Relevance of the problem
In the last decade, this type of hypersensitivity in children under 12 months of age has acquired new features:
- very early appearance;
- high prevalence;
- combined manifestations of allergies with symptoms from the digestive tract.
Cow's milk protein antigens are considered the strongest allergens. Milk contains more than 40 allergens.
The most dangerous are:
- caseins;
- bovine serum albumin;
- beta-lactoglobulin;
- alpha-lactalbumin.
Risk factors for food hypersensitivity to cow's milk proteins:
- hereditary predisposition;
- artificial feeding;
- consumption of large amounts of dairy products by a nursing mother;
- diseases of the gastrointestinal system in newborns;
- early introduction of complementary foods including dairy products.
How to determine that this is a reaction to milk?
The doctor necessarily conducts a visual examination, pays attention to the condition of the skin, and is interested in the general condition of the patient.
The more detailed the patient describes the clinical picture of the disease, the more likely the doctor will be able to help.
Do not try to diagnose yourself, your loved ones, especially your children.
Remember, only a certified pediatrician can correctly diagnose a child. Parents do not need to self-medicate and give their child all kinds of medications.
The digestive system of an infant is not formed, and there is a risk of further harming the baby’s health.
To properly diagnose the disease it is necessary:
- Get tested for lactose intolerance . Manifestations of lactase deficiency are easily confused with an allergy to cow's milk protein;
- Pass medical tests.
Testing for lactose intolerance
The test for lactase deficiency itself involves adhering to a lactose-free diet (if the baby has symptoms, the mother follows the diet).
Lactose is a component of all dairy products, including milk, butter, cheese and cream.
Present in all dairy derivatives:
- ice cream;
- kefir;
- yogurt;
- condensed milk;
- sour cream;
- acidophilus milk;
- hot cocoa.
If after several days the symptoms of the disease disappear, we can definitely say that the cause is lactase deficiency.
If it is an allergy to protein, then for recovery it is necessary that the contact of the allergen with the body stops completely, and this is a long process and, as a rule, it does not go away in a few days.
Analyzes
If the symptoms remain, then a set of tests is carried out to identify the allergen, including:
- General urine analysis . The protein level should be increased, and red blood cells may be present in the urine;
- Blood test (general and biochemical);
If allergic reactions occur in the body, then there should be many immune complexes in the blood:
- Determination of the amount of immunoglobulins IgE, IgG;
- Determination of the degree of sensitization of the body to milk proteins.
Scarification tests
In addition to laboratory tests, the use of skin prick tests .
During the procedure, shallow scratches 0.5–1.0 cm long are made on the skin of the forearm or back, onto which one drop of a different allergen is applied.
Next to each scratch, a brief designation of the allergen that was applied is written with a pen.
In the case of an allergy to milk, various proteins, fats and carbohydrates included in its composition are used separately as allergens.
After a certain time, an inflammatory shaft forms around one or several scratches, larger in size than around the other scratches. This means that the body exhibits an allergic reaction to this component of milk.
How is an allergy to cow protein characterized in an infant?
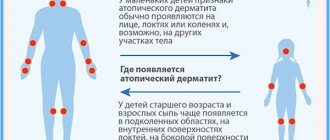
Symptoms in the form of a skin rash - atopic dermatitis - are typical for very young children. Most often, at the age of 2 - 3 months, mothers may notice redness in the baby’s cheeks. Redness may either disappear or intensify.
Subsequently, bubbles appear at the site of the rash, which burst, and a weeping surface is formed, covered with crusts. The baby is very bothered by itching. In advanced forms of allergies, the rash can cover the child’s entire body.
In some special cases, allergic immune reactions to milk in a child may manifest as hives - the appearance of itchy blisters on the body. Against the background of urticaria, allergic swelling of the face, eyelids, and lips may appear.
Do not forget that in children allergic processes can imitate pathologies of the gastrointestinal system. Such manifestations complement the skin symptoms. Gastrointestinal manifestations include vomiting, intestinal colic, loose stool, and increased gas formation.
In children in the first month of life, the process of allergic inflammation in the tissues of the esophagus can be accompanied by severe pain and refusal of breast milk, reminiscent of the picture of pyloric spasm.
Milk protein allergy in adults
Adults are not as susceptible to milk allergy as children, but it is more difficult to diagnose because it presents with a variety of symptoms, and if the allergen is not known in advance, the allergy can be easily confused with other ailments.
The appearance and severity of symptoms in adults depends on several factors:
- Degree of sensitivity to milk protein;
- The amount of allergen entering the body;
- The body's ability to resist an allergen;
- General state of human health.
There are 3 stages of development of an allergic reaction:
- Immune;
- Biochemical;
- Clinical.
Let's look at these stages in a little more detail.
Immune stage
The first contact of the immune system antibodies and the allergen occurs. Antibodies try to cope with foreign substances, as a result of which sensitization of the body occurs, that is, the body becomes hypersensitive to the action of the allergen.
The essence of sensitization is to prepare internal organs for the negative effects of foreign substances on them.
Biochemical stage
Reactions caused by the presence of foreign particles begin to take place in the body. This stage develops when the second contact of the allergen with antibodies occurs. In the area where contact occurred, lymphocytes and antibodies accumulate, and together they try to isolate the antigens.
During this, substances such as histamine and serotonin are formed in the body. They provoke the initial signs of allergies (skin rashes, fever, inflammatory processes).
Clinical stage
A reaction begins from the body tissues. The degree of reaction is influenced by the amount of allergen, the body’s ability to fight it and the general state of a person’s health.
Clinical reactions can occur either instantly or with a delay of up to several days.
Symptoms of manifestation
Symptoms of milk protein allergy in adults:
Stomach ache;- The appearance of heartburn due to increased acidity;
- Vomiting;
- Diarrhea;
- Skin lesions, rashes, itching;
- Anaphylactic reactions;
- Nasal congestion;
- Breathing problems;
- Ear congestion;
- Cardiopalmus;
- Dizziness;
- Quincke's edema (develops immediately after contact with milk; can be fatal, so if such symptoms occur, you should immediately call an ambulance).
Why do allergies to cow's milk antigens occur?
These processes are associated with a decrease in the protective functions of the immune system to food allergens.
Even in the prenatal period, the type of response of the immune system is laid down. In the presence of hereditary prerequisites, the Th-2 type of immune reaction is formed.
Allergens can penetrate the placenta and also enter the fetus through amniotic fluid.
In children, due to physiological characteristics, there is immaturity of the digestive tract. An increased antigenic load on the intestinal wall can trigger the formation of an allergic reaction.
Specific immunoglobulins E from the mother, starting from the 20th week of pregnancy, are able to penetrate the placenta.
Treatment
The main method of treating food hypersensitivity is diet therapy.
If a small patient is breastfed, mothers are prescribed a special diet excluding dairy products. Mothers are also advised to avoid foods with a high allergenic potential - chocolate, coffee, spices, mushrooms, nuts, strawberries, sausages, canned food. Pasta, gluten-containing cereals and sugar are limited.
Children receiving formula milk are prescribed medicinal hydrolysate formulas.
What to do if your baby is allergic to milk?
In this case, you need to adhere to several rules:
- The mother needs to adhere to a hypoallergenic diet and breastfeed the baby for as long as possible, because mother’s milk contains everything necessary for the normal development of the baby;
- It is necessary to exclude dairy products and products that may contain milk proteins in one form or another (ice cream, baked goods, etc.): when the allergy is mild, the mother can consume fermented milk products in small quantities: kefir, fermented baked milk, sour cream;
- when the allergy is severe, the mother will have to completely give up not only milk, but most likely also foods such as eggs and fish;
- completely eliminate “milk” - if the allergy is pronounced;
What to do if an artificial baby is allergic to milk?
Many complementary feeding mixtures contain milk protein. If a child is allergic to it, then it is necessary to switch to mixtures of hydroisolated proteins or amino acids.
There is an option to use a mixture based on goat's milk, but here you need to be very careful in order to diagnose allergy symptoms in time if they appear. There are also soy mixtures on the market; they are allowed only after six months and provided that the child is not allergic to soy.
What are hydrolysate mixtures?
Highly hydrolytic mixtures are obtained by enzymatic breakdown of the substrate - whey or casein - into peptides. Peptides have a low molecular weight, which means that by hydrolysis it is possible to reduce the allergenicity of the mixture hundreds of times. It will be useful for parents to familiarize themselves with the classification of hydrolysate mixtures.
