H1 CC
Skip to content
- cosmetologist
- Contacts
Home »Facial care »Facial masks
Most often, women experience complexes about their face, because it is considered a calling card. And these complexes concern not so much the shape of the eyes or the thickness of the eyebrows, but rashes on the skin.
One of the most significant problems for many women is facial skin like an orange peel. Why does this problem appear and what can be done at home to get rid of it?
Reasons for appearance
The human body has a huge number of exocrine glands, which perform an important function: through the production of sebum (sebum), the glands nourish, moisturize, protect and soften the skin. Features of the localization of such glands, in particular on the face, provoke the progression of seborrhea:
- in the frontal region;
- on the eyebrows;
- nasolabial “triangle”;
- scalp.
When a malfunction occurs in the body, sebum is produced in excess and “works against a person” - it becomes a favorable environment for the development of fungal and infectious diseases. More often, facial seborrhea is accompanied by excessive activity of the secretion organs.
But in medical practice, there are cases of dry seborrhea of the face, when, under the influence of various factors, the function of the glands is inhibited. The third type of pathology is mixed, when both manifestations of seborrheic dermatitis occur.
In each case, the chemical composition of sebum changes, which disrupts the oxygen exchange of the skin, reduces the protective functions of the epithelium and provokes irritation.
The main “provocateur” of the development of seborrhea is the opportunistic yeast-like fungus Pityrosporum (pityrosporum), which parasitizes the hair follicles, as well as the exocrine glands.
Normally, pityrosporum is found on the surface of the skin in 90% of people, but in the presence of a favorable environment, it begins to actively multiply and acquire pathogenic properties.
The reasons for the appearance of seborrhea on the face and the activation of the fungus are caused by the following factors:
- genetic predisposition;
- hypovitaminosis, weakening of the body's protective functions;
- pathologies of the endocrine system, including hormonal imbalance (increased testosterone), diabetes mellitus;
- stress, overwork, violation of work and rest schedules;
- disruption of the central nervous system;
- chronic diseases of the gastrointestinal tract and liver;
- insufficient facial skin care, lack of proper hygiene.
Men are more susceptible to oily seborrhea of the facial skin. This fact is due to an excess of testosterone in the male population, the peak of which activity occurs during puberty (from 12 to 20 years). But in some cases, pathology manifests itself regardless of gender and age.
Despite the constant improvement of methods for diagnosing and treating seborrhea, experts still cannot establish the reliable causes of its occurrence.
Previously, the main causative agent of the disease was considered to be the subcutaneous mite, but this theory has long been refuted, since this parasite can activate its activity during seborrhea, but is not its cause.
Other factors that contribute to the appearance of symptoms of this disease include:
- Genetic predisposition and poor heredity. In cases where a person has close relatives suffering from this disease, he is at risk.
- An adolescent factor that contributes to the development of seborrhea during puberty, when the concentration of hormones of the corresponding type in the blood increases significantly.
- The presence of various pathological processes in the body or diseases, for example, the development of testicular tumors in men.
- Malfunctions in the body, for example, due to poor functioning of the gastrointestinal tract or infectious lesions of the central nervous system.
- Taking hormonal contraceptives or steroid drugs.
- A decrease in the body’s immune defense, due to which it loses the ability to control the process of reproduction of a number of parasitic and fungal formations, which leads to disruption of the functioning of the glands.
- A person’s stay in a depressed or depressed state for too long, frequent stressful situations.
- Lack of a balanced and healthy diet, especially when consuming large amounts of fatty foods or honey.
- Paralysis of certain nerves or the presence of nerve diseases.
For most women, “orange peel” appears on the nose, forehead, and cheeks due to some unfavorable circumstances. It can be:
- sudden climate change (for example, during a vacation);
- frequent and prolonged stay in rooms with high humidity;
- intensive use of any poorly selected cream;
- abuse of purely decorative cosmetics - foundations and powders;
- a lifestyle that is very far from healthy.
However, sometimes the cause should be sought directly in the individual, congenital characteristics of the body or in age-related changes. It is possible that the problem was a consequence of hormonal imbalances that accompany puberty or aging.
Why your face itches: the main causes of itching
Doctors of various specialties, including endocrinologists, encounter pathological changes in the skin. Skin lesions can be either an accidental finding or the main complaint of the patient. Skin changes that appear harmless at first glance may be the only sign of a serious illness. The skin is the most accessible organ for research and at the same time a source of the most important information.
Skin lesions can clarify the diagnosis in many internal diseases, including diabetes mellitus (DM). Skin changes in diabetes are quite common. Severe metabolic disorders underlying the pathogenesis of diabetes lead to changes in almost all organs and tissues, including the skin [30].
Some diabetes-associated skin symptoms are a direct result of metabolic changes such as hyperglycemia and hyperlipidemia [4, 7]. Progressive damage to the vascular, nervous, or immune systems also contributes significantly to the development of cutaneous manifestations.
The mechanisms of other diabetes-associated dermatological lesions remain unknown [7, 20]. Hyperinsulinemia may also contribute to skin changes, as seen in the early stages of insulin-resistant type 2 diabetes. Macro- and microangiopathies also significantly aggravate the course of skin complications of diabetes. In combination with large vessel arteriosclerosis, these microvascular abnormalities contribute to the formation of diabetic ulcers.
In addition, diabetes results in loss of cutaneous innervation sensation, which predisposes to infections and damage [16]. As a rule, diabetic skin lesions have a long and persistent course with frequent exacerbations and are difficult to treat.
There are several classifications of skin lesions in diabetes, they are based on clinical characteristics and some aspects of the pathogenesis of skin changes. According to the classification of Khlebnikova A. In the classification described by Andrea A.
Kalus, Andy J. Chien, John E. Olerud [4] distinguish the following groups of diabetes-associated skin lesions: Dermatoses associated with diabetes include diabetic scleredema.
Scleredema is more common in long-term diabetes in combination with obesity and is manifested by diffuse symmetrical indurative skin changes mainly in the neck and upper third of the back, like an orange peel. The pathogenesis of diabetic scleredema has been proposed to involve unregulated production of extracellular matrix molecules by fibroblasts, leading to thickening of collagen bundles and increased deposition of GAG glycosaminoglycans [53].
