously with medications, consultation with a treating specialist is required.
List of tested recipes:
- treat the affected area of skin with propolis tincture (sold in a pharmacy) 4 times a day for up to 12 days;
- Infuse 15 g of chamomile inflorescences in 200 ml of boiling water for 30 minutes. use daily. Can be applied to the scalp. Leave for 60 minutes;
- Rub prepared apple cider vinegar into the skin 6 times a day until the rash disappears;
- use a compress of freshly squeezed cranberry juice as a compress 3 times a day;
- Apply garlic juice to the skin. Use carefully, as it can cause burns to the epidermis;
- Apply a cabbage leaf to the affected area and spread sour cream on top. Leave the bandage on for 1 hour.
Before using the products, it is necessary to cleanse the skin.
Folk recipes
In past centuries, people knew well how to cure lichen without the use of drugs. Few of the secrets have survived to this day.
To reduce the inflammatory reaction, it will be useful to make compression lotions from pumpkin pulp. It must be squeezed through a gauze or bandage and applied to the affected areas morning, afternoon and evening. After a day, the symptoms should subside.
A compress with the addition of mashed boiled beets, honey or cranberry juice can help a lot.
To restore pigmentation and restore skin, a decoction of chamomile flowers can help. A warm decoction is applied to the head with a cotton swab, and then washed off an hour later.
There is also a positive trend in the use of raw chicken eggs, from which we only need a film that has many nutrients. It must be smeared on sore spots in the morning, afternoon, and evening for 7 days.
Using these recipes in combination with basic medications gives excellent results.
Consequences of ringworm
If ringworm is quickly detected and all the specialist’s prescriptions are followed, the disease is completely cured, without the development of complications. In its advanced form, the disease can become chronic with the formation of scars, bald spots and possible infection in open wounds.
Ringworm does not develop in people with strong immune systems , so dermatologists recommend supporting immunity by taking vitamins and eating healthy foods.
The disease can be transmitted from an infected person or animal, which requires daily inspection of pets visiting the street. Numerous photographs allow you to assess the severity of the disease.
Author: Kotlyachkova Svetlana
Which doctor should I contact?
If an adult or child has symptoms of ringworm, you should immediately consult a doctor. This could be a dermatologist or infectious disease specialist.
The doctor, using the diagnostic methods available to him, will confirm or deny the fact of infection and prescribe the appropriate treatment. It is worth remembering that without treatment, ringworm can provoke very unpleasant consequences in the form of baldness or suppuration, and can also be spread to other people.
In addition, there is a possibility that the symptoms of ringworm hide diseases such as atopic dermatitis, psoriasis, lichen planus, alopecia areata, etc.