Scleroderma is a chronic connective tissue disease that is traditionally classified as an autoimmune rheumatic disease. The most visible manifestation of the disease is thickening of the skin.
Initially, the disease was called “progressive systemic sclerosis,” but this term is not entirely correct, since scleroderma does not always progress. Symptoms of the disease vary from patient to patient. Scleroderma is not a contagious, infectious, cancerous or malignant disease.
HOW DANGEROUS IS SCLERODERMA?
As with many chronic diseases, scleroderma can be dangerous. Symptoms vary widely and the effects on the body can range from minor to life-threatening.
The degree of danger varies depending on which part of the body is affected and the extent of the damage. A mild case can develop into a serious one if treatment is chosen incorrectly. A quick and accurate diagnosis and treatment under the supervision of qualified specialists reduces the symptoms of scleroderma to a minimum and reduces the chances of causing irreversible harm to the body.
Causes of the disease
The causes of this disease are not fully understood. It is assumed that the development of pathology is influenced by genetic factors. There is a hereditary predisposition to autoimmune diseases. This does not mean that the disease will appear immediately after birth; the pathology can develop at any age.
In people with a tendency to scleroderma, the following factors can trigger the onset of the disease:
- past infections;
- hormonal disorders;
- hypothermia (especially frostbite on the hands and feet);
- molecular mimicry of microorganisms, which results in increased activity of lymphocytes;
- hormonal disorders;
- intoxication with drugs or chemicals;
- poor ecology of the place of residence;
- work associated with harmful effects (for example, in chemical production).
The environment and human health are closely interconnected. Very often, the development of scleroderma is provoked by living in a region with a large number of industrial enterprises. This is especially true for the juvenile form of the disease, which manifests itself at an early age. Silicon dioxide, white spirit, welding gases, ketones, solvents, trichlorethylene can have a harmful effect. Not every person whose work involves these substances will necessarily develop the disease. But with a hereditary predisposition, the risk of scleroderma due to constant contact with chemical compounds is very high.
WHAT TYPES OF SCLERODERMA ARE THERE?
Scleroderma is usually divided into two types:
- Localized scleroderma
- Systemic scleroderma
In the future, other classifications with different characteristics and prognosis for the course of the disease may be developed.
- Localized (limited) scleroderma. Changes usually appear as local lesions of the skin or muscles, which rarely spread beyond the affected areas. As a rule, the disease is relatively mild and does not affect internal organs. Patients suffering from a localized form of the disease rarely develop systemic scleroderma. Some abnormalities in laboratory tests characteristic of systemic scleroderma are often absent in the localized form.
- Morphea (focal scleroderma). A form of localized scleroderma, which is characterized by the formation of waxy plaques on the skin that vary in size, shape and color. The skin under the plaques may become thickened. Such plaques can change size over time and often disappear on their own. Morphea usually occurs between the ages of 20 and 50, but is often seen at younger ages.
- Linear scleroderma. A form of localized scleroderma, at the beginning of which the appearance of compacted, waxy lesions in the form of a strip on the skin of the arm, leg or forehead is characteristic. Sometimes, on the head or neck, such a stripe can develop into a long fold, reminiscent of a mark from a blow with a saber or sword. Often, linear scleroderma affects not only the superficial layer of the skin, but also its deeper layers. In some cases, movement of the joints located under the lesion may be difficult. Typically, the disease develops in childhood. Children with linear scleroderma may experience abnormal growth of the limbs.
- Systemic scleroderma (systemic sclerosis). This type of disease affects connective tissue in many parts of the body at once. It can affect the skin, esophagus, gastrointestinal tract (stomach and intestines), lungs, kidneys, heart and other internal organs, and, in some cases, blood vessels, muscles and joints. The tissue of the affected organs hardens, fibrosis develops in it, as a result of which the functioning of these organs is disrupted.
The disease, as a rule, has two main forms: diffuse and limited. With diffuse scleroderma, skin thickening occurs faster and more extensively than with the limited form. In addition, patients with diffuse scleroderma have a higher risk of developing “sclerotic changes,” i.e. fibrous compaction of internal organs.
Antibiotics for skin diseases, psoriasis, scleroderma - tablets, ointments
Ointment for rashes in children
The reaction of the child's body to the action of any irritant manifests itself very violently. This may be a mild rash, itching, burning, pustular manifestations and other negative symptoms. A long-term allergic reaction leads to the development of dermatitis. Ointment for rashes in children can relieve discomfort and restore skin health.
- Fenistil
Antiallergic drug with a sedative effect. It is used for urticaria, allergic rhinitis, drug and food allergies. Helps eliminate itching in atopic dermatitis, insect bites, and chickenpox. The product is applied in a thin layer to the affected areas of the epidermis 1-3 times a day.
How to treat fungus
Fungal skin diseases are very resistant. To completely get rid of them, an integrated approach to treatment is required. It is necessary to contact a medical institution to find out the type of pathogen that has affected the skin. A competent dermatologist will be able to select ointments for mycosis, as well as other antifungal agents and immunostimulating drugs.
If a fungal infection is detected at an early stage, it can be cured by using anti-fungal ointment on the skin. If you notice peeling and itching on the skin (the skin of the feet is especially susceptible to this), you should start using antifungal agents.
Compliance with the following rules will help increase the effectiveness of treatment:
- Before using any ointment, it is necessary to clean the skin of contaminants using warm water and soap, and dry thoroughly;
- It is necessary to change daily underwear that is in direct contact with the skin surface infected with mycosis;
- It is necessary to treat the inner surface of the shoes of a patient with mycosis of the feet (for example, wiping with ammonia, chlorhexidine, miramistin);
- Most often it is necessary to take systemic antimycotic drugs;
- It is necessary to follow the regimen for using ointment against skin fungus. Usually the regimen prescribed by the doctor coincides with that proposed in the instructions for the drug. But sometimes, based on the situation, a specialist may recommend a different frequency and duration of treatment. As a rule, therapy for mycoses lasts from several weeks to several months;
- Sometimes it is necessary to continue therapy for a couple of weeks after recovery from mycosis;
- When selecting a drug, it is necessary to take into account its side effects;
- You should switch to ointments containing corticosteroids only after treatment with conventional antifungal creams and ointments has been tried and has not yielded a positive result.
Antibiotic ointments
Used for the treatment and prevention of rashes complicated by inflammation and bacterial infection. Most often, patients are prescribed the following medications:
- Gentamicin sulfate
It has a wide spectrum of antimicrobial action and inhibits the growth of most harmful microorganisms. After use it is well absorbed. Main indications for use: treatment and prevention of skin rashes caused by infection. Helps with furunculosis, dermatitis, trophic ulcers, burns.
The dosage and duration of therapy are individual for each patient. The medicine is applied to the affected skin 2-3 times a day for 7-14 days. In case of overdose, side effects are possible: ototoxic effect, itching, irritation. Contraindicated for use in case of a history of allergic reactions, impaired renal or liver function. Not suitable for treating pregnant women and newborns.
- Lincomycin ointment
Antimicrobial agent with antibiotic. Suitable for the treatment of pustular lesions of the skin and soft tissues. Apply a thin layer to the affected areas 1-2 times a day.
Contraindicated for use in case of kidney and liver diseases, or a history of allergic reactions. Long-term therapy can cause itching, burning, swelling and an increase in the number of rashes.
- Levomekol
A group of medications that include hormones, antibacterial, anti-inflammatory and fungicidal substances. They are used if the rash is severe and accompanied by infection and inflammation.
- Flucinar
Contains the active substance – fluocinolone acetonide. It has a pronounced anti-inflammatory and antiallergic effect. It is well absorbed and accumulates in the skin. Biotransformed in the liver, excreted by the kidneys in the form of metabolites.
Antibiotics are used exclusively in cases where the disease is caused by bacterial flora. Correct antibiotic treatment can only be prescribed by a doctor.
Antibacterial drugs differ in their spectrum of action; this is primarily taken into account when prescribing them. Antibiotics, which have a broad spectrum of action, are prescribed for diseases with an unknown pathogen.
Antibiotics are divided into 5 groups:
- Penicillin group;
- Group of cephalosporins;
- Macrolides;
- Tetracycline group;
- Aminoglycosides.
Plus, each of the 5 groups is divided into 2 subgroups:
- Wide spectrum of action;
- Narrow spectrum of action.
Broad-spectrum antibiotics can suppress the proliferation of a large number of pathogenic bacteria. Narrow-spectrum antibiotics are aimed at killing only certain bacteria. A separate group includes antisyphilitic and antituberculosis drugs.
Narrow-spectrum antibacterial drugs:
- Erythromycin;
- Penicillin;
- Oxacillin.
Depending on what disease the patient is suffering from, he is prescribed drugs of a certain group and subgroup of antibiotics.
Just a few decades ago, many diseases were treated with an antibiotic such as penicillin. Medicine does not stand still, and now, when determining a bacterial infection that has affected the human body, a special antibiotic is prescribed, which is aimed at destroying this bacterium.
These medications are highly effective for diseases caused by streptococci and staphylococci. They are also used in the treatment of sexually transmitted diseases, respiratory tract infections, endocarditis, sepsis, central nervous system lesions, purulent skin lesions, cystitis, peritonitis, otitis, prostatitis and many other diseases.
For example, streptococci cause a purulent disease - streptoderma. Here you can read more about what streptoderma is in children.
Since each medication has a huge number of contraindications, it is necessary to consult a specialist before use.
Our skin is our largest organ and has many important functions. The beauty and health of a person depends on the skin. Skin diseases are not only unpleasant, but in many cases they are dangerous to health. Antibacterial therapy is used to treat some skin diseases, if they are infectious.
The following diseases are treated with antibiotics:
- Eczema;
- Erysipelas;
- Lymphocytoma;
- Pemphigus of newborns;
- Acrodermatitis atrophying;
- Lupus erythematosus;
- Some types of lichen;
- Infected skin lesions;
- Scleroderma;
- Furunculosis.
Antibacterial drugs of the penicillin group are currently used for skin diseases. These medications are effective in getting rid of infectious skin diseases. They are best used by intramuscular injection.
Antibiotics for the treatment of skin diseases:
- Benzylpenicillin potassium or sodium salt;
- Semi-synthetic penicillins are used in the treatment of infectious dermatosis caused by streptococcus and streptococcus.
- Oxacillin. This drug is used by intramuscular injection, as well as in the form of tablets and capsules.
- Ampicillin. A drug that has a wide spectrum of action and effectively fights many skin diseases.
- Ampiox. This antibiotic contains oxacillin and ampicillin. It has proven itself well in the treatment of dermatoses.
Antibiotics in tablet form
Antibiotics in the form of capsules and tablets are convenient to use because they can be taken at home. Plus, they can be taken by pregnant women and children with minimal risk of side effects.
Some of the most commonly prescribed drugs in the form of tablets and capsules are:
- Ecoclave;
- Amoxiclav;
- Flemoxin;
- Panclave;
- Augmentin;
- Flemoclav.
The main disadvantage of taking drugs of the penicillin group is that they can cause severe allergies. This group of antibiotics treats skin diseases well for a long time.
Injectable forms of antibiotics
Antibiotics in the form of injections are more effective than the same drugs in the form of capsules and tablets.
In the treatment of skin diseases, injections of cephalosporin antibiotics are most often used, such as:
- Cefazolin;
- Ceftriaxone;
- Cephalexin;
- Cefuroxime;
- Ceftibuten;
- Cefipime;
- Kefzol.
Antibiotics of this subgroup are effectively used in the treatment of skin diseases in advanced cases.
It is also worth noting that in the treatment of many skin diseases, in addition to antibacterial drugs in tablets and injections, ointments with antibiotics are used. Ointments are applied by applying to damaged areas several times a day. The advantages of ointments are that they have virtually no side effects and are easy to use. With their help, treatment can take place at home.
For skin diseases, ointments such as:
- Levomikol;
- Tetracycline ointment;
- Streptocide emulsion.
Ointments help reduce the number of rashes, reduce burning and itching.
Antibiotics for psoriasis
Psoriasis is a skin disease that has become widespread recently. It is impossible to completely cure psoriasis, but there is a way to reduce the number of flare-ups. If, during the next exacerbation of psoriasis, an infectious focus is detected in the patient’s body, which became the cause of the exacerbation of the disease, then antibiotics cannot be avoided.
Antibacterial therapy is also necessary for weeping forms of this disease, since infection may occur. The antibiotic is selected depending on where the inflammation occurs.
Antibiotics for scleroderma
Scleroderma is another skin disease that is treated with antibiotics. They mainly use drugs of the penicillin group and their analogues. This disease affects internal organs, which is why the choice of antibiotics depends on which organs are affected and at what stage the disease is. And also on the age of the patient.
One of the disadvantages of antibacterial therapy is the large number of contraindications and side effects. For example, broad-spectrum antibiotics have many more side effects than narrow-spectrum drugs.
The most common side effects include:
- Nausea;
- Vomit;
- Diarrhea;
- Constipation;
- Headache;
- Allergic reactions;
- Disruption of the cardiovascular system;
- Kidney disorders.
Each antibiotic has its own individual side effects. And if you notice side effects while taking antibiotics, you need to change them.
Contraindications to the use of antibiotics indicate that this drug may not only not be beneficial, but also have a negative impact on health.
The most common contraindications to the use of antibiotics are:
- Allergy;
- Liver or kidney diseases;
- Pregnancy, first and second trimester;
- Breastfeeding period;
- Children's age, especially, this applies to strong antibiotics.
Pregnant women and children can use antibiotics only in case of a serious infection, which would be quite problematic to cure without antibiotics. If you are taking any other medications in addition to antibiotics, you should consult a specialist. Since some medications can react with antibacterial drugs and cause undesirable effects.
Wounds can be located on any part of the body and in any organ. After receiving an injury, you should consult a doctor about the necessary treatment. Typically, therapy is limited to sterile dressings with the following creams or ointments:
- Baneocin is a drug from the group of aminoglycoside antibiotics. Has a wide spectrum of action.
- Levomekol is one of the representatives of chloramphenicol.
- Erythromycin ointment is one of the budgetary means for treating wounds.
- Lincomycin ointment belongs to the lincosamide group of drugs.
Ointments containing antibiotics should be used only for the treatment of purulent wounds, since their frequent use leads to the development of resistance in bacteria. This means that with long-term use they will not have the necessary therapeutic effect.
Features of the use of ointments with antibiotics:
- As a rule, the ointment is applied to the site of injury (wound, inflammation) in a thin layer, lubricating the site of injury well. However, there are ointments that, on the contrary, are applied in a thick layer and must be absorbed into the skin on their own. However, a more detailed method of using the ointment can be prescribed by your doctor, as well as the frequency of its use, but it is recommended to apply the ointment at night.
- The duration of use of the ointment is also determined by the doctor or depending on the speed of healing of the injury (wound).
It is important to note that in order to avoid the appearance of various pimples, boils, and blackheads in the future, you need to adjust your diet by getting rid of fatty, fried, salty foods, sweets, and also get rid of alcohol abuse and smoking.
Non-hormonal ointments
Treatment of skin rashes should begin with a visit to the doctor. A qualified specialist will determine the cause of the disorder and select the optimal therapy that will be effective in each individual case. Knowing the names of ointments for skin rashes, it is much easier to navigate when choosing the appropriate medication.
They have anti-inflammatory, antiseptic, and in most cases antipruritic and analgesic properties. Medicines in this category are suitable for eliminating rashes on the face, as they have a gentle effect. They are prescribed for children from an early age.
- Gistan
It has anti-inflammatory, antiexudative and antipruritic properties. Induces the release of proteins that are responsible for the biosynthesis of inflammatory mediators by inhibiting the release of arachidonic acid. Reduces inflammatory exudate, processes of granulation and infiltration. Rashes and inflammation go away due to the formation of a chemotaxis substance.
Negative skin reactions may occur upon contact with various substances. Rashes, burning, and peeling appear on different parts of the body. For treatment, an ointment for rashes on the body is used, which is used as prescribed by a doctor. As a rule, these are combined products that not only restore the epidermis, but relieve inflammation, hyperemia and moisturize.
Let's consider popular topical preparations for the treatment of rashes on the body:
- Advantan
An external preparation with the active ingredient – methylprednisolone aceponate. The active component is a non-halogenated synthetic steroid. Suppresses allergic and inflammatory reactions, reduces pain and symptoms.
Very often, skin rashes are accompanied by itching, burning and dryness. Ointment for rashes and itching eliminates discomfort and accelerates the regeneration processes of damaged skin. Let's consider effective medications from this group:
- Protopik
Local therapy is used in the treatment of many diseases, including sexually transmitted diseases. Ointment for syphilitic rash is included in the category of such drugs. Medicines anesthetize skin rashes, eliminate peeling, and resolve dense formations. A rash with syphilis appears at all stages of the disease, but the sooner treatment is started, the higher the chances of eliminating it.
Consider effective ointments for syphilitic rash:
- Hexicon
Antiseptic with the active ingredient – chlorhexidine bigluconate. Active against gram-positive and gram-negative microorganisms, including Treponema pallidum, Chlamydia spp., Ureaplasma spp. and other bacteria.
- Indications for use: syphilis, bacterial vaginosis, colpitis, ureplasmosis, gonorrhea, genital herpes. Various skin infections: paronychia, pyoderma, impetigo, diaper rash. Not prescribed for intolerance to the components and for pediatric patients. The product is applied to the affected areas of the epidermis 1-2 times a day for 7-10 days.
- Cases of overdose are unlikely, since the substance has low systemic absorption. Allowed during pregnancy and lactation with appropriate medical permission. Adverse reactions manifest themselves in the form of allergies, which disappear after discontinuation.
- Zigerol
Locally applied preparations, such as ointments, creams, gels, sprays, can be very effective, especially if a small area of skin is affected by mycosis at the initial stage of the disease. Having familiarized yourself in detail with the composition and effect of means for the treatment of mycosis, you can form your own idea of which ointment will best help against fungus.
Erythromycin ointment contains erythromycin as its main component, which is a strong antibiotic from the macrolide group. The product is produced in Russia and is available in the form of an eye and external ointment. The excipients in the drug include: lanolin, sodium disulfite and petroleum jelly.
Erythromycin has pronounced bactericidal activity against a number of pathogens: Staphylococcus aureus and dermal Staphylococcus, Streptococcus, Clostridia, Corynebacteria, Neisseria, Bordetella, Haemophilus influenzae, Treponema pallidum, Legionella.
But the ointment contains only 1 antibiotic, so many pathogens have developed resistance. These include: E. coli, Shigella and Salmonella.