Patients with diabetic scleroedema may experience decreased pain and light sensitivity in the affected areas of the skin, as well as complain of difficulty moving the upper limbs and neck. In extreme cases, the disease can lead to complete loss of joint mobility, however, the presence of scleredema is not associated with retinopathy, nephropathy, neuropathy or damage to large vessels [4, 25]. A connection with insulin resistance and obesity can be seen in acanthosis nigricans, acanthosis nigricans, which manifests itself as areas of hyperpigmentation of the skin with papillomatous growths in the neck and large folds [34].
Insulin plays a central role in the development of acanthosis. In women suffering from acanthosis, loss of functional mutations of the insulin receptor or anti-insulin antibody receptor syndrome type A and type B can be found [18, 31].
Excessive growth factor stimulation in the skin is thought to cause aberrant proliferation of keratinocytes and fibroblasts, resulting in the clinical manifestations of acanthosis nigricans [52].
In conditions of insulin resistance and hyperinsulinemia, acanthosis can develop due to excessive binding of insulin to IGF-1 receptors on keratinocytes and fibroblasts [27]. Evidence supporting the role of various growth factors in the pathogenesis of acanthosis nigricans continues to accumulate. Undiagnosed diabetes and hypertriglyceridemia can provoke the appearance of eruptive xanthoma on the skin [46, 8]. They are reddish-yellow papules measuring mm.
Pathological elements appear in the form of grains and over time can merge to form plaques. Initially, triglycerides predominate in the skin elements, but since they are mobilized more easily than cholesterol, with their breakdown more and more cholesterol accumulates in the skin [47]. Insulin is an important regulator of LDL activity. The degree of enzyme deficiency and subsequent clearance of serum triglycerides is proportional to the rates of insulin deficiency and hyperglycemia [22].
Clearance of plasma lipoproteins depends on adequate insulin levels [17]. In uncontrolled diabetes, this inability to metabolize and release triglyceride-rich chylomicrons and very low-density lipoproteins can result in plasma triglyceride levels rising into the thousands.
Uncontrolled diabetes is a common cause of massive hypertriglyceridemia [4, 26, 29]. Patients with diabetes are prone to developing skin infections, especially with poor glycemic control. This decrease directly correlates with the severity of diabetes.
Infectious and inflammatory diseases primarily develop on the skin of the lower extremities in connection with angio- and neuropathies. The cause is usually polymicrobial infections: Staphylococcus aureus, group A and B streptococci, gram-negative aerobic bacteria and many anaerobes.
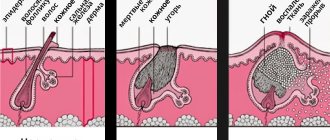
Pyoderma is represented mainly by folliculitis, ecthyma, erysipelas and can be complicated by eczematization. In addition, the development of furunculosis, carbuncles, paronychia, and soft tissue infections is possible [21]. Under conditions of hyperkalemia, fungi actively use sugar for their metabolic processes and multiply intensively, causing disease.
In diabetes, impaired microcirculation in the vessels of the lower extremities is observed 20 times more often than in persons without endocrine pathology, which contributes to the development of fungal infections of the feet and onychomycosis [1]. The causative agents of fungal infections are dermatophytes and Candida albicans.
Moreover, in the normal population, fungal skin lesions caused by C. The most common are intertrigo with damage to the axillary, inguinal areas, interdigital spaces, vulvovaginitis, balanitis, paronychia, glossitis and angular cheilitis.
In addition to symptomatic vaginal yeast infections, patients with diabetes also have an increased incidence of asymptomatic carriage [36]. Diseases associated with diabetes and having an unclear pathogenesis include necrobiosis lipoidica, granuloma annulare, diabetic blister and diabetic dermopathy.
Necrobiosis lipoidica Oppenheim-Urbach disease is a rare granulomatous chronic disease of a vascular-metabolic nature, which is a localized lipoidosis with lipid deposition in those areas of the dermis where there is degeneration or necrobiosis of collagen [15].
The first symptoms of dermatosis usually appear in the age group from 20 to 60 years. Oppenheim-Urbach disease is rare in childhood [13]. The clinical picture of Oppenheim-Urbach disease is very diverse. Various areas of the skin may be involved in the process, but primarily the skin of the anterior surfaces of the legs.
This can probably be explained by the fact that in diabetes, pathological changes initially occur in the small vessels of the lower extremities [10].
Typically, necrobiosis lipoidica appears as one or more well-demarcated yellowish-brown plaques. The elements have purple, jagged edges that may rise above the surface of the skin or become denser. Loss of sensation occurs in the area of plaques [44, 2, 42]. The association of granuloma annulare with diabetes remains a matter of debate, as it may be associated with other diseases [55]. Localized, generalized, as well as subcutaneous nodular and perforating forms of granuloma annulare associated with diabetes have been observed [3, 37, 24].
The typical history of granuloma annulare involves one or more papules growing peripherally with simultaneous resolution in the center. Lesions may retain natural skin color or be erythematous or violet. The usual sizes of lesions range from 1 to 5 cm in diameter [41]. Granuloma annulare is usually asymptomatic; Mild skin itching is possible, painful lesions are rarely observed [33].
Diabetic bullosis is a subepidermal bullous dermatosis that occurs in patients with diabetes [39]. For the first time, blisters were observed as one of the variants of skin lesions in diabetes by D.
Kramer in Cantwell and W. Martz described this condition as diabetic bullosis [23,11]. The cause of blisters in diabetic patients is not clear. There are theories about the role of microangiopathy and local metabolic disorders. Diabetic bullosis occurs mainly in people who have had diabetes for a long time, and somewhat more often in women. The age of onset of the disease ranges from 17 to 79 years. On unchanged skin, blisters ranging in size from several millimeters to several centimeters appear, usually on the skin of the lower extremities [19].
