Palmoplantar psoriasis affects the palms of the hands and soles of the feet, and the disease itself is a pathological autoimmune condition.
According to the Center for Disease Control and Prevention, about 3.1 percent of the Russian population aged 20 to 59 have some form of this pathology. According to WHO estimates, the prevalence of psoriasis in some countries of the world has reached 11.4% and is currently regarded as a “serious global threat.”
Psoriasis on the palms and soles, along with localization of the process on the scalp, is considered one of the most common forms of the disease. It accounts for about 14% of cases of pathological skin conditions.
Reasons for the development of the disease
Although the palmoplantar form of psoriasis is not age-related, the highest incidence of the disease is observed between 15 and 35 years. There is also a connection with ethnicity. It is reported that people of Caucasian nationality over the age of 50 years have a significantly increased risk of developing this pathology.
The exact causes of the pathological condition are not fully understood and it is still believed that the disease is based on an autoimmune process. During normal functioning of the immune system, a person receives protection from a variety of foreign agents: viruses, allergens, protozoa and other microorganisms.
With psoriasis, a certain malfunction occurs in the body, after which the immune system begins to produce aggressive substances against its own cells and tissues. An excessive number of T-lymphocytes (the main immune cells) and macrophages leads to the development of an inflammatory reaction and excessive proliferation of skin cells, which is why characteristic symptoms and the appearance of hyperkeratosis are observed.
Note! Hyperkeratosis is excessive thickening of the epidermis, the outer layer of the skin.
Some studies indicate a small role for heredity. For example, about 10% of the population inherits genes associated with psoriasis and only 3% of them develop the disease. Such statistics suggest the presence of other, more fundamental causes of the disease.
What is psoriasis
Psoriasis is a disease that primarily affects the skin.
Recently, the autoimmune nature of the pathology has been assumed. Psoriasis is classified as a non-infectious disease that is inherited. If the mother has a pathology, the risk of its development in the child increases by 25%, but if both parents are sick, the probability of developing lichen planus in the child is 50%. Symptoms of the disease include the appearance of red rashes of varying sizes on the body. In medical practice, these spots are called plaques or papules.
In most cases, the rash is accompanied by severe itching and peeling. When you try to scrape off the scales, their number increases.
Peeling is not typical for all types of disease. With a drop-shaped form, they may have a weak character or be completely absent.
Pustular psoriasis is accompanied by the appearance on the body of pustules filled with sterile liquid. In this case, the patient complains of severe itching and burning, especially at night.
The most common form of the disease is vulgar or ordinary psoriasis. The pathology often occurs in a mild form, accompanied by the appearance of rounded plaques on the body, localized on various parts of the body.
Common forms of the disease include psoriasis of the scalp, palmar-plantar, knee-elbow and other types of psoriasis.
Diagnosis of palmoplantar psoriasis
Despite the rapid development of modern medicine, the diagnosis of psoriasis on the palms is still possible through a visual examination by a skin doctor without special equipment. The physical examination is based on the “psoriatic triad,” the manifestations of which are observed when scales are easily scraped off from the affected areas of the body.
The doctor pays attention to the history of the disease, since some constantly taken medications can be triggers for the development of the disease:
- Indomethacin and other non-steroidal anti-inflammatory drugs (NSAIDs);
- Lithium and antimalarials;
- Abrupt withdrawal of glucocorticosteroids;
- Taking penicillin, hydroxychloroquine.
In difficult cases, a comprehensive examination is recommended, which includes a laboratory blood test and ultrasound scanning, as well as excluding fungal infections using mycological diagnostics. When indicated, a biopsy of a questionable lesion of the skin is performed.
Symptoms and first signs of palmoplantar psoriasis
Among the main types of the disease, there are five variations. Moreover, in 90% of cases a characteristic visual clinical picture is observed.
What does palmoplantar psoriasis look like? The patient has psoriatic plaques on the palms and soles - red, scaly patches on thickened skin that are prone to peeling. In the lesions, a person feels itching, heat and pain of varying intensity; in some cases, the skin cracks and bleeds.
It also influences the formation of nails:
- Defects and holes may appear in the nail plates;
- The nail thickens and becomes discolored;
- Its shape changes.
The palmoplantar type of the disease occurs as part of the general process, but is limited only to the skin of the palms and feet. Psoriasis of the soles makes walking and wearing shoes difficult. Damage to the hands can not only interfere with the performance of any work, but also leave a negative imprint on relationships with people. Ordinary situations, such as shaking hands, can be awkward, leading to embarrassment and social anxiety in a person, even to the development of social phobia.
A distinctive feature of the palmoplantar form of the disease is the presence of varieties of the process, which can be called by the following terms:
- Barber palmoplantar pustular psoriasis;
- Palmoplantar pustular psoriasis;
- Pustular dermatitis.
Treatment of psoriasis with traditional methods
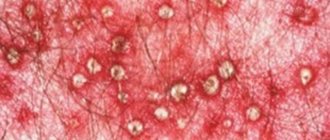
Pustular psoriasis
The listed skin disorder causes the formation of clusters (accumulations) of whitish pustules in the area of plaques. In general, this rash is very similar to regular acne. It is worth noting that this type of disease is quite resistant to light treatment methods and often requires an integrated approach to the therapy.
Note! Pustular psoriasis of the palms and soles requires treatment with antibacterial drugs when a bacterial infection is associated.
Folk remedies
To speed up the healing process, experts recommend combining drug therapy with alternative methods. Numerous reviews indicate that infusions and decoctions have the best effect. Most often, treatment of palmoplantar psoriasis with folk remedies includes the following recipes:
- Two teaspoons of elderberry flowers and leaves are poured into 500 ml of boiling water. The product is allowed to brew for 40 minutes, after which it is necessary to filter. You need to drink 1/3 glass after each meal.
- You need to take 25 grams of bay leaves and pour 450 ml of boiling water over them. The infusion is boiled in a tightly closed saucepan over low heat for thirty minutes. The finished product is filtered through cheesecloth and taken orally half a glass 3-4 times a day. The duration of treatment is 8-10 days.
- Experts recommend taking sea buckthorn oil orally, one teaspoon once a day. In addition, this natural remedy can be gently lubricated on the affected areas on the palms and soles.
- To treat damaged skin, you can independently prepare a high-quality ointment from the following ingredients: spring adonis, celandine powder, tar, petroleum jelly (ratio 25:25:50:200 grams). All components are carefully mixed in one container, after which the product is ready for use.
- A positive effect can be achieved by applying fish oil to psoriasis plaques.
It is worth considering that patients with this disease, in addition to constant pain and discomfort, also experience psychological problems. Along with medication and alternative treatment, they may need the help of a psychotherapist. Only an integrated approach to solving the problem allows you to achieve good results.
It is impossible to completely get rid of DIBI. This chronic pathology will manifest itself periodically throughout life, but modern treatment methods make it possible to achieve stable remission. For high-quality prevention of relapse of the disease, it is imperative to follow all the instructions of the attending physician, as well as avoid unfavorable factors that can provoke an exacerbation.
Stages of palmoplantar psoriasis
As with all forms of the pathological process, palmoplantar localization is characterized by three clinical stages:
- First stage. The appearance of rashes on the arms and legs. The plaques have a characteristic red tint; whitish purulent inclusions may be observed; The patient is bothered by intense itching. Elements of the rash merge into large lesions. Their number depends on the individual characteristics of the disease.
- Stabilization stage. The condition does not progress, new pathological elements are not formed, but the old ones are still preserved. The itching gradually subsides, and the color of the plaques becomes less bright.
- The final stage. Accompanied by regression of elements, there is no itching. Treatment becomes supportive or is eliminated altogether; Recommendations are offered for maintaining remission and preventing relapses.
In some cases, the disease is classified according to the elements of the rash:
- The usual form is a typical appearance on the skin;
- The horny form is accompanied by hyperkeratosis, and there are few or no typical red spots;
- Vesicular-pustular form (Barbera).
Manifestation of different forms of psoriasis
At the initial stage, all types of pathology manifest themselves as scaly rashes that affect the palms and soles. Plaques not only itch, but also become inflamed. In the absence of quality treatment, a secondary infection may occur, which only aggravates the situation. Specific manifestations on the surface of the epidermis depend on the type of DILI:
- Calloused form. The pathology develops against the background of progression of hyperkeratotic coarsening (rapid growth of the stratum corneum of the skin). Against this background, hardening of the skin is noted, leading to the formation of specific calluses. Initially, they are located chaotically, but then merge into a single plaque. If the patient does not go to the hospital, calluses will continue to affect the lateral surfaces of the palms and feet. But even in such a difficult situation, you can see the border between healthy skin and modified skin.
- Round form. Tiny scaly plaques form on the patient's hands, which can even affect the outside of the hands. The disease is quite severe, as the patient experiences constant itching, redness, swelling and tightness of the skin. Gradually, the plaques begin to peel off, and the epithelium peels off in large fragments. Against this background, a person can no longer move freely and do his favorite things.
- Plaque-fan-shaped form. This is the most common type of psoriasis, accompanied by classic symptoms. Light gray plaques form on the back of the hands, which gradually take on an oval shape. Without treatment, the affected skin becomes covered with small cracks through which blood leaks.
- Pustular form. At the initial stage, thin skin turns red, after which vesicles and pustular pimples appear on it. After some time, they dry out and turn into dense crusts. In a short period of time, pustules can affect a huge area of the epithelium. This form of the disease is characterized by symmetry.
Treatment methods
Palmoplantar psoriasis is a chronic disease that can recur, regardless of treatment. However, there are treatment methods that can reduce the duration of exacerbation and prolong the period of remission.
The main method of treatment is an attempt to prevent the rapid growth of cellular elements that lead to the development of plaques; anti-inflammatory therapy is carried out. An alternative technique offers direct removal of scales.
Since the skin on the palms and soles is thickened even in healthy people, treatment of this localization often involves a combination of techniques and a more aggressive effect on the lesions.
First of all, for psoriasis of the palms and soles, local treatment is prescribed in the form of gels, ointments and creams:
- Vitamin D analogues (representative - Daivonex);
- Ointments based on corticosteroids (hydrocortisone);
- Retinoids;
- Anthralin;
- Coal tars;
- Salicylic acid;
- Moisturizers to reduce swelling and relieve inflammation.
Common side effects include irritation, drying and thinning of the skin. Additionally, phototherapy sessions can be performed:
- Natural ultraviolet radiation from the sun;
- Artificial ultraviolet radiation using special devices;
- Excimer laser;
- Photochemotherapy.
Important to know! A smooth transition to natural phototherapy is very important. It is recommended to start with 5-10 minutes of direct sunlight per day. Subsequently, you can gradually increase the exposure time by 30 seconds per day.
Course of the disease and prevention
The severe course of the disease to a certain extent can influence the development of serious conditions that threaten the health and life of the patient: the risk of myocardial infarction increases by 58% and stroke by 43%. The main immediate complications of psoriasis of the palms and soles are psoriatic arthritis and nail dystrophy.
The photo shows an example of psoriatic arthritis
The National Medical Research Center of Russia has named a number of diseases that may depend on skin pathology:
- Associated autoimmune conditions: Crohn's disease, celiac disease, sarcoidosis and others;
- Eye diseases: cataracts and glaucoma, as well as infectious processes;
- High blood pressure;
- Parkinson's disease;
- Diabetes;
- Liver and kidney diseases;
- Osteoporosis;
- Depression.
Note: With timely treatment and following the necessary recommendations, possible relapses of psoriasis can be reduced and skin manifestations can be minimized.
Recommended preventive measures:
- Take daily baths with natural oils, salts and mild soaps that do not contain artificial fragrances or colors;
- Use a skin moisturizer (in severe cases - twice a day), especially after taking water procedures. The use of hard towels is not allowed. Simply apply a soft, dry cloth to your skin and then use the cream;
- Get enough sunlight. It is necessary to consult a doctor and choose the “golden mean”. Too little insolation will not bring a noticeable effect, and too intense will increase the risk of developing skin cancer;
- Avoid triggers such as smoking, drinking, stress and infections;
- Use aloe juice. It is necessary to apply lotions to damaged areas of the skin several times a day. There are official studies proving the effectiveness of this plant in combating inflammatory skin processes;
- Get at least three grams of omega-3 fatty acids per day. Include fish, walnuts, flaxseed oil in your diet, or take fish oil capsules. Fatty acids help reduce inflammation in the body;
- Taking some special supplements based on barberry, tea tree oil or Dead Sea salt helps.
Diets
An important component of effective treatment or prevention of psoriasis is a therapeutic diet. Many doctors consider it the basis and guarantee of a speedy recovery.
Basic nutritional recommendations:
- exclude smoked meats, pickles, fried and spicy foods from the diet;
- do not consume foods considered allergenic (citrus fruits, chocolate, tomatoes);
- limit consumption of corn and potatoes;
- do not eat pork and lamb, since these types of meat contain fatty acids that are difficult to digest;
- include fiber in your daily menu; there is a lot of it in fresh herbs, fruits and vegetables;
- increase consumption of lactic acid products;
- Make buckwheat, oatmeal and wheat porridge the basis of your diet.