Most often in this group, skin diseases are caused by E. coli, especially in older people. Erythromycin is used in patients with allergies to penicillin drugs.
Indications for prescribing erythromycin ointment are:
- purulent infections of the skin and soft tissues (abscess, furunculosis, carbuncles);
- vulgar and juvenile acne;
- infected wounds;
- thermal and sunburns with blisters (2nd or 3rd degree);
- bedsores and ulcerative lesions.
Lincomycin ointment is a domestic antibacterial drug, which is available in tubes of 10 and 15 g. The ointment contains lincomycin hydrochloride as an active substance, which, when entering the body, is converted into active lincomycin.
It has bactericidal activity against many gram-positive bacteria: staphylococci, streptococci, pneumococcus, diphtheria pathogen, etc. It has a weak pathogenic effect against anaerobic clostridia and mycoplasma.
To speed up skin healing processes, it is recommended to apply it up to 2 times a day for 2 weeks. Afterwards, you need to undergo a re-examination by a doctor. Side effects develop with increasing duration of treatment and dose of the drug. These include:
- dyspepsia: nausea, vomiting, diarrhea, abdominal pain, flatulence;
- skin lesions in the form of an allergic reaction: rash, dermatitis, urticaria, angioedema;
- liver damage with the development of jaundice and an increase in bilirubin in the blood serum;
- changes in blood tests: neutropenia, thrombocytopenia, leukopenia - these conditions are reversible.
Contraindications to the use of antibiotics
It is not recommended to use this kind of ointment only if a person has hypersensitivity to antibiotics or is completely intolerant to them, which can lead to various side effects.
Therefore, it is important to act as prescribed by your doctor. Although to date there have not been any negative consequences of using antibiotic ointments for pregnant women, it is still better for them to refrain from doing so in order to avoid negative consequences.
SYMPTOMS OF SCLERODERMA
Signs and symptoms depend on what part of the body is affected:
- Skin. Almost all patients with scleroderma experience severe hardening and swelling of the skin. Such lesions may be oval or straight line shaped, or cover a large area of the trunk or limbs. Their number, location and size depend on the form of scleroderma. Due to severe swelling and limited movement, the skin in the affected areas may take on a shiny hue.
- Fingers or toes. An increased reaction of the body to low temperatures or to emotional stress in the form of numbness, soreness or discoloration of the fingers is one of the first signs of the development of systemic scleroderma. This condition, called Raynaud's syndrome, can also occur in people who do not have scleroderma.
- Digestive system. In some cases, in addition to acid reflux, which causes damage in the lower esophagus closest to the stomach, patients with scleroderma and impaired intestinal muscle motility associated with the disease may have problems absorbing nutrients.
- Heart, lungs, kidneys. The disease affects the heart, lungs and kidneys to varying degrees. If problems with these organs are left untreated, they can lead to serious consequences, even life-threatening./li>
https://youtu.be/xcAfXhSJQMg
Drugs for the treatment of psoriasis: effective and new drugs
Psoriasis is a disease of the human skin, accompanied by the formation of rashes on the body that are very itchy and flaky. Often the pathology takes on quite dangerous forms for the patient’s life. Pustular psoriasis, psoriatic arthritis, and erythroderma are considered to be severe types of the disease. To treat pathology, medications are most often used for internal use and external application.
Types of medications
All medications for psoriasis are divided into drugs for the treatment of psoriasis internally, as well as external agents. External preparations are ointments on a hormonal or non-hormonal basis, vitamin preparations. Medicines for internal use may be as follows:
- cytostatics;
- anti-inflammatory drugs;
- hepatoprotectors;
- keratolytics;
- immunosuppressants;
- biological products;
- sedatives;
- antiallergic drugs;
- immunomodulators;
- vitamin complexes.
All medications for psoriasis are prescribed by a doctor, taking into account the individual characteristics of the patient and the severity of the disease.
Medicines in the form of ointments
Ointments for psoriasis can be hormonal and non-hormonal. The use of certain remedies depends on the symptoms of the pathology and its severity. In the first stages of the disease, non-hormonal drugs are most often used.
Non-hormonal ointments
Ointments of this group have anti-inflammatory, analgesic, disinfecting, drying, restorative effects. The drugs help relieve itching, redness, and swelling. Often used for the treatment of psoriasis:
- Salicylic ointment is a keratolytic agent used to treat various skin diseases. The medicine is well tolerated by patients, does not cause addiction, and rarely causes side effects.
- Zinc paste – the product contains zinc. The substance has a drying and disinfecting effect when psoriatic rashes appear.
- Zinocap is an excellent anti-inflammatory and antifungal agent. The active component here is zinc pyrithione. Zinocap relieves peeling of the dermis, itching, redness and swelling.
- Losterin belongs to naphthalene-based products. The ointment has anti-inflammatory, vasodilating, wound-healing, antimicrobial effects. In addition, the medicine contains urea and salicylic acid.
- Psoriaten is a homeopathic medicine based on herbal components. The ointment normalizes the process of cell division, has antipruritic, anti-inflammatory, regenerating effects.
Non-hormonal drugs are considered relatively safe. Their advantages include:
- good action;
- lack of withdrawal and addiction effects;
- minimal number of side effects;
- relatively low price, availability of drugs;
- no disturbance in the hormonal balance of the body.
Among the disadvantages, experts note that the effect of treatment does not occur immediately. You have to wait some time for the desired result. Because of this, in severe cases of pathology, non-hormonal ointments are ineffective.
Hormonal ointments
Hormonal or glucocorticosteroid ointments are widely used today to treat pathology. Hormones for psoriasis give a quick effect, which makes them very popular in the treatment of severe forms of the disease. Commonly used ointments include:
- Trocar is a drug based on triamcinolone. The medicine is used to treat various dermatitis, eczema, and psoriasis. To get rid of plaques, it is recommended to apply the ointment to the affected areas several times a day.
- Flucinar - used in short courses for skin pathologies, copes well with the manifestations of psoriasis, such as itching, swelling, redness, inflammation, peeling. The active component here is fluocinolone acetonide. The drug is perfectly absorbed into the skin and has an immediate effect.
- Silcaren is an ointment based on mometasone. The medicine quickly and effectively eliminates itching, which is an important condition for the treatment of psoriasis and other dermatitis.