There are two types of lesions: intraepidermal blisters, which disappear without scar formation, and subepidermal blisters, which leave atrophied scars. The rash is localized primarily on the feet and legs, but can occur on the hands and forearms. The blisters resolve spontaneously after weeks, and relapses are possible [45]. Diabetic dermopathy occurs more often in patients with long-term diabetes and is more common among men [29, 40].
Clinically, it appears as small, less than 1 cm atrophic spots, pink to brown in color and resembling scar tissue, located in the pretibial areas. These elements are asymptomatic and disappear after years, leaving behind slight atrophy or hypopigmentation [54].
The appearance of new elements suggests that pigmentation and atrophy are persistent conditions. Exchange-endocrine disorders are often the trigger for the development of certain dermatoses. There is a certain relationship between the course of these diseases and the presence of endocrinopathy.
Often, damage to the oral mucosa with lichen planus is combined with diabetes and arterial hypertension Potekaev-Grinshpan syndrome, and rashes on the mucous membrane, as a rule, are erosive and ulcerative in nature. Against the background of diabetes, psoriasis is more severe, such forms as exudative psoriasis, psoriatic polyarthritis, and large fold psoriasis are observed [32]. Thus, skin changes may well be associated with systemic pathological processes characteristic of diabetes.
The clinical and pathomorphological picture of dermatoses and dermopathy, preceding or developing against the background of diabetes, is based on metabolic, vascular, neurological and immune disorders.
Valeeva F. Sergeeva I. Skin changes in diabetes mellitus are quite common, and doctors of various specialties may encounter this. Diabetes-associated skin symptoms are based on metabolic hyperglycemia, hyperlipidemia, vascular, neurological and immune disorders. The article presents the etiology, pathogenesis, clinical picture and classification of dermatoses that develop with prolonged increases in glucose levels. Many dermatological diseases are associated with insulin resistance and obesity.
Against the background of diabetes mellitus, there is an increased frequency of fungal and bacterial infections, which is most pronounced with unsatisfactory glycemic control.
How to remove orange peel from face?
Methods of dealing with orange peel on the face can be divided into home methods and those carried out in beauty salons. The main measures that should be taken in the fight against orange peel on the face should be aimed at:
- Cleaning pores. This should be done using light soap solutions and cleansing lotions that do not contain alcohol. You can also use scrubs and steam baths.
- Narrowing of flabby areas, which can be achieved by using ice creams from herbal decoctions.
- Toning skin with enlarged pores.
The best solution to getting rid of orange peel on the face is to use complex drugs that have all three of the above actions. Also, products of this type will easily relieve other unhealthy manifestations: greasyness and unhealthy shine.
The services of beauty salons that help get rid of orange peel on the face include the following procedures:
- Peeling is the process of removing the upper stratum corneum of the skin using mechanical action.
- Darsonval therapy is exposure to high-frequency pulsed current.
- Microdermabrasion is mechanical skin resurfacing.
- Laser resurfacing is the process of exposing pores to a laser of a certain frequency and color.
The cost of the procedures cannot be considered budgetary; moreover, their multiplicity is always at least ten, and the duration of one can exceed two hours. Also, salons often have appointments, and the times may be inconvenient for people. That is why these actions are not considered by many people for many reasons.
Home remedies for dealing with orange peel involve applying masks to tighten the skin pores. All the remedies are simple, and most importantly, they can be used at a convenient time, without leaving home. Although no less effort needs to be made and the duration of getting rid of the unpleasant phenomenon on the face will also not be quick.
Excellent remedies in the fight against “orange” skin will be:
- A decoction of linden flowers, which must be prepared from one tablespoon of the preparation, ground into powder, and one hundred milliliters of hot water. The aromatic tea should be boiled for an hour over low heat, and then steeped for another twenty minutes. The cooled broth is applied to the face with cotton swabs, and then left on the skin until completely dry. There is no need to wash off the product.
- Nourishing masks made from fresh fruits or seasonal berries. Whipped protein should be added to all cosmetic products.
- Potato mask made from one potato tuber, grated and mixed with the yolk of a chicken egg. Apply the product to the face and leave for half an hour, after which it is washed off.
- Tomato mask with a narrowing effect. To enhance the effect, add rye bread soaked in water and squeezed out and one tablespoon of vegetable oil to the grated tomatoes. The duration of the application is fifteen minutes. The product should be washed off with cold water.
- A mask made from one tablespoon of fresh lemon zest mixed with a teaspoon of natural olive oil. By using this remedy regularly for a month, you can achieve the desired results. It is only important to know that for those who want to maintain a tan on their face, this product is not suitable.
- A cleansing scrub made from steamed coffee grounds and dry oatmeal, taken in equal quantities.
- A mask made from one beaten chicken protein mixed with one tablespoon of finely grated carrots and three tablespoons of rye flour. The exposure time of the medicinal composition is no more than fifteen minutes, after which the pore narrowing product should be washed off with cool water without soap. After this operation, you should wipe your face with ice cubes and then lubricate with moisturizer or milk.
All of the above remedies must be used for a long time. You should also refrain from using decorative cosmetics at the time of treatment. Vitamins and probiotics can also help in the fight against facial skin problems, which will improve intestinal function, because everyone knows that external beauty begins with order inside the body.
If your face is covered with unevenness, firstly, you need to eliminate the factors that we list above:
- improve working and living conditions;
- cleanse the skin more thoroughly using lotions;
- do not abuse concealers;
- get rid of bad habits.
Secondly, you should contact a cosmetologist and together with him create an individual correction program. Such programs usually include both salon and home treatments.
The salon can provide a professional course of peeling, microdermabrasion, laser resurfacing or darsonvalization. It makes sense to make masks and scrubs yourself. It is advisable to select their specific names and recipes together with a cosmetologist.
Below, just as an example, we name several good masks that tighten pores and tighten the skin:
- “Pure system” by Yves Rocher;
- gel-scrub-mask “Clean Skin” from Garnier;
- Avon White Tea Energizing Face Mask;
- film mask with calendula and rose hips from Green mama.
In addition to purchased products, it is advisable to experiment with coffee, lemon, cucumber, kefir and oatmeal masks.
Getting rid of orange peel in a beauty salon
When you contact a cosmetologist, they will create a program for improving your skin, recommend good facial products, and give recommendations on physical activity and diet.
