Epstein Barr virus (EBV) is one of the members of the family of herpes infections. Its symptoms, treatment and causes in adults and children are also similar to cytomegalovirus (herpes according to No. 6). EBV itself is called herpes number 4. In the human body, it can be stored for years in a dormant form, but when immunity decreases, it is activated, causes acute infectious mononucleosis and later - the formation of carcinomas (tumors). How else does the Epstein Barr virus manifest itself, how is it transmitted from a sick person to a healthy person, and how to treat the Epstein Barr virus?
What is: Epstein Barr virus The virus got its name in honor of the researchers - professor and virologist Michael Epstein and his graduate student Iwona Barr.
Einstein bar virus has two important differences from other herpes infections:
- It does not cause the death of host cells, but on the contrary, it initiates their division and tissue proliferation. This is how tumors (neoplasms) form. In medicine, this process is called proliferation - pathological proliferation.
- It is not stored in the ganglia of the spinal cord, but inside immune cells - in some types of lymphocytes (without their destruction).
The Epstein Barr virus is highly mutagenic. With the secondary manifestation of infection, it often does not respond to the antibodies produced earlier at the first meeting.
Manifestations of the virus: inflammation and tumors
Acute Epstein Barr disease manifests itself as flu, colds, inflammation
. Long-term, low-grade inflammation initiates chronic fatigue syndrome and tumor growth. At the same time, different continents have their own characteristics of the course of inflammation and the localization of tumor processes.
In the Chinese population, the virus more often forms nasopharyngeal cancer. For the African continent - cancer of the upper jaw, ovaries and kidneys. For residents of Europe and America, acute manifestations of infection are more typical - high temperature (up to 40º for 2-3 or 4 weeks), enlargement of the liver and spleen.
Epstein Barr virus: how is it transmitted
Epstein bar virus is the least studied herpes infection. However, it is known that the routes of its transmission are varied and extensive:
- airborne;
- contact;
- sexual;
- placental.
The source of infection through the air is people in the acute stage of the disease (those who cough, sneeze, blow their nose - that is, they deliver the virus into the surrounding space along with saliva and mucus from the nasopharynx). During the period of acute illness, the predominant method of infection is airborne droplets.
After recovery (decrease in temperature and other symptoms of ARVI), the infection is transmitted through contact (kissing, shaking hands, sharing utensils, during sex). EBV resides in the lymph and salivary glands for a long time. A person can easily transmit the virus through contact during the first 1.5 years after the disease . Over time, the likelihood of transmitting the virus decreases. However, research confirms that 30% of people have the virus in their salivary glands for the rest of their lives. In the other 70%, the body suppresses a foreign infection, while the virus is not detected in saliva or mucus, but is stored dormant in the beta lymphocytes of the blood.
If there is a virus in a person’s blood ( virus carrier
) it can be transmitted from mother to child through the placenta. In the same way, the virus is spread through blood transfusions.
What happens when infected
The Epstein-Barr virus enters the body through the mucous membranes of the nasopharynx, mouth or respiratory organs. Through the mucous layer, it descends into the lymphoid tissue, penetrates beta lymphocytes, and enters the human blood.
Note: the effect of the virus in the body is twofold. Some of the infected cells die. The other part begins to divide. At the same time, different processes predominate in the acute and chronic stages (carriage).
During acute infection, the infected cells die. In case of chronic carriage, the process of cell division with the development of tumors is initiated (however, such a reaction is possible with weakened immunity, but if the protective cells are sufficiently active, tumor growth does not occur).
The initial penetration of the virus often occurs asymptomatically. Infection with the Epstein Barr virus in children manifests visible symptoms only in 8-10% of cases
. Less commonly, signs of a general disease develop (5-15 days after infection). The presence of an acute reaction to infection indicates low immunity, as well as the presence of various factors that reduce the body's protective reactions.
Epstein Barr virus: symptoms, treatment
Acute infection by a virus or its activation with decreased immunity is difficult to distinguish from a cold, acute respiratory infection or acute respiratory viral infection . The symptoms of Epstein bar are called infectious mononucleosis. This is a general group of symptoms that accompany a number of infections. Based on their presence, it is impossible to accurately diagnose the type of disease; one can only suspect the presence of an infection.