- Hydrocortisone is a product based on hydrocortisone acetate. The ointment is indicated for eczema, psoriasis, neurodermatitis, and insect bites.
Medicines for the treatment of psoriasis containing hormones have a number of contraindications.
The drugs often provoke a number of systemic side effects. Undesirable consequences include:
- atrophy of the skin;
- formation of stretch marks;
- development of acne;
- pigmentation of the dermis;
- the appearance of spider veins;
- digestive system disorders;
- cardiovascular pathologies;
- difficulty breathing.
To avoid complications, it is recommended to use all hormonal drugs strictly as prescribed by your doctor. Self-medication is unacceptable.
Oral medications for psoriasis
In addition to the use of ointments, drugs for the treatment of psoriasis are used orally to treat pathology. Let's look at the most popular medications for psoriasis in the form of tablets, vitamins, and injections.
Immunomodulators
Medical treatment for psoriasis in most cases involves the use of immunomodulators. The actions of this group of drugs include:
- establishing metabolic processes;
- reduction of the inflammatory process;
- providing a desensitizing effect;
- stimulation of the production of liver enzymes;
- increasing immunity;
- reducing the toxic effect of certain drugs.
Medicines against psoriasis in this group may be as follows:
- Glutoxim.
- Timalin.
- Pyrogenal.
The drugs are prescribed in the form of complex therapy, taking into account the characteristics of the pathology.
Immunosuppressants
Medicine against psoriasis in the form of immunosuppressants is based on the suppression of a person’s natural defenses, which is necessary to get rid of some forms of the disease. Under the influence of the active substances of the drug, the body's immune cells are suppressed. As a result, the manifestation of symptoms such as peeling, itching, redness, and inflammation is reduced.
Drug treatment of psoriasis using immunosuppressants is carried out taking into account all contraindications of drugs. These include:
- the presence of infectious diseases in the patient;
- deterioration of blood composition;
- kidney and liver pathologies;
- allergy to the components of the drug;
- It is not recommended to use the products in children;
- It is prohibited to take immunosuppressants during pregnancy and lactation.
Commonly used drugs include:
- Thymodepressin.
- Stelara.
- Remicade.
Most often, drugs in this group are prescribed to patients with severe forms of the disease, such as psoriatic arthritis, pustular psoriasis, and erythroderma.
Steroid drugs
Hormonal drugs are used to achieve a rapid therapeutic effect in severe forms of pathology.
Popular means include:
- Diprospan.
- Dexamethasone.
- Diprosalik.
Hormones are used in courses. With long-term treatment, patients experience the development of side effects. To prevent complications, steroid medications are taken in strict accordance with the instructions of the attending physician.
Enzyme preparations
Drugs for psoriasis are often used in the form of enzymes. With a long course of the pathology, in many patients the normal functions of the digestive system are disrupted, the liver ceases to perform its natural functions due to the use of certain medications. Enzymes are used to maintain the body. For this purpose, the following is used in medical practice:
- Mezim.
- Creon.
- Pancreatin.
- Wobenzym.
Medicines help restore normal gastric microflora, promote good absorption of vitamins, and support normal liver function. Medicines for psoriasis in the form of enzymes are an important aspect of treatment, ensuring the fastest achievement of the desired result.
Sorbents
Oral medications for psoriasis also include drugs in the form of sorbents. The goal of therapy is to remove harmful substances, waste, and toxins from the body, which is important for cleansing the skin of plaques.
Among the sorbents used:
- Activated carbon.
- Smecta.
- Enterosgel.
- White coal.
- Sorbex.
Sorbents are relatively safe and rarely cause the risk of complications and side effects.
Antibiotics for psoriasis
Antibiotics are prescribed if a complication such as a secondary infection occurs. To fight infection use:
- Cefaclor.
- Ceftriaxone.
- Lomacin.
- Neomycin.
Antibiotics have the ability to suppress both pathogenic and beneficial microorganisms. Probiotics are used to restore beneficial microflora. These are drugs such as Linex, Baktisubtil, Eubicor.
Antibiotics are used strictly as prescribed by a doctor; in the absence of indications, taking these drugs can only worsen the situation.
Hepatoprotectors
Hepatoprotectors are drugs for the treatment and restoration of liver function. The liver performs such an important role for the body as filtering blood. During the course of psoriasis, a large amount of harmful substances passes through the liver. Hepatoprotectors are used to maintain the organ. Popular drugs include:
- Allohol.
- Antral.
- Karsil.
Medicines restore liver cells and help normalize the regeneration of organ tissue.
Sedatives
Drug treatment of psoriasis at home often includes the use of anti-allergenic drugs. Drugs that have a sedative effect help eliminate itching, peeling, redness, and swelling. Among this group they use:
- Diazolin.
- Claritin.
- Zyrtec.
- Suprastin.
The course of treatment is prescribed by a doctor, its duration depends on the severity of the pathology.
New drugs for psoriasis
Today, there are effective medications for psoriasis in the form of biological products. A peculiarity of the use of such drugs is that during treatment with their help it is necessary to abandon any other medications. The method of administering biological products is injections of special active substances for psoriasis. The choice of drug depends on the severity of the pathology:
- Enbrel is often used to treat postriatic arthritis. The medicine effectively eliminates the manifestations of pathology. It is prohibited to use the drug for diseases of the cardiovascular system, kidney and liver pathologies.
- For pustular, guttate, plaque psoriasis, Remicad is used. The course of therapy ranges from 4 to 8 weeks. It is prohibited to use the product if infectious diseases develop.
New drugs for the treatment of psoriasis are safe and effective. Despite this, using the funds yourself is strictly prohibited.
MEDICATIONS
At the moment, there is no drug that can stop the main disease process in the body - excessive collagen synthesis. However, there are various medications on the market that help control the symptoms of scleroderma and prevent complications from occurring. To achieve this effect, they:
- Dilate blood vessels. Medicines to normalize blood pressure help to widen (dilate) blood vessels and prevent problems with the lungs and kidneys, and also help fight Raynaud's syndrome.
- Suppress the immune system. Drugs that suppress the immune system, such as those given after organ transplantation, may also relieve the symptoms of scleroderma.
- Reduces the acidity of gastric juice. Medicines such as omeprazole (Prilosec) help relieve symptoms of acid reflux.