In addition, the salon will offer you the following procedures:
- Peeling;
- Darsonvalization;
- Microdermabrasion;
- Laser resurfacing.
All these techniques are aimed at cleansing and eliminating imperfections of thick skin. After their use, a short rehabilitation course follows. But you can’t go back to your old lifestyle in order to maintain the results for a long time.
To ensure that the result remains in its original form, pores do not begin to expand and tubercles appear, buy only high-quality facial cosmetics.
- Yves Rocher;
- Garnier;
- Green mama;
- Clean line;
- One hundred beauty recipes.
Eczema is a skin disease characterized by rashes, itching, redness, and swelling. This disease has two forms: dry (flaky eczema) and weeping. Inflammation in eczema is essentially an allergy, but it has many different causes, such as metabolic disorders, prolonged contact with allergens, nervous and endocrine diseases. In this regard, the dermatologist prescribes a comprehensive treatment with an individual approach to each patient.
Eczema occurs in acute or chronic form. It develops cyclically, as relapses occur followed by remission.
This disease is considered a non-infectious disease, although it is not possible to say 100% exactly what causes it. But you can be sure that whatever the skin disease, it is certainly interconnected with the functioning of the intestines. In this regard, the first thing to do is clean it.
To cleanse, people need to eat bran and activated carbon, as these sorbents help remove toxins from the body and prevent intoxication (poisoning).
Translated from Greek, eczema means to boil; it was so named because the rash that appears at first looks like small bubbles, soon they burst and liquid is released. These bubbles look like boiling water.
After this, the skin begins to crust over, the cracks heal, but then bubbles form again. Eczema is completely non-contagious, no matter whether it is flaky or weeping.
Seborrheic
- To prevent infectious complications, be sure to follow the rules of personal hygiene, it is advisable to walk more in the fresh air and sun, as well as swimming in the sea will prevent the development of psoriasis.
- Skin with this type of eczema needs vitamin D, found in foods such as spinach, cabbage, yeast, carrots, unsprouted wheat, and sunflower oil.
Symptoms
Seborrheic dermatitis
- Irritation, peeling, itching and redness of the facial skin, possibly a burning sensation and tightness;
- The formation of white or yellow scales on the face;
- The skin of the face becomes more sensitive even to a soft touch - this causes pain;
- Formation and accumulation of single or multiple papules on the surface of the skin of the cheekbones, forehead, nasolabial folds and eyebrows.
In the initial stages of seborrheic facial dermatitis, red patches usually form, which then turn into yellowish plaques. The rashes grow and take on different shapes.
Seborrheic dermatitis on the cheek
Seborrheic dermatitis on the nose
Seborrheic dermatitis on the face
Seborrheic dermatitis on the eyelid
The most common is oily seborrhea of the face, which is often accompanied by a secondary infection of infectious or fungal origin. Symptomatically, the pathology manifests itself as:
- increased sweating;
- enlarged pores on the face;
- inflammatory processes that provoke redness of the epithelium;
- foci of suppuration;
Dry seborrhea is characterized by:
- the appearance of dry, flaky skin;
- fine dandruff appears on the hair and face;
- hair loss occurs;
- changes in the skin are accompanied by itching and burning;
- Pinkish and red spots of thin epithelium appear on the skin.
The mixed type of disease combines the symptomatic manifestations of the two varieties described above.
Symptoms and types of crusts
The appearance of the lesions is highly dependent on the primary pathology. Often these are dryish dense formations with uneven contours, similar to a wound scab. With secondary infection, they can become very thick. Based on their appearance and composition, the following types of crusts are distinguished:
Serous - dry formations of yellow color, microscopy of which reveals fibrin protein, a small number of leukocytes and destructively altered cells of the epidermis Purulent - gray-green color, fibrin and a large number of leukocytes are visible under the microscope Hemorrhagic - red-brown color, microscopy reveals fibrin, leukocytes and red blood cells
Prevention measures
Compliance with simple rules prevents the primary development of pathology and also reduces the possibility of relapse to a minimum:
- first of all, eliminate the factors that provoked the disease (treat pathologies of internal organs, avoid stressful situations);
- strictly follow a hypoallergenic diet;
- pay attention to skin care cosmetics;
- carefully observe the hygiene of the face and other “seborrheic” areas;
- observe a work and rest schedule in which walks and sea air are recommended.
The main thing in the treatment of facial seborrhea is to identify the primary source of the pathology. Only in this case will the doctor be able to draw up the correct therapeutic regimen to effectively solve the problem in a relatively short time.
Measures to prevent the occurrence of orange peel, the appearance of which is not associated with genetic problems, are simple. They consist of proper care for skin prone to the formation of enlarged pores. The most popular of all warning methods are listed below.
- Healthy lifestyle. If possible, try to avoid stressful situations and overwork. Playing any kind of sport, good company and active pastime, plus proper nutrition will help prevent pore enlargement under other negative conditions.
- Do not use cosmetics that are not age appropriate. Avoid decorative cosmetics from unverified manufacturers. Apply makeup correctly and avoid excess, and in the evening be sure to remove it using gentle products.
- Use stone, coffee or grain scrubs intended for facial and décolleté skin care. Use the product strictly in accordance with the instructions, but be sure to perform the procedure at least once every ten days.
- To wash your face, use soft products based on essential oils and extracts of medicinal herbs. You can also use gels or decoctions of herbs and medicinal plants. The best options would be infusions prepared with hawthorn berries, lemon zest, marigolds, horsetail and chamomile.
Prevention of enlarged pores on the face is also the use of masks to improve blood circulation and. as a result, elasticity and firmness of the skin. The frequency of such procedures is at least once every five days.
We hope that the article was useful to all those who are looking for ways to solve the problem of orange peel on the face, and the proposed simple and affordable skin care products will help instill confidence in themselves and get rid of complexes.
Orange cheeks. Care for oily skin
Don’t be alarmed, cellulite has not yet “climbed” that high.