In addition to signs of a common acute respiratory infection, symptoms of hepatitis, sore throat, and rash may be observed . The manifestations of the rash increase when the virus is treated with penicillin antibiotics (such erroneous treatment is often prescribed due to incorrect diagnosis, if instead of a diagnosis of EBV a person is diagnosed with tonsillitis or acute respiratory infections). Epstein-Barr is a viral infection in children and adults; treatment of viruses with antibiotics is ineffective and fraught with complications .
Epstein Barr infection symptoms
In the 19th century, this disease was called an unusual fever, in which the liver and lymph nodes become enlarged and the throat hurts. At the end of the 21st century, it received its own name - Epstein-Barr infectious mononucleosis or Epstein-Barr syndrome.
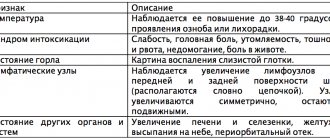
Signs of acute mononucleosis:
- Symptoms of acute respiratory infections - poor health, fever, runny nose, enlarged lymph nodes.
- Symptoms of hepatitis : enlarged liver and spleen, pain in the left hypochondrium (due to an enlarged spleen), jaundice.
- Symptoms of sore throat : soreness and redness of the throat, enlarged cervical lymph nodes.
- Signs of general intoxication : weakness, sweating, soreness in muscles and joints.
- Symptoms of inflammation of the respiratory organs : difficulty breathing, cough.
- Signs of damage to the central nervous system : headache and dizziness, depression, sleep disturbances, attention, memory.
Signs of chronic virus carriage:
- Chronic fatigue syndrome, anemia.
- Frequent relapses of various infections - bacterial, viral, fungal. Frequent respiratory infections, digestive problems, boils, rashes.
- Autoimmune diseases - rheumatoid arthritis (joint pain), lupus erythematosus (redness and rashes on the skin), Sjögren's syndrome (inflammation of the salivary and lacrimal glands).
- Oncology (tumors).
Against the background of a sluggish infection with the Epstein Barr virus, a person often develops other types of herpes or bacterial infections. The disease becomes widespread and is difficult to diagnose and treat. Therefore, the Einstein virus often occurs under the guise of other infectious chronic diseases with wave-like manifestations - periodic exacerbations and stages of remission.
Types and stages of the disease
The disease has the following code according to ICD-10 (International Classification of Diseases) - B27.0.
Today, medicine has not developed a unified classification of IVEB - Epstein-Barr viral infection. The disease is usually divided into:
- according to the method of infection - infection can be congenital, that is, it occurred in the mother’s womb and acquired;
- according to the flow phase - it can be active and inactive;
- according to the degree of manifestation and severity of the course - mild, moderate and severe;
- according to the duration of the disease - acute form, protracted and chronic presence of infection are distinguished;
- for reasons of occurrence - due to the penetration of only one virus - EBV and mixed infection (combined, mixed infection) - when another pathogen is present, most often cytomegalovirus (we wrote about the symptoms of cytomegalovirus in children and women here);
- according to the form of manifestation of the disease - typical (in the form of infectious mononucleosis) and atypical - without pronounced symptoms, erased and accompanied by damage to the patient’s organs.
The incubation period of the disease lasts on average from 1 to 2 months in adults; in young children it is much shorter. The disease in the acute phase can last from 1 to 3 weeks.
With the most positive outcome of this process, the patient can recover - the DNA of the virus is detected using a special study only in single B-lymphocytes or epithelial cells.
Virus carriage: chronic infection
All types of herpes viruses reside in the human body for life. Infection often occurs asymptomatically. After the initial infection, the virus remains in the body until the end of life (stored in beta lymphocytes). In this case, a person often does not realize that he is a carrier.
The activity of the virus is controlled by antibodies produced by the immune system. Without the opportunity to multiply and manifest itself actively, the Epstein-Barr infection sleeps as long as the immune system functions normally.
Activation of EBV occurs with a significant weakening of protective reactions . The reasons for this weakening may be chronic poisoning (alcoholism, industrial emissions, agricultural herbicides), vaccination, chemotherapy and radiation, tissue or organ transplantation, other operations, prolonged stress.
. After activation, the virus spreads from lymphocytes to the mucous surfaces of hollow organs (nasopharynx, vagina, ureteral canals), from where it reaches other people and causes infection.