Classification of highly hydrolytic mixtures
Based on the substrate undergoing hydrolysis, all mixtures are divided into casein and whey.
Casein is the least allergenic and is used for severe cases of allergies. Casein mixtures include Pregemestil, Frisopep AS, and Nutramigen. Whey mixtures are more nutritious and valuable in chemical composition. These include “Alfare”, “Nutrilon Pepti Allergy”.
According to the degree of substrate breakdown, mixtures are divided into:
- highly hydrolyzed - “Alfare”, “Neocate”, “Frisopep”;
- partially hydrolyzed preventive mixtures - “NAN GA”, “Frisolak GA”.
Based on the chemical composition, mixtures are divided into lactose-free, low and high lactose. There are also mixtures containing long-chain and medium-chain triglycerides.
For severe food allergies with disruption of the digestive tract, lactose-free casein mixtures are prescribed. Medium chain triglycerides significantly increase the digestibility of fats.
Goat milk based formulas
Goat milk has a reduced content of casein and beta-lactoglobulin, and alpha-lactalbumin has a different structure. New Zealand produces Nanny and Nanny Golden Goat blends. The mixtures are well absorbed and have hypoallergenic properties.
“Amalthea” is an instant goat’s milk powder recommended for use in women during lactation and pregnancy in order to prevent allergic diseases in the baby.
Introduction of complementary foods
Complementary foods are administered as prescribed by a doctor.
Start with mono-component vegetable purees or lactose-free gluten-free cereals. From six months you can introduce canned meat puree from rabbit, horse meat, turkey, excluding beef and veal.
From 8 months of age, vegetable and cereal dishes with the addition of meat puree are introduced. You can give your baby apples, currants, cherries, yellow plums baked or in the form of compotes.
A child is not given cottage cheese, eggs or seafood until he is one year old.
Dietary prevention
For babies at risk of developing allergic reactions to cow's milk protein, hypoallergenic preventive formulas are recommended. For example, “NAS Hypoallergenic”, “Nutrilon GA”, “Hipp GA”. The mixtures are based on partially hydrolyzed peptides.
Breastfeeding is the main factor in preventing the development of food allergies, providing immunity from antigens. It is advisable to continue breastfeeding for at least six months in order to reduce the risk of allergic processes.
Nuts, peanuts, chicken eggs, milk, and seafood are excluded from a nursing mother's diet. Cow's milk is introduced after a year, chicken eggs after reaching 24 months, nuts and seafood are not recommended until 3 years of age.
Allergy to milk protein in children over one year of age
While a child is experiencing symptoms of a reaction to milk protein, pediatricians recommend completely eliminating the dangerous allergen from the child’s diet.
Cow's milk can be replaced with other products such as:
- Goat milk . The main thing is to monitor how the child’s body reacts to this product;
- Rice milk . To prepare it, you need to grind the boiled rice to a paste and strain;
- Soy milk . Made from soybeans. You need to pour water over the beans, boil them after a while, grind and strain.
Most often, food allergies go away when a child reaches the age of three, when all body systems are formed.
If an allergy occurs to a specific substance, then such an allergy has nothing to do with the immaturity of the body and will manifest itself whenever the body interacts with an allergen.
Memo to parents
Cow's milk protein antigens are considered the strongest allergens. For very young children, manifestations of food hypersensitivity to cow's milk proteins in the form of a skin rash - atopic dermatitis - are typical. What parents need to know:
- An increased antigenic load on the intestinal wall can trigger the formation of an allergic reaction.
- The main method of treating food allergies is diet therapy.
- Highly hydrolyzed mixtures are obtained by enzymatic breakdown of the substrate - whey or casein - into peptides. Peptides have a low molecular weight, and through hydrolysis it is possible to reduce the allergenicity of the mixture hundreds of times.
- Breastfeeding is the main factor in preventing the development of cow's milk allergy in infants, providing immunity from food antigens.
- For babies at high risk of developing allergic processes, hypoallergenic preventive formulas are recommended.
Allergy to milk protein in children under one year of age
For a newborn baby, everything except mother's milk, any mixture, is the roughest food. In infants, the mucous membrane of the digestive tract is loose, immature, not protected by natural microflora, and is easily accessible to allergens.