But, unfortunately, even without its help, facial skin can look similar to a holey citrus peel. The reason for this is enlarged pores. Every person has pores; sebum comes out through them, which performs a protective function. But when the sebaceous glands work too actively and the skin does not receive proper care, sebum, mixing with dead skin cells, gradually stretches the pores.
Squeezing out blackheads (comedones) and poor-quality mechanical cleaning in salons aggravate the problem. If at an early age the skin can still independently resist the stretching of pores, then with age it loses this ability and becomes uneven.
As a result, the face resembles the peel of an orange.
Most often, increased sebum secretion is a problem of adolescence, caused by hormonal changes in the body, and therefore, as a rule, there is no need to influence it from the inside.
But the cause of excessive oily skin after 20 years can be problems in the body, for example, metabolic disorders.
In this case, it makes sense to consult with a gastroenterologist and endocrinologist.
Preventing stretching of pores
Cleansing.
Excessive sebum secretion in the T-zone (on the chin, wings of the nose and forehead) is indicated by combination skin. And all over the face - oily.
Therefore, cleansing products must meet the needs of these skin types. The best option is a gel for daily washing.
It may contain extracts and essential oils of aloe, chamomile, basil, cloves, orange, iris, grapefruit.
After the gel, you need a high-quality lotion or tonic without alcohol, containing astringents such as birch, hawthorn, calendula, lemon, rosemary extract, which will “tighten” the cleansed pores.
Care.
The most common mistake in caring for oily and combination skin is lack of hydration. And it is necessary not only for the general condition of the skin, but also to prevent stretching of pores. After all, sufficiently moisturized skin is elastic and in good shape, therefore, less susceptible to deformation. You need to choose creams with a light texture.
Special program.
Use a facial scrub twice every 7-10 days. It will remove dead skin cells, thereby preventing clogged pores.
Every other day, morning and evening, rinse clean skin with a decoction of chamomile and horsetail (1:1). This will help her cope with excess fat production.
It is useful to make masks 1-2 times a week to regulate the functioning of the sebaceous glands, as well as increase the elasticity and firmness of the skin. For example, this one.
– Mix grated carrots with well-beaten egg whites, grind the mixture thoroughly, adding flour to it until a homogeneous paste forms. Apply to face for 15 minutes. Then rinse off first with warm water, then with cool water. After this, wipe your face with ice and apply moisturizer to damp skin.
Treating pores
Cleansing.
With already enlarged pores, deeper cleansing is required. For this, there are special gels containing glycolic (1-3%) and azelaic acids. Don't forget to tone your skin with a toner for your skin type.
And also give your skin contrasting washes - a few seconds with warm and then cold water. Such small stresses are simply necessary for the skin; they activate metabolic processes.
Such effects open the pores, forcing the skin to breathe, making it more receptive to moisturizing creams.
Care.
To make enlarged pores less noticeable, you should call for help from special cosmetics (creams and serums intended for skin with enlarged pores).
They have a triple effect, control the functioning of the sebaceous glands, tighten pores and make the skin matte. I would like to note: the opportunity to get rid of enlarged pores once and for all with the help of such cosmetics is nothing more than a delusion.
It is impossible to return already stretched pores to their previous size. The effect of such cosmetics is similar to the effect of tights. When the tightening effect of cosmetics ends, the pores expand again.
Therefore, to visually reduce pores, you will have to use special products constantly. By the way, now some tonal products have this effect.
Special program.
Be careful when choosing a peeling product. Opt for gentle scrubs with fine particles or soft and non-irritating gommage masks. Otherwise, large particles entering the pore can injure its walls and cause inflammation.
A blue clay mask will be an excellent “help” in caring for skin with enlarged pores. It absorbs the contents of pores, disinfects, and reduces sebum secretion.
In addition, it removes the surface layer of dead cells and thereby helps the skin renew itself faster. Dilute powdered clay with green tea to the consistency of sour cream. Apply an opaque layer to your face.
After 20 minutes, rinse with water at room temperature. Carry out the procedure 1-2 times a week.
Modern cosmetological techniques can effectively cope with the problem of increased sebum secretion and enlarged pores. You should begin developing a course of procedures only after consultation with a cosmetologist. He will conduct diagnostics, determine your skin type, and identify the causes of enlarged pores.
Ultrasonic facial skin cleansing
An alternative to mechanical facial cleansing is ultrasonic cleansing (due to high sound exposure) – vacuum cleansing + lymphatic drainage (dosed, negative barometric pressure)
– disincrustation (deep cleansing of pores using galvanic current).
During the procedure, superficial exfoliation of dead skin cells occurs, inflammatory elements (comedones) are removed, blood circulation and metabolic processes in the skin are stimulated, and this, in turn, leads to normalization of the sebaceous glands. Fat and dirt accumulated in the pores are softened and brought to the surface, where they can be easily removed.
An alternative to scrubs is chemical peels.
This is a procedure for removing the surface layers of the skin epithelium using weak acid solutions for the purpose of rejuvenation.
Acids ensure uniform exfoliation of several layers of dead cells, which promotes skin rejuvenation, reduces oiliness, stimulates the synthesis of collagen and elastin, and leads to the formation of young cells. As a result of this stimulation, skin tone and elasticity increase.
Currently, chemical peeling uses glycolic and trichloroacetic acids, as well as fruit (alpha hydroxy acids). Phenol is used for deep peeling, but its use is limited due to the high risk of scarring.
After chemical peeling, it is necessary to use moisturizing creams that will eliminate the feeling of tightness and prevent fluid loss. The crusts that appear after peeling cannot be removed; they must be lubricated with cream,
Most often, a combination of procedures is the most effective; in this case, an individual complex will be created for you. At the end of the procedures, the specialist is obliged to once again diagnose the condition of the facial skin and recommend how to maintain the achieved effect.
Source: https://beauty.wild-mistress.ru/wm/beauty.nsf/publicall/2008-09-14-906447.html
Help from a cosmetologist
Dry skin is not a reason to panic. If your face begins to peel a little, you should buy a good moisturizer or use a pharmacy product (the most popular ones will be described below). But if your face peels off in patches or there is severe irritation, it makes sense to seek help from a professional cosmetologist.
A cosmetologist will help you get rid of peeling in a few procedures.