Medical fact: herpes viruses are found in at least 80% of people examined. Bar infection is present in the body of the majority of the adult population of the planet.
Epstein Barr: diagnosis
Symptoms of Epstein Barr virus are similar to those of cytomegalovirus
(also herpetic infection No. 6, which manifests itself as a long-term acute respiratory infection). It is possible to distinguish the type of herpes and name the exact causative virus only after laboratory tests of blood, urine, and saliva.
Testing for Epstein Barr virus includes several laboratory tests:
- Blood is tested for Epstein Barr virus. This method is called ELISA (enzyme-linked immunosorbent assay) and determines the presence and amount of antibodies to the infection . In this case, primary antibodies of type M and secondary antibodies of type G may be present in the blood. Immunoglobulins M are formed during the first interaction of the body with an infection or when it is activated from a dormant state. Immunoglobulins G are formed to control the virus during chronic carriage. The type and quantity of immunoglobulins allows us to judge the primacy of the infection and its duration (a high titer of G bodies is diagnosed with a recent infection).
- Saliva or other biological fluid of the body (mucus from the nasopharynx, discharge from the genitals) is examined. This test is called PCR and is aimed at detecting viral DNA in liquid samples . The PCR method is used to detect various types of herpes viruses. However, when diagnosing the Epstein Barr virus, this method shows low sensitivity - only 70%, in contrast to the sensitivity of detecting herpes types 1, 2 and 3 - 90%. This is explained by the fact that the bara virus is not always present in biological fluids (even when infected). Since the PCR method does not provide reliable results for the presence or absence of infection, it is used as a confirmation test. Epstein-Barr in saliva - says that there is a virus. But it does not show when the infection occurred, and whether the inflammatory process is associated with the presence of the virus.
Diagnosis of the virus
The main diagnostic steps are instrumental methods that confirm the presence of the virion in the human body. But before prescribing these methods, the doctor must first make a diagnosis.
Based on the above symptoms, at the appointment the doctor must carefully collect an anamnesis of the disease and the patient’s life and conduct an objective examination. The following will help with this disease:
- examination to identify exanthema;
- palpation and percussion to determine polyadenopathy and hepatosplenomegaly;
- Auscultation can detect complications of the underlying disease in the form of pneumonia or bronchitis with the addition of a secondary infection.
After establishing a preliminary disease, the attending physician prescribes laboratory and instrumental tests.
- Complete blood count - detection of atypical mononuclear cells more than 10%, increased ESR, lymphocytosis, monocytosis, leukocytosis with a shift to the right.
- Liver tests - increased acute phase proteins (C-reactive protein, seromucoids, sialic acids), increased ALT, AST, total bilirubin.
- Serological reactions - enzyme-linked immunosorbent assay (ELISA) allows you to find immunoglobulins in the blood and determine the severity of the process. An acute process is diagnosed when immunoglobulins of class M are detected, and a chronic course is confirmed by the presence of immunoglobulins of class G. Concentration in the blood is also important: the diagnosis is considered doubtful if the cell level is more than 20 U/ml.
- Determination of the presence of viral DNA by polymerase chain reaction (PCR). Today, the PCR method is the most sensitive, as it can determine the presence of a virus even by a minimal amount of DNA of a foreign organism in various biomaterials (saliva, blood, nasopharyngeal swab, liver and spleen biopsy, cerebrospinal fluid).
- If necessary, consultations with an ENT doctor, surgeon, gastroenterologist, oncologist, and hematologist are possible. To determine the hypertrophy of the sternal and mediastinal lymph nodes, radiography and computed tomography are used.
Epstein Barr virus in children: symptoms, features
Epstein-Barr virus in a child with normal (average) immunity may not cause painful symptoms. Therefore, infection of children of preschool and primary school age with the virus often occurs unnoticed, without inflammation, fever or other signs of illness.
The Epstein-Barr virus in adolescent children often causes a painful manifestation of the infection - mononucleosis (fever, enlarged lymph nodes and spleen, sore throat). This is due to a lower protective reaction (the reason for the deterioration of immunity is hormonal changes).
Epstein-Barr disease in children has the following features:
- The incubation period of the disease is reduced - from 40-50 days it is reduced to 10-20 days after the virus penetrates the mucous membranes of the mouth and nasopharynx.