Only by the age of 2 in children do the walls of the stomach and intestines acquire the ability to resist the introduction of pathogenic agents.
Milk allergy and lactose intolerance
There are two reasons why milk intolerance occurs:
- Lactose intolerance contained in milk;
- Intolerance to milk proteins: casein, globulin, albumin.
The enzyme lactase is responsible for processing lactose; if there is a lack of lactase in the body, then the immune system immediately reacts to milk. Lactase is produced from the cells that make up the small intestine and is responsible for dissolving the sugar found in dairy products.
Lactase deficiency can be the result of inflammatory processes and infections.
A milk allergy is an allergic reaction to proteins that are present in milk, rather than to lactose. People with milk allergies can tolerate lactose as long as it is separated from the milk proteins.
During infancy, the body may react to milk due to lactose intolerance, because at this age the child mainly feeds on mother's milk.
Here is a comparative analysis of the symptoms of lactose deficiency and allergy to cow's milk protein:
| Lactose deficiency | Allergy to milk protein |
| increased gas formation, stomach pain may occur; bloating; loose stools, possibly with mucus; frequent regurgitation after eating; the child slowly gains weight, most of the substances from the mother’s milk are not absorbed into the blood; good appetite, but whims during feeding. | Undigested milk residues in the stool, possibly mixed with blood; frequent regurgitation; stomach ache; loss of appetite; colic in the intestines; possible fever. |
As you can see, the characteristic features may be similar. When they appear, you need to carefully monitor the child’s condition.
Causes of the disease
When the allergen is cow's milk protein, the body may react to one or more of the 25 proteins present in the milk.
Factors that cause a reaction to milk protein:
- Heredity . The patient’s immune system may simply not be able to produce the required number of enzymes to digest milk;
- Bad ecology;
- There were pathologies during pregnancy (premature birth, constant stress, etc.);
- Parents' lifestyle , attention to a healthy lifestyle in the family;
- Avitaminosis;
- Frequent use of immunostimulants.
Possible causes of an allergy specifically to cow's milk protein:
- Liver problems . Allergies occur due to the fact that unprocessed milk molecules enter the circulatory system;
- Pathologies with the gastrointestinal tract . Milk is processed worse in the stomach and begins to be perceived by the stomach as an antigen;
- Parasitism.
Manifestations of allergies
Allergens travel with the blood to all parts of the body, therefore, it is unknown which organs may be affected due to an allergy to cow's milk protein. The process may be aggravated by the occurrence of other diseases, such as acute respiratory viral infections, various infections, etc.
An allergy to cow protein can manifest itself as a malfunction:
- Gastrointestinal tract;
- Skin lesions;
- Respiratory system.
If problems in the gastrointestinal tract of an infant are caused by an allergy to cow's milk, then the body may react as follows:
- Loose stools , in which you can discern undigested food particles, and in special cases, streaks of blood;
- Gagging , frequent regurgitation;
- Abdominal pain (not to be confused with regular colic);
- Possible pain in the stomach (due to an increase in the level of hydrochloric acid in it);
- The child’s pancreas stops producing the necessary enzymes in the required volume, and lactase levels may decrease. The number of bifidobacteria in the intestines decreases, this creates good soil for the proliferation of harmful microorganisms (for example, E. coli, helminthic infestation).
The skin is also susceptible to milk allergies.
Symptoms:
- Rash under the knees, on the arms, on the face;
- Milk eschar (unpleasant scabs on a child's head). This mainly happens when a child is fed formula. These crusts need to be moistened with oil and carefully removed with a wooden comb.
- Eczema . It can appear throughout the body in the form of bubbles with liquid; such bubbles burst over time, and a dry crust forms in their place.
- Quincke's edema . Such swelling occurs on the mucous membranes of the body: lips, eyelids, reproductive system, larynx. In the latter case, the child requires emergency assistance; this form of edema is fatal - a swollen larynx can block the access of air to the child’s lungs.
Problems with the respiratory system are quite rare, but they are still useful to know.
The following symptoms appear:
- Rhinorrhea;
- Sneezing;
- Cough;
- Wheezing;
- The child has difficulty breathing;
- Very rarely, allergic processes lead to the development of bronchial asthma.