Peeling is another technique that will remove unsightly flaky spots. This procedure using laser or fruit acids can be carried out in any salon. The cost of a session ranges from 500 to 2000 rubles. After cleansing, the specialist will definitely prescribe a product to additionally moisturize the skin.
Biorevitalization is a procedure that allows you to solve the problem if your face is peeling in spots. A special medicinal drug is injected precisely into those areas where the skin is most irritated. Exfoliation occurs gradually. Sometimes you have to perform several procedures. Additionally, the cosmetologist also prescribes moisturizers.
Appearance from photo
Externally, oily facial seborrhea is characterized by the following manifestations:
- acne;
- comedones;
- milia;
- scars on the skin as a result of acne;
- increased oiliness of hair and skin.
With the dry type of the disease, dry skin, cracks, peeling and scales appear. The hair of patients with dry seborrhea is brittle, and the head is covered with fine dandruff. Dry seborrhea is more common in children.
Mixed seborrheic dermatitis is easily confused with the manifestation of atopic dermatitis, psoriasis, and lichen. Therefore, to clarify the diagnosis, a doctor’s examination is necessary.
Hives
Doctors of various specialties, including endocrinologists, encounter pathological changes in the skin. Skin lesions can be either an accidental finding or the main complaint of the patient. Skin changes that appear harmless at first glance may be the only sign of a serious illness. The skin is the most accessible organ for research and at the same time a source of the most important information. Skin lesions can clarify the diagnosis in many internal diseases, including diabetes mellitus (DM). Skin changes in diabetes are quite common. Severe metabolic disorders underlying the pathogenesis of diabetes lead to changes in almost all organs and tissues, including the skin [30]. Some diabetes-associated skin symptoms are a direct result of metabolic changes such as hyperglycemia and hyperlipidemia [4, 7].
If you have never had this disease, you have probably heard about it.
Treatment of seborrhea on the face
The standard therapeutic regimen for the treatment of seborrheic dermatitis includes:
- means to enhance the body's immune function;
- multivitamin complexes;
- external agents (creams and ointments);
- sedatives;
- physiotherapy (ozone therapy, cryotherapy, Darsonval microcurrents, UV and gamma radiation).
Among the variety of external remedies for the treatment of oily and dry seborrhea on the face, the following creams and ointments are popular:
- Flucinar is an antiseptic that relieves itching and redness of the skin;
- Advantan is an effective hormonal remedy against itching and inflammation;
- Skin cap. The ointment is based on zinc, which eliminates allergic rashes, reduces itching and irritation;
- Belosalik (Russian analogue of Akriderm). Effective in the treatment of dry seborrheic dermatitis.
Ketoconazole, Lamisil, sulfur-salicylic and naphthalene ointments are also used for medicinal purposes.
An acute inflammatory reaction with seborrhea on the face requires rapid relief of unpleasant symptoms, so the course of treatment includes:
- antiallergic drugs, such as Loratadine;
- NSAIDs, such as Indomethacin;
- corticosteroids such as Dexamethasone and Akriderm;
- in some cases - antibiotics.
Complete elimination of the disease is possible only with comprehensive treatment and adherence to a gentle diet. At the discretion and with the permission of the attending physician, therapy is supplemented with traditional medicine and physiotherapy (after the symptoms have subsided).
Traditional recipes for the treatment of seborrhea on the face and scalp are designed to normalize the secretory function of the sebaceous glands and restore the epithelium. The main components are often the following herbs:
- series;
- plantain;
- chamomile;
- St. John's wort;
- nettle;
- burdock;
- sea buckthorn;
- viburnum.
Also used in home remedies are sea salt, castor oil, kefir, whey, and apple cider vinegar. Here are a few recipes:
- Gauze wipes are moistened in whey and applied to the affected areas for 1 hour twice a day. After the procedure, the face is thoroughly washed. Kefir is used in the same way;
- Every morning, wipe the skin with the following mixture: add 150 g of vermouth and 100 g of crushed horseradish root to 300 g of vinegar. The infusion is kept for a week and stored in a cool place;
- Based on the above herbs, infusions are made at the rate of one tablespoon per glass of boiling water. Rinse hair with infusion or use it as a tonic and facial compress;
- Make a mask from one fresh cucumber and a tablespoon of honey. The mixture is kept on the face for 10-15 minutes, after which it is washed off;
- Sea salt is used as a scrub, which is used to massage the scalp and face. In this way, it is possible to gently exfoliate dead skin and “dry” excess sebum.
Home remedies cannot replace basic treatment, and independent “therapy” provokes the development of complications. Therefore, the use of traditional recipes must be agreed with a doctor.
What to do if an orange peel forms on your face
Most often, women experience complexes about their face, because it is considered a calling card. And these complexes concern not so much the shape of the eyes or the thickness of the eyebrows, but rashes on the skin.
One of the most significant problems for many women is facial skin like an orange peel. Why does this problem appear and what can be done at home to get rid of it?
Why does orange peel form on the face?
It will not be possible to understand immediately why tubercles, irregularities, or crusts appear on the skin.
A person’s face is always open, and the skin is constantly exposed to various external factors: weather, harmful effects of cosmetics, pollution, etc. If it has become lumpy, then the reason should be sought in your lifestyle and factors such as:
- sudden climate change. Sometimes this problem manifests itself in people who have changed their place of residence, city, or gone on a business trip or vacation;
- constant use of inappropriate cosmetics;
- eating unhealthy foods or eating irregularly;
- frequent and prolonged stay in places with high air humidity;
- hormonal disbalance;
- constant use of foundations that clog pores;
- frequent exposure to the open sun, as well as exposure to strong wind and dust on the skin of the face;
- presence of bad habits;
- constant stress, worries;
- reluctance to remove makeup before bed;
- increased work of the sebaceous glands and, as a result, the production of large amounts of sebum;
- hereditary factor.
Many of these factors contribute to pollution and clogging of pores on the face, and therefore inflammation, rashes and orange peel appear on the skin.
How to get rid of orange peel?
Of course, if your budget allows, you should go to a beauty salon and use such effective procedures as deep peeling or laser facial resurfacing.