- The recovery time is determined by the state of immunity. A child’s defensive reactions often work better than an adult’s (as evidenced by bad habits and a sedentary lifestyle). Therefore, children recover faster.
How to treat Epstein-Barr in children? Does treatment depend on the person's age?
Virus structure and stages of reproduction
Professor Epstein described the structure of the virus quite accurately. He classified it in the group of herpes viruses. On average, the particle has a size of up to 150 nm, which explains its easy penetration into the body.
Encode the virion envelope over 8 proteins (proteins). This means that the virus has a complex structure and rich protection in an environment that is aggressive for foreign cells in the human body. For example, the number of proteins of various classes in herpes types 1 and 2 (human herpes simplex) does not exceed 20 units.
Each unit of the virus has a capsid with a protein shell. Inside the capsid is the DNA of the virus. It is double-stranded, which means a more complex structure and development of the viral particle.
On the surface, the virion has a simple system that allows it to attach to a cell of the human body and inject its DNA into the nucleus.
The simple and convenient system of genome transfer explains the ease of penetration and the large number of infected people. Once on the mucous membrane, the virus will almost 100% enter a healthy cell and begin to multiply.
Further steps are provided by a set of enzymes that enter the cell along with DNA. Foreign genetic information replaces human DNA and is replicated.
Apoptosis (rupture) of the cell occurs, during which foreign particles containing DNA scatter throughout the body and penetrate other healthy cells.
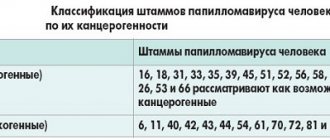
The virus is able to replicate inside B lymphocytes, and with the help of its capsid proteins (nuclear (EBNA), capsid (VCA), early (EA) and membrane (MA) antigens) passes undetected.
They help not only prevent the immune system from killing the affected cells, but also activate their proliferation. It is the active growth in the number of B-lymphocytes that provokes the development of malignant neoplasms.
In addition to the lymphatic system, the cells are carried with the blood throughout the body. They can be found in liver puncture, cervical mucosa, heart muscle and other organs.
Epstein Barr virus in children: treatment of acute infection
Since EBV is the least studied virus, its treatment is also under research. For children, only those drugs are prescribed that have passed the stage of long-term testing with identification of all side effects . There are currently no antiviral drugs for EBV that are recommended for the treatment of children of any age. Therefore, pediatric treatment begins with general supportive therapy, and only in cases of urgent need (threat to the child’s life) are antiviral drugs used. How to treat Epstein bar virus in the stage of acute infection or when chronic carriage is detected?
In acute manifestations, the Epstein-Barr virus in a child is treated symptomatically. That is, when symptoms of sore throat appear, they gargle and treat the throat; when symptoms of hepatitis appear, medications are prescribed to support the liver. Vitamin and mineral support of the body is required; in case of long-term protracted course, immunostimulating drugs
. Vaccination after suffering from mononucleosis is postponed for at least 6 months.
Chronic carriage cannot be treated unless it is accompanied by frequent manifestations of other infections and inflammations. For frequent colds, measures to strengthen the immune system are necessary - hardening procedures, walks in the fresh air, exercise, vitamin and mineral complexes.
Epstein Barr virus: treatment with antiviral drugs
Specific treatment for the virus is prescribed when the body cannot cope with the infection on its own. How to treat Epstein bar virus? Several areas of treatment are used: counteracting the virus, supporting one’s own immunity, stimulating it and creating conditions for the full development of protective reactions. Thus, the treatment of Epstein-Barr virus uses the following groups of drugs:
- Immunostimulants and modulators based on interferon (a specific protein that is produced in the human body when a virus intervenes). Interferon-alpha, IFN-alpha, reaferon.
- Drugs containing substances that inhibit the proliferation of viruses inside cells. These are valacyclovir (Valtrex), famciclovir (Famvir), ganciclovir (Cymevene), and foscarnet. The course of treatment is 14 days, with intravenous administration of drugs recommended for the first 7 days.
Important to know: the effectiveness of acyclovir and valacyclovir against the Epstein Barr virus is under research and has not been scientifically proven. Other drugs - ganciclovir, famvir - are also relatively new and insufficiently studied; they have a wide list of side effects (anemia, disorders of the central nervous system, heart, digestion). Therefore, if Epstein-Barr virus is suspected, treatment with antiviral drugs is not always possible due to side effects and contraindications.
During treatment in hospitals, hormonal drugs are also prescribed:
- Corticosteroids are hormones that suppress inflammation (they do not act on the causative agent of infection, they only block the inflammatory process). For example, prednisolone.
- Immunoglobulins - to support immunity (administered intravenously).
- Thymic hormones - to prevent infectious complications (thymalin, thymogen).
If low titers of the Epstein Barr virus are detected, treatment can be restorative - vitamin
s (as antioxidants) and drugs to reduce intoxication (
sorbents
). This is maintenance therapy. It is prescribed for any infections, diseases, diagnoses, including those with a positive test for the Epstein-Barr virus. Treatment with vitamins and sorbents is allowed for all categories of sick people.
Clinical manifestations
Depending on the severity of the process, the virus can manifest itself in different ways. Let's consider the clinical manifestations of infectious mononucleosis, since the virus is the direct cause of the disease, when during other pathologies described above, the particle appears to be only a factor in its occurrence.
That is, the virus was not detected in all cases, but there was often a connection with infectious mononucleosis.
Acute course
Infectious mononucleosis does not begin to develop immediately after the virus is introduced into the body. This will take some time.
The incubation period for disease manifestation varies from 2 days to 2 months. On average it is 5-19 days.
The disease does not begin with an acute clinically developed process; it has a prodrome period. This is like a preparatory stage. At this moment, the particles had already entered the bloodstream, but did not have time to affect the internal organs and lymph nodes.
It lasts several days (3-4). The prodromal period is associated with general weakness, malaise, headache, and low-grade fever.
The full clinical picture begins with a sharp rise in temperature and sore throat. The symptoms are completely reminiscent of a sore throat. The process involves the palatine tonsils, which swell, become hyperemic and hypertrophied.
There is a possibility of even the addition of a secondary infection with the appearance of islands of pus (catarrhal tonsillitis flows into the lacunar form).
Infectious mononucleosis is dangerous because in the first days the symptoms of sore throat are the only signs. But after 3-4 days, a high temperature (39-40 degrees) appears, intoxication syndrome appears and a rash on the body is possible.
Rashes on the body can be of different types. They can appear as spots, papules and even vesicles.
A distinctive feature is generalized lymphadenopathy. But it can also be missed if you do not pay due attention to the examination of the body.
Lymphadenopathy is also characteristic of ordinary streptococcal sore throat. But it affects only the posterior and submandibular lymph nodes.
In turn, infectious mononucleosis affects all groups (behind the ear, occipital, submandibular, cervical, inguinal, axillary, elbow, popliteal, retrosternal - which can be palpated).
The nodes reach sizes of up to 2 cm. On palpation, they have a doughy structure, not fused with the skin and subcutaneous adipose tissue.
Enlarged nodes do not cause discomfort in the form of pain. The skin is not changed. Sometimes they are compared to potatoes in a bag.
That is, palpation is reminiscent of “feeling” a root vegetable through burlap. The height of lymphadenopathy occurs at the end of the first week of the acute process, and subsides by the end of the second.
Internal organs are also affected. But not due to parenchymal processes, but due to the enlargement of the subcapsular lymph nodes.
The liver and spleen are affected - hepatosplenomegaly is observed. This can provoke a short-term appearance of signs of parenchymal jaundice (yellowing of the sclera and visible mucous membranes and skin, darkening of urine, acholia).
After a month, the size of the organs returns to normal. The enlargement of the spleen is explained by the ability of the virus to activate the replication of lymphocytes. And this organ, as you know, is the main depot of the latter.
Widespread contamination of virus cells in the body and massive release into the blood can provoke the development of focal symptoms of nerve damage.
Serous meningoencephalitis is characteristic. Fortunately, with properly selected therapy, the complication quickly regresses with complete restoration of lost functions.
Epstein-Barr herpes virus (lymphoma)
Chronic course
The protracted and chronic course of the Epstein Barr herpes virus has the same symptoms as in the acute process. But they are expressed less intensely.
No high temperatures. It acquires a chronic low-grade fever. Due to exhaustion of the body, the child notices constant fatigue and fatigue.