- Prevents the occurrence of infections. Antibiotic ointments, good hygiene and protection from low temperatures prevent infection of finger ulcers with Raynaud's syndrome. Regular flu and pneumonia vaccinations can help protect lungs affected by scleroderma from infection.
- Relieves pain. If over-the-counter pain relievers are not effective enough, your doctor may prescribe stronger medications.
Scleroderma - what is this disease?
The disease in question is an autoimmune damage to any connective tissue and blood vessels against the background of both inflammation and generalized fibrosis and disturbances in the microcirculation of biological fluids. The term “scleroderma” can be explained more simply by what this lesion is:
- skin;
- structures of the musculoskeletal system;
- kidney;
- hearts;
- digestive tract organs;
- liver.
Scleroderma - pathogenesis
To develop effective therapy and search for new medications for this pathology, it is important to understand the mechanisms of its development. Since the 40s of the last century, scleroderma has been studied, what it is and how to treat the disease.
The causes or factors provoking the problem have not yet been precisely established, but the mechanisms of its progression have been thoroughly determined.
A key role in the pathogenesis of the disease belongs to humoral and cellular immunity. Disturbances in their work lead to an increase in the concentration of CD4+ and B lymphocytes. A hypersensitivity reaction occurs, and a huge number of autoantibodies and circulating protective complexes of various types are formed. Fibroblasts become hyperactive and attack both the connective tissues and blood vessels of the body.
Excessive production and accumulation of collagen begins. This simultaneously provokes acute inflammatory processes, which quickly develop into a chronic form, which is difficult to treat. Because of these features, the definition of what scleroderma is includes the word “autoimmune.” The cells of the defense system perceive their own organic structures as foreign and destroy them.
Scleroderma - causes
The exact factors causing changes in immune function are not yet known. The knowledge gained through medical research helps to determine only the mechanisms due to which scleroderma occurs, what it is, and how to treat the pathology. There are several theories of the origin of the described disease and individual etiological hypotheses. Scleroderma may have the following causes:
- genetic predisposition;
- cytomegalovirus infection;
- streptococcal sore throat;
- complications of influenza;
- prolonged exposure to chemicals;
- taking medications such as cytostatics;
- stress;
- hypothermia and frostbite;
- mechanical injuries of the body;
- exposure to vibration;
- hormonal changes;
- improper vaccination;
- surgical interventions, including operations in the oral cavity (tooth extraction, tonsil removal).
METHODS FOR DIAGNOSTICS OF SCLERODERMA
Diagnosing scleroderma can be difficult because the disease comes in many forms and affects different areas of the body.
After a thorough physical examination, the doctor may order the patient to undergo blood tests to check the level of antibodies produced by the immune system. To examine the skin for abnormalities, your doctor may take a small sample of tissue from the affected area (biopsy).
Spirography (lung function test), CT scan of the lungs and echocardiogram of the heart may also be prescribed.
How to treat scleroderma at home? Folk recipes
I won’t hide it, systemic scleroderma is a serious disease, and recovery is difficult: it should be carried out with the active participation of the patient and his relatives.
For treatment, available medicinal plants are used, used in the form of decoctions, infusions, tinctures, juices, ointments, inhalations, and applications.
Sources of natural silicon used for all dermatitis, problems with cartilage, bone, and connective tissue are horsetail, knotweed, dandelion, birch leaves and buds.
Among the plants that improve blood flow, sweet clover, horse chestnut, and stinging nettle are effective; anti-inflammatory drugs - calendula officinalis flowers, barberry root, raspberry leaf, blackberry leaf, birch leaf, walnut leaf; natural regenerators - plantain, licorice root; immunity correctors include duckweed, wheatgrass roots, and burdock.
For localized scleroderma
When only the skin is affected, a medicinal mixture has worked well, in which all the plants, dried and crushed, are taken in equal proportions, for example, 30-50 grams. These are licorice root, wheatgrass, string grass, sage, duckweed, calendula flowers, black elderberry, meadowsweet, nettle leaf, birch, currant.
Take 1 tbsp. spoon of the mixture, pour 0.5 liters of water, bring to a boil, keep on low heat for 5-7 minutes. Leave for 1 hour, then, after straining, add 1 tbsp to the broth. a spoonful of honey and 1 tbsp. a spoonful of juice (plantain, elderberry, burdock, to choose from). Take 70-100 ml before or after meals 3-4 times a day. Heal until the entire collection is over.
Externally, use calendula ointment (sold at the pharmacy) - apply a thin layer to the affected areas of the skin 2 times a day. You can prepare such an ointment with an anti-inflammatory effect yourself by mixing dried, powdered calendula flowers with baby cream or castor oil in a ratio of 1:3 or 1:5.
But what plants will help with systemic scleroderma
If pulmonary lesions are observed, the collection will include plantain, lungwort, licorice root, wheatgrass, marshmallow, elecampane, linden flowers, calendula, duckweed, thyme, string. All dried, crushed components of the collection are also taken in equal parts, 30-50 g each, and the decoction is prepared according to the same scheme as for the localized form.
The only difference is that in addition to burdock and plantain juices, you can add thyme and elderberry juices to the broth, also to choose from.
For joint lesions, we give preference to the roots of burdock, rose hips, cinquefoil, licorice, wheatgrass, and water lilies; birch, raspberry, currant leaves; poplar buds. The cooking method is the same as in previous recipes. Of the juices that come as an additional component, I can recommend the juices of burdock, birch, and rowan.
New developments in the treatment of scleroderma
Medical scientists have long been studying the nature of scleroderma: what it is and how to treat this complex and serious disease. After all, traditional methods of therapy do not lead to complete elimination of the disease. New methods of treatment are being searched, drugs are being developed that can more effectively influence the pathology.
A new genetically engineered drug, Tocilizumab (Actemra), has been created. This drug is an antibody to interleukin-6 receptors. It is this anti-inflammatory cytokine that is the provoking factor in the occurrence of scleroderma and rheumatoid arthritis. Clinical studies have shown the effectiveness of the drug.
A new complex method of therapy with the enzyme “Lidase” in combination with vitamin preparations “Pantogam”, “Dexpanthenol” and “Picamilon” has been proposed. This method is effective for focal forms of the disease. Biologically active substances help improve metabolism in affected tissues.