However, some cosmetologists believe that home remedies are not only not inferior in quality, but are often more effective than salon procedures. At the same time, everyone can afford such funds - you don’t have to spend serious money.
How to remove orange peel from facial skin? We offer several effective recipes:
- Pour a tablespoon of linden flowers into 100 milliliters of hot water. Don't use boiling water - just hot water! Place the mixture on the stove and wait until it thickens. When this happens, allow the mass to cool, and then safely apply it to the skin. After 20 minutes, remove the mask with a cotton pad, then carefully wash with cool running water. It is important not to rub your face while washing.
- Buy bread made from black flour and soak a small amount of it in plain water. Apply the mixture for 15 minutes, after which you can rinse with cool water.
- Crush the pulp of one orange with a spoon and apply this mixture to your face. Lie with it for about 15 minutes, rinse with water, and then use a moisturizer.
- Take a not very large grater and grate one raw potato. Add one egg to the mixture, mix everything and apply to the skin of the face. After 30 minutes, the mask can be washed off.
- A paste of fresh tomatoes will also help tighten your pores if you apply it for about half an hour.
- Another version of the above mask with tomatoes. It stays on the face for the same amount of time, but only the tomatoes are cut into rings.
- If you have oatmeal at home, you can use it to cleanse your pores of impurities. Simply soften the flakes in water and apply to problem areas for 20 minutes. Washing with oatmeal is also useful.
- You can use coffee grounds as a scrub. It must be applied to the skin, gently rubbed over the face, then rinsed off.
- To tighten the pores, lemon zest, grated and mixed with olive oil, is also suitable. However, this recipe is not suitable for everyone. If irritation occurs after applying the mask, it is better to discard it and use another product.
Prevention
There is currently no orange peel on your face, but are you afraid of its appearance in the future? Then you need to take skin care measures:
- reconsider your lifestyle. Lack of sleep, poor diet, stress and anxiety clearly do not contribute to improving the condition of facial skin. In addition, it is important to be attentive to your health in general and to treat diseases in a timely manner, if any. It is also advisable to play sports or at least do exercises;
- Always cleanse your skin before going to bed, both makeup and dirt. A cleansing gel is perfect for this purpose;
- Don’t forget to clean your pores using suitable cosmetics and home recipes. It is recommended to pay special attention to products that contain medicinal herbs;
- make not only cleansing, but also nourishing and moisturizing masks, but try not to overdo it (this also applies to other cosmetics), otherwise the consequences will be even worse;
- Be sure to moisturize your skin, even oily and combination skin. By the way, the combined one needs this most of all;
- to get rid of dead skin cells, steam it once a week or two and clean it with a scrub;
- Once every 7 days it is recommended to use a tightening mask to restore elasticity to the skin.
This problem is much better preventable, but it is more difficult to treat. If orange peel does appear on your facial skin, you should start treatment immediately.
In order for all of the recommendations listed to really help and be effective, it is recommended not only to do home treatment, but also to visit a cosmetologist.
Treatment by a specialist will not take too much time, but the skin will become noticeably better and more beautiful.
If we talk about home care methods, it will be possible to get rid of bumps, bumps and pimples forever only if care procedures are carried out regularly.
Now you know what to do if the skin on your face turns like an orange peel. But as soon as you stop caring for her, you return to your old, incorrect lifestyle, and the previous cosmetic defects will return. With age, of course, changes are inevitable, but you have the power to minimize them.
Kartash Christina
(2 5,00 of 5) Loading...
Source: https://kladovaia-krasoti.ru/chto-delat-esli-obrazovalas-apelsinovaya-korka-na-lice/
Pharmacy drugs
If peeling skin is a consequence of any disease, you cannot do without medical attention. First of all, it is necessary to treat the illness that caused the deterioration of the facial condition. If the problem arose due to allergies, antihistamines such as Diazolin, Loratadine, Cetirizine will come to the rescue.
Fungal or bacterial skin infections may also be accompanied by peeling. Treatment should be carried out using special ointments. Only a dermatologist can prescribe the drug. You can hear a lot of good reviews about Diflucan and Exoderil.
In some cases, you cannot do without pharmaceuticals
Any creams that contain hydrocortisone (about 0.5%) perfectly eliminate peeling and irritation of the skin. It is worth considering that the epidermis can get used to this kind of drugs. Therefore, they must be used once a day for no more than two weeks.
Panthenol is a good product that not only moisturizes the skin, but also eliminates irritation. Dexpanthenol can be used against peeling, as an adjunct even for fungal infections or hormonal imbalances. To treat irritation in children, you can use Bepanten cream. The product copes well with various problems of children's skin, eliminates flaky spots and redness.
Diet
The condition of the skin directly depends on the diet. Therefore, another step on the path to recovery is to follow a diet plan that includes:
- refusal of “fast” carbohydrates;
- minimizing salted, smoked, fried foods in the diet;
- refusal of spices, spices, alcohol.
For seborrheic dermatitis, emphasis is placed on the use of:
- dairy and fermented milk products;
- soups;
- vegetables;
- steamed fish, lean meat;
- foods rich in fiber;
- rye bread.
Doctors also recommend eating small meals and having “fasting” days once a week. "Fasting" does not mean fasting. As an alternative, mono-diets, “unloading” on kefir, fruits or vegetables, are recommended.
It is very important to follow a hypoallergenic diet even after facial seborrhea has been cured.
What kind of disease is this?
Seborrhea occurs when the sebaceous glands malfunction. They produce a secretion that removes toxins, but at the same time a water-fat layer is formed, which is necessary to protect against drying out.
With seborrhea, the quantity and quality of the secretion produced changes, which causes disturbances in the microflora of the skin. Its protective functions weaken, creating a favorable environment for infections and inflammation.
The areas where the problem is concentrated are called seborrheic zones. Most often this is the face, scalp, shoulders, back and chest.
Skin of the head
The scalp is abundantly supplied with sebaceous glands, which produce sebum. It, in turn, performs the most important function - it protects cells from negative external influences.