Lymphadenopathy is still pronounced. There are no manifestations of tonsillitis either, but you can think about chronic tonsillitis due to hypertrophy of the tonsils. The liver and spleen are moderately enlarged, which reduces the risk of rupture of the organ capsule.
The nervous system is more affected. The patient feels overwhelmed and weak. Sleep inversion occurs (insomnia at night, drowsiness during the day), and is susceptible to frequent depression. The child experiences a decline in school performance, weakened attention and concentration.
An EBV-infected person complains of night sweats (excessive sweating), aching pain in the joints, and a rash in the form of an exanthema may be observed.
Herpes Barr can cause a persistent dry cough in the form of grunting. Not only the palatine tonsils hypertrophy, but the entire lymphatic pharyngeal ring of Pirogov. Therefore, with an increase in the pharyngeal tonsil, constant nasal congestion and nasal sound occur.
Bacterial flora can join the chronic process, which provokes the appearance of vaginosis, thrush, and fungal infections.
How to cure Epstein Barr virus
Medical research is asking the question: Is the Epstein-Barr virus a dangerous infection or a quiet neighbor? Is it worth fighting the virus or focusing on maintaining immunity? And how to cure Epstein Barr virus? The answers from doctors are mixed. And until a sufficiently effective cure for the virus is invented, we must rely on the body's immune response .
A person has all the necessary defense reactions against infections. To protect against foreign microorganisms, it is necessary to have good nutrition, limit toxic substances, as well as positive emotions and the absence of stress. Failure in the immune system and infection with the virus occurs when it is weakened. This becomes possible with chronic poisoning, long-term drug therapy, and after vaccination.
The best treatment for a virus is to create healthy conditions for the body, cleanse it of toxins, provide adequate nutrition , and enable it to produce its own interferons against infection.
Therapeutic measures
It is impossible to completely destroy the herpes virus in the body. Even with proper treatment, it is present in immune cells throughout the patient's life. The causative agent of infection is activated when the body's defenses are weakened. There is no single treatment regimen; drugs are selected taking into account the individual characteristics of the body. No highly specialized drugs have been developed. Infectious mononucleosis is treated in a hospital setting, rehabilitation takes place at home. For mild cases of the disease, hospitalization is not required.
During the acute period, it is necessary to exclude any physical activity, observe special drinking regimes, and adhere to a diet. Fatty and fried foods, smoked foods, sweets and marinades are removed from the menu. Fermented milk products, meat, fresh vegetables and fruits are healthy. If constant fatigue occurs, you need to reconsider your daily routine, normalize your sleep, and start taking vitamins.
Drug therapy is aimed at strengthening the immune system, relieving symptoms of the disease, and accelerating the recovery process. In acute infectious mononucleosis, standard antiviral drugs may be ineffective. But for generalized forms of Epstein-Barr herpes and infection-related malignant tumors, the use of these medications increases the chances of recovery. Interferons are not prescribed during an exacerbation of viral mononucleosis. They are used only for severe forms of the disease. The drugs are prescribed for recovery from infectious mononucleosis. They contain antibodies active against the virus. They capture Epstein-Barr virions and remove them from the body. Medicines of this pharmacological group are used only in hospital settings.
In case of bacterial infections, antibacterial therapy is prescribed. For infectious mononucleosis, penicillin drugs are not prescribed. Vitamins are used after completion of antiviral therapy, as well as when chronic fatigue syndrome occurs. Antihistamines eliminate the symptoms of acute mononucleosis and reduce the risk of dangerous consequences.
There is currently no cure for the Epstein-Barr virus. In the acute period of the disease, symptomatic treatment, adjustments to diet and lifestyle are prescribed.
NSAIDs are prescribed in the presence of pronounced signs of intoxication of the body. Aspirin, Prednisolone and Dexamethasone should not be used. Hormonal drugs can be prescribed for the generalized form of Epstein-Barr herpes. Antibacterial sprays prevent the development of sore throat. Hepatoprotectors are prescribed for toxic liver damage. Sorbents accelerate the process of removing harmful substances from the body, which is especially important during an exacerbation period. The treatment regimen is selected taking into account the severity of the disease, the state of the immune system and the presence of concomitant pathological processes.