Currently, research is being conducted on drugs that could block the signaling pathway for the development of scleroderma. Inhibitor molecules that can affect the pathogenesis of the disease are being investigated. This could help prevent fibrosis, an overgrowth of connective tissue. New developments in the treatment of scleroderma are also associated with the use of stem cells. They are able to replace diseased cells. This leads to a decrease in fibrosis and the formation of new blood vessels to replace those that were damaged by pathology.
How does systemic scleroderma affect blood vessels?
Finally, when the vascular muscles relax, more blood than normal enters the vessels, they become congested, and the fingers or toes become intensely red. Due to the typical sequence of color changes (white, blue, red), many compare this tricolor to the French tricolor flag. Individual Raynaud's attacks can be caused by low outside temperatures, working in cold water, and emotional stress. In addition to discoloration, patients will complain of tingling in the fingers and numbness.
Raynaud's phenomenon sometimes appears long (months or even years) before skin changes develop. It can also occur in the context of other diseases and even for no apparent reason. Some experts believe that spasms of blood vessels in the fingers, nose, and ears occur in every tenth inhabitant of the planet, and connective tissue damage occurs in only 5% of them. In general, systemic scleroderma should be ruled out first when a patient reports tricolor vascular attack.
When vascular spasms are repeated over a long period of time, the ends of the fingers eventually become permanently swollen and the skin becomes inflamed. The toes and lower legs may also be affected. This is the first stage of the disease.
In general, changes in the dermis go through three successive stages:
The patient has the following complaints:
With systemic scleroderma, the skin becomes hard not only on the limbs, but also on the face. Small wrinkles formed during life gradually disappear. The person looks strangely young, his face becomes amicable, and he has difficulty expressing his emotions. The eye slits become narrow, the face resembles a mask. The tip of the nose becomes pointed and may become ulcerated. The patient cannot open his mouth the same way as before (microstomia), it is difficult for him to eat and brush his teeth, it is difficult for him to stick out his tongue and smile. Even the frenulum of the tongue shortens and thickens. Tightening of the skin on the upper body can make breathing difficult. Upon contact with the skin there is a feeling of stiffness.
Of all the internal organs, the esophagus is the most commonly affected by systemic scleroderma: in more than 60 percent of patients, the esophagus hardens, dilates, and becomes immobile. Because the muscles of the esophagus are no longer able to move chewed foods into the stomach, patients usually suffer from difficulty swallowing (dysphagia).
Changes also occur in the oral cavity - it shrinks and becomes dry.
The sphincter muscle between the esophagus and stomach becomes atonic and no longer functions properly. As a result, acidic stomach contents can flow into the esophagus. Gastroesophageal reflux, also called reflux disease, occurs. Ulcers appear in the lower part of the esophagus.
Like the esophagus, the connective tissue in the stomach can harden. Because the stomach wall is then unable to stretch and move sufficiently, this often causes bloating, aerophagia, or nausea after eating. The corresponding changes in the intestines can lead to both constipation and diarrhea. Fecal incontinence may develop. If nutrients through the thickened intestinal wall can no longer be fully absorbed into the bloodstream, the result is unwanted weight loss.
In 80% of patients with scleroderma, lung tissue is involved in the process. Typically, the layer of connective tissue that lies between the air-filled alveoli and the blood vessels of the lungs is very thin so that oxygen molecules can diffuse into the blood. When systemic scleroderma accumulates connective tissue fibers (pulmonary fibrosis), the lung tissue becomes stiffer and thicker, and diffusion capacity is reduced. Oxygen saturation drops. The result of impaired gas exchange is shortness of breath, especially during physical exertion and coughing.
Pathological changes in the pulmonary connective tissue can lead to high blood pressure in the lungs. Pulmonary arterial hypertension causes stress on the right ventricle of the heart. Physical performance decreases as pneumosclerosis progresses, and patients suffer from shortness of breath or even dizziness as soon as they make a slight effort.
High pressure in the arteries of the lungs strains the muscles of the right ventricle. In the long term, this direct cardiac strain can lead to weakness of the right ventricle (right heart failure).
In addition, in the process of systemic scleroderma, collagen fibers increase in all areas of the heart muscle (myocardium) - not only in the right ventricle, but also in the left ventricle and in the two atria. Myocardial fibrosis develops. Because the heart muscle is under severe strain, heart failure occurs. Sometimes a heart defect develops.
In addition to heart failure, deposition of collagen fibers in the heart muscle can cause various types of cardiac arrhythmias. The reconstructed areas of connective tissue conduct electrical current much worse than healthy heart muscle and prevent the propagation of electrical impulses in the heart. Heart damage is manifested by pain behind the sternum, sudden palpitations, arrhythmia, cyanosis of the nasolabial triangle, shortness of breath with slight physical effort.
If the disease affects the blood vessels in the kidneys, kidney function deteriorates (renal failure occurs): water and mineral salts, as well as waste products of the body's metabolism such as creatinine and urea, accumulate in the body and blood pressure rises. Victims complain of headaches, malaise, and fluid accumulation (edema) in the lower extremities. Chronic renal failure develops with ascites and impaired consciousness. Hardening of the renal vessels can lead to acute nephropathy, which can be fatal.
Systemic scleroderma sometimes causes inflammation of the tendon sheaths (tenosynovitis), joints (arthritis), fingers, or skeletal muscles (myositis). With myositis, the affected muscles hurt and their strength decreases. Contractures appear that disrupt the functions of the joints and limit their mobility. The deformation of the hand with bent fingers makes it look like a bird's foot.
The disease is classified into four forms according to the nature of skin changes and the degree of organ involvement during the disease
In localized systemic scleroderma, hardening of the skin on the arms, legs and face is limited. The first sign of the disease is usually episodic circulatory problems in the fingers or toes (Raynaud's phenomenon). After the first Raynaud's attack, it usually takes several years for the disease to become visible - the skin will become noticeably tight. The disease then continues to progress slowly: internal organs are often affected only after years or even decades. This form includes the so-called CREST syndrome (outdated name). CREST - syndrome is an abbreviation in English, the initial letters of the list of the most common symptoms of scleroderma
C-Calcinosis cutis - dense calcifications under the skin in the form of calcium salts, they periodically open, forming ulcers that become the gateway to infection.
R-Raynaud - Raynaud's phenomenon, which occurs due to a sudden spasm of small vessels under the influence of a cold agent.
E - Esophageal dysmotility - inflammation of the esophagus due to damage to smooth muscles, impaired motility with symptoms of dysphagia and heartburn
S - Sklerodaktylie - thickening of the skin of the fingers, swelling of the hand;
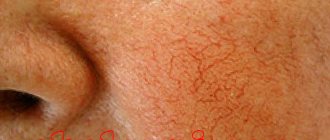
T - Teleangiektasien - dilated capillaries in the form of stars, especially in the face
Skin changes may visually appear
Local scleroderma is considered benign in course, the prognosis is favorable.
With diffuse systemic scleroderma, symptoms develop much more quickly: after the first Raynaud's attack, it takes less than a year until the first hardening of the skin is felt. They occur in the reverse order of the limited form, affecting the upper body first, then the face, and finally the arms and legs. Internal organs are often affected several years after the onset of the disease.
- Undifferentiated
Patients with the undifferentiated form suffer from Raynaud's attacks, persistently swollen fingers, and pulmonary arterial hypertension. This form of the disease may lack the roughening of the skin that is typical of other types of SSc. Scleroderma without scleroderma is a rare form (about 2% of cases)
- Cross forms of scleroderma.
Complaints and anamnesis in adults and children
- Itchy skin (common complaint).
- Difficulty swallowing solid foods. May be accompanied by difficulty swallowing liquids and subsequent nausea, vomiting, weight loss, abdominal cramps, wet diarrhea and fecal incontinence.
- The patient may experience shortness of breath during exercise and at rest.
- Rapid heartbeat without characteristic chest pain, fatigue and shortness of breath.
- Joint pain, limited movement, joint swelling and muscle pain.
REFERENCE! Systemic sclerosis first manifests itself as joint pain in 15%. As inflammatory myopathy – in 10% of patients. Weakness and general malaise – in 80% of patients.
Symmetrical swelling of the fingers and hands appears, which is generalized to involve the forearms, face, trunk and lower extremities. Over time, the swelling develops into hard, associated induration and fibrosis, which eventually causes deformation of the fingers.
Complaints in children include
- loss of skin's ability to stretch;
- reduced hand functionality;
- severe sensitivity to cold;
- enlarged blood vessels on the hands, face, and around the nail beds;
- subcutaneous calcium deposits (calcinosis).
The history of the disease and the study of the patient’s complaints are closely intertwined with the history of the development of scleroderma.
The medical history will consist of both personal and family medical history.
The anamnesis (in addition to biographical information) includes information about:
- bad habits;
- first manifestation of the disease;
- severity of symptoms;
- hereditary pathologies causing systemic sclerosis;
- provoking factors (stress, acute and chronic infectious diseases, physical and chemical irritants);
- possible therapy.
Treatment
Treatment of systemic scleroderma is a lifelong process, and the regimen is always chosen individually
Experts take into account the course of the disease, the nature of the pathology, the form, and the degree of damage
It is extremely important for patients to follow all doctor’s recommendations and undergo regular examinations. The main objectives of the prescribed therapy are:
The main objectives of the prescribed therapy are:
- Prevention of vascular complications.
- Suppressing the progression of internal organ damage and skin fibrosis.
- Reducing activity and suppressing disease progression.
- Prevention and treatment of Raynaud's syndrome.
- Reducing swelling and tightness of the skin.
- Prevention of visceral manifestations of the disease.
To treat Raynaud's syndrome, it is recommended to wear warm clothes, avoid stressful situations or exposure to cold on the skin, and give up bad habits and drinking coffee. Factors provoking the disease reduce the effectiveness of treatment and lead to a slow but progressive pathology. One of the risk factors is ultraviolet radiation, which provokes an exacerbation of the disease. During periods of solar activity, you should avoid visiting open areas without special means to protect your skin.
Drug treatment
Taking medications is aimed at stabilizing the functional state and achieving the stage of remission, suppressing the activity of the process
It is also important to restore the function of internal organs, or prevent their damage if the disease is detected in the early stages. For this, the following types of drugs are prescribed:
Non-steroidal anti-inflammatory drugs (Ibuprofen, Piroxicam, Indomethacin). They are aimed at suppressing the inflammatory process in soft tissues, providing pain relief and improving the patient’s well-being. Vascular agents (“Foridon”, “Nifedipine”, “Corinfar”). These drugs block calcium channels, so they are widely prescribed at the initial stage of the disease. But they differ in effectiveness as the pathology progresses. Anti-inflammatory drugs (“Cuprenil”). They suppress the inflammatory process in tissues and have a pronounced antifibrotic effect. Prescribed for rapid progression of pathology
Prescribed with caution, as some types of drugs can have undesirable effects on the kidneys and intestines. Immunosuppressants (“Cyclophosphamide”, “Azathioprine”, “Methotrexate”)
They are effective against damage to muscles and joints, suppress the inflammatory process at the early stage of the disease, and slow down its progression. Glucocorticosteroids (Prednisolone, Dexamethasone, Metipred). They are prescribed in the later stages, during the acute course of the disease. But they definitely require constant monitoring of the condition of the kidneys, as they can have a negative effect on them. Enzyme agents (Ronidaza, Lidaza). Prescribed for chronic disease in the form of injections. Their peculiarity is to reduce the viscosity of hyaluronic acid.
The use of genetically engineered biological products is considered a new technique, but their effectiveness has not been proven today and is only at the study stage. This is a new direction in the treatment of systemic scleroderma. Such drugs include Inflixicamb and Etarnecept, but doctors prescribe them only as part of experimental treatment.
Changing your diet is an important part of treatment
Nutrition correction
Patients should definitely reconsider their diet not only for the period of taking medications, but also for the rest of their lives
It is important to design the menu in such a way that there are short intervals between meals and the portions are small. Foods high in protein are completely eliminated from the diet.
First of all, this applies to products such as:
- Fermented milk products.
- Seafood.
- Milk, kefir, fermented baked milk.
- Spicy cheese.
- Meat and fish.
- Products rich in calcium.
The presence of concomitant pathologies, such as renal failure, requires that food intake be strictly dosed, in compliance with a strict diet. Patients with systemic scleroderma are recommended to eat foods rich in vegetable oils and polyunsaturated acids, as they help suppress the inflammatory process in the body. Carbohydrates are consumed limited.