Sometimes the amount of sebum secreted exceeds the norm, which initiates blockage of the sebaceous glands. After a while, an inflammatory process occurs and, as a result, the head becomes crusty and itchy.
Symptoms of skin structure disorders:
Seborrhea
- unbearable itching, constant scratching of the head in different areas;
- the appearance of dandruff - white scaly formations at the hair root, ranging in size from 1-2 mm to 15 mm, falling onto the ears and shoulders;
- hyperemia and scratching in areas of itching;
- purulent wounds - the addition of a bacterial infection.
Other causes of scalp crust formation are dermatitis, seborrhea, fungal and autoimmune diseases - psoriasis. The skin becomes covered with white scales resembling dandruff. They itch a lot and when peeled, a drop of blood is released.
Peeling skin in men, women and children
A child's skin reacts more vividly to certain irritants. This is due to decreased functioning of the immune system. A sharp change in temperature, sweets, citrus fruits, cosmetics - all this can lead to peeling of the baby's skin. The problem can be eliminated only by identifying its source.
If we consider women and men, the latter are much less likely to suffer from peeling skin. The epidermis of the stronger sex is more resilient, as it is more often susceptible to various types of irritants. In addition, men practically do not use cosmetics. Therefore, the likelihood of an allergic reaction is minimized.
Representatives of the fairer sex often experiment with cosmetics. It is not always possible to predict how the epidermis will react to a new product.
Women strive to prolong their youth and maintain a beautiful figure. Lack of vitamins due to various diets, the use of untested cosmetics, natural lack of moisture - all these are factors that do not work in favor of healthy skin. Proper care will help solve the problem.
Diet for scaly eczema
The need for proper nutrition for these skin diseases can hardly be overestimated.
- It is advisable to practically exclude from your diet: canned food (any kind), sweets, semi-finished products, spicy, smoked, fatty and fried foods, eggs. Alcoholic drinks, oranges, tangerines, etc., tomatoes, fatty meats, flour, are also not welcome.
- Vegetable soups, kefir, fermented baked milk, cottage cheese, porridge, turkey, chicken breast, rabbit will be very useful. If you eat millet porridge at least every week, you can save yourself from this disease.
- Eat sauerkraut in any quantity, drink dried fruit compote, and replenish calcium deficiency with eggshells.
- Drink more water, eat salads with carrots, baked apples.
- If there is no allergic reaction, eat vegetables, especially beets, beans, lettuce, fresh cucumbers, dill, parsley, celery.
Eczema can be treated if the patient makes efforts in combination: diet, medications and ointments or creams.
We wish you good health!
The condition of your facial skin directly signals health problems. And you shouldn’t mistakenly believe that a crust on your face is just a consequence of weathering, frost or heat. There are many more factors that lead to excessive peeling of the skin, the appearance of growths, and inflammatory spots. A frivolous attitude can lead to the formation of cracks and bleeding areas, which will be impossible to combat with ordinary cosmetics. The problem requires adequate medical intervention and examination of the whole body.
Getting rid of crust on the face
Classification
Experts in the field of dermatology usually identify several options for the course of such a pathological condition. Thus there is:
- liquid oily seborrhea - in such situations, the skin or hair looks excessively greasy and acquires a specific oily tint;
- thick oily seborrhea – characterized by profuse hair loss and intense formation of acne on the face. A distinctive feature is that if you apply a dry cloth to the affected area, after a few minutes it will absorb sebum secretions.
Skin crusted over
Human skin is quite sensitive to external irritants.
And if the skin suddenly becomes rough (covered with a crust), then perhaps the reason is too dry air or an allergic reaction to household chemicals, for example, powder, dishwashing detergent, soap, shower gel. This is possible even if you have already used these products before. However, a more serious scenario cannot be ruled out - contact dermatitis or psoriasis.
If the crust that appears on the skin does not go away within a few days, then you should urgently visit a dermatologist. He will take all the necessary tests and prescribe the correct treatment.
In cases where the crust appears due to external irritants, you can try to deal with it yourself - buy a special cream that has a softening effect and relieves irritation, and lubricate the affected areas with it. It is desirable that it be fragrance-free.
If the itching is unbearable, then antiallergic drugs will help. It is enough to take them for several days to cope with allergens. True, in order for treatment to be effective, it is necessary to identify and eliminate contact with the source of the allergy.
Diagnostics
First of all, the doctor collects an anamnesis. Then the risk factor for developing the disease, nervous disorders, genetic predisposition, living and working conditions are determined.
Laboratory tests are prescribed:
- Biochemical blood test, which allows you to determine the functioning of internal organs, liver, pancreas, biliary tract, and obtain an informative assessment of the metabolism of proteins, lipids, and carbohydrates. Cost of analysis: from 2 thousand rubles.
- A hormonal blood test to evaluate the functioning of the thyroid gland. The cost of the study is from 3 thousand rubles.
- Trichogram, with its help the condition of hair and skin is assessed. The cost of the procedure is from 3 thousand rubles.
- Ultrasound of the thyroid gland, gastrointestinal tract (if necessary). Cost from 2 thousand rubles.
How to diagnose the disease?
To make a diagnosis, you should make an appointment with a dermatologist. Based on an external examination, as well as special examination methods, a specialist will determine the form and severity of the disease and prescribe comprehensive treatment.
Additional diagnostic methods include:
- Biochemical analysis, as well as determination of hormone levels in the blood.
- Ultrasound examination to detect diseases of the ovaries, thyroid gland and adrenal glands.
- Consultation with related specialists such as a gastroenterologist, endocrinologist, gynecologist and trichologist.
Important!
It is imperative to carry out a differential diagnosis with psoriasis to exclude it.
- Possible complications in the absence of therapeutic therapy
- Possible complications in the absence of therapeutic therapy.
In the absence of proper treatment and in advanced forms, severe complications may occur. These include:
- Spread of the disease to the skin of the chest, back, armpits.
- Attachment of a secondary infection and development of inflammation.
- The formation of boils, carbuncles, and purulent abscesses requiring surgical treatment in a hospital.
Important!
The appearance of purulent foci in the area of the nasolabial triangle is especially dangerous, since any damage to the blood vessels in this area leads to infection in the meninges.