After surgery, patients often complain about the condition of the suture. Complications arise for various reasons. A hard lump on the stitch after surgery is the most common one. It is not always dangerous to health, and special treatment is usually not required. In order to identify the cause of the lump, you need to consult a doctor. Self-medication leads to the development of complications and the need for repeated surgery.
A dangerous symptom is the appearance of a lump on the suture, accompanied by the discharge of pus. This is a common occurrence and can be noticed upon self-examination of the area where the intervention was performed. Problems can arise for various reasons, including: improper suturing, bacterial infection, rejection of threads by the human body, use of low-quality materials. You should remember the importance of proper treatment of the surgical area, and if bumps, pain or suppuration occur, you should immediately consult a doctor.
Possible reasons for a wet seam
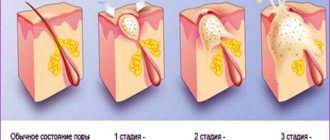
If you observe the postoperative wound, for the first few days it will be a little damp and even hot. The first few hours the suture may bleed. Then the blood coagulates and dries, but shiny droplets are still visible on the wound - transudate. This is a natural transparent moisture secreted by the serous membranes as a result of fluid filtration by blood vessels.
Over time, the serous fluid no longer flows so abundantly, because the condition of the tissue returns to normal. Otherwise, the amount of transudate may increase. This indicates the beginning of an inflammatory process, the causes of which are different.
- Incorrectly installed or removed drainage system too early.
- Low quality suture and dressing materials.
- Dressing under non-sterile conditions.
- The intervals between dressings are too long.
- Incorrectly chosen treatment tactics with antibiotics and local remedies.
- Reduced immunity of the patient.
The abundant secretion of serous fluid is a kind of protective reaction of tissues to the inflammatory reaction. But it turns out that the situation is only getting worse: a humid environment leads to the fact that the suture festers after the operation, i.e. inflammation develops more rapidly. Transudate is transformed into exudate - a liquid of inflammatory nature.
In addition to serous fluid, transparent or whitish ichor may ooze from the postoperative suture - this is lymph that is released from small capillaries. With the ichor flowing out of the wound, toxins and microbes are “washed out”, so this process is natural for the first few days. If it does not stop, then bloody discharge can also cause the wound to get wet and not heal for a long time.
Types of paraprosthetic infection
In orthopedics and traumatology, several classifications of SSI are used. Systematization and assignment of infection to a specific type helps doctors assess the severity of the patient’s condition. The Coventry-Fitzgerald-Tsukayama classification is the most common.
Table 1. Types of deep paraprosthetic infection according to Coventry-Fitzgerald-Tsukayama.
| Type | Development time | Treatment tactics | |
| I | Acute postoperative | 1st month | Revision of the postoperative wound, removal of necrotic tissue, and, if necessary, replacement of some parts of the endoprosthesis while maintaining its main components. |
| II | Late chronic | From 1 month to 1 year | Mandatory revision endoprosthetics. |
| III | Acute hematogenous | After 1 year | It is entirely justified to try to preserve the installed prosthesis. |
| IV | Positive intraoperative cultures | Asymptomatic bacterial colonization of the implant surface | Conservative treatment consisting of parenteral antibiotic therapy for 6 weeks. |
In the classification created by the Novosibirsk Research Institute of Traumatology and Orthopedics, SSIs are divided into early acute, late acute and chronic. The first develop within three months after endoprosthetics, the second - at 3-12 months, the third - after 1 year. Infectious complications can occur in a latent, fistulous, phlegmon-like or atypical form.
According to the prevalence, infections are epifascial (superficial) and subfascial (deep). May be accompanied by total, femoral or tibial instability.
Treatment of postoperative sutures
In most cases, the patient spends the first 7-10 days after surgery in the hospital, where his wound is regularly bandaged under the supervision of the attending physician. And if any problems are discovered, measures are taken immediately. The patient is discharged with the stitches removed and only the wound in normal condition. But literally the next day after discharge, the suture may begin to get wet and then fester.
The goals of treating a weeping suture after surgery are as follows: it is necessary to relieve inflammation by destroying pathogenic microflora, and also to dry the wound to avoid recurrence of suppuration. What to do, what measures to take, and what means to use?
Attention! If the suture gets wet and suppurates, you should go to the hospital! Self-medication is an extreme measure that you can resort to if you are unable to see a doctor.
Local remedies
External preparations will help cope with wetting and inflammation of the seam. In the case of a weeping wound, you need to use gels. They, unlike ointments and creams, do not leave a greasy film and allow the skin to breathe, which is very important for drying the wound. Solcoseryl is one of the most effective gels for postoperative wounds.
If the postoperative suture continues to get wet, you can also use powders. They also have a drying property because they absorb moisture while promoting healing. For example, Baneocin powder. It has a pronounced antimicrobial effect and is able to effectively heal weeping wounds.
The gel or powder should be applied to a clean wound, so it must be treated first. First, remove dead skin and dirt using hydrogen peroxide. Then blot the seam with a sterile napkin, drying it in this way, and only then apply the gel.
By the way! Wet wounds heal better in the open air. Therefore, the patient can apply bandages only at night or when leaving home.
There are cases when the suture bleeds for a long time after surgery. This also cannot be left like this, because bleeding indicates damaged blood vessels through which infection can enter the body. In this case, in addition to antibacterial and anti-inflammatory agents, you also need to use antiseptics. For example, brilliant green or Betadine (iodine solution).
Medicines
When the seam simply gets wet, it cannot be treated with pills. Another thing is the development of inflammation. Antibiotics may be needed here. What kind of drug it will be, as well as its dosage and duration of administration will be determined by the doctor. Usually these are broad-spectrum antibacterial drugs.
If the suture does not heal after surgery
It is necessary to resort to surgery in case of accumulation of exudate inside the wound. The formation of an abscess is indicated not only by the wetting of the suture and the unpleasant odor from it, but also by an increase in the patient’s temperature.
The operation to evacuate purulent contents is performed under local anesthesia (injection). This is a shallow opening of the abscess, probing it and installing drainage. If the excision was extensive, additional sutures are applied. In some cases, a sterile bandage is sufficient. After such an intervention, the patient remains in the hospital for a couple of days. He is prescribed rest, antibiotics and physiotherapy.
Lab tests
Taking tests helps identify acute and chronic inflammatory processes in the body. An increase in indicators is not a reliable sign of SSI. To make a diagnosis, it is necessary to take into account the presence of certain clinical symptoms, radiographic data and other research methods.
Clinically significant laboratory parameters:
- Leukocyte count. It is important in the diagnosis of acute paraprosthetic infection. A clear sign of inflammation is an increase in the total number of leukocytes and neutrophils, a shift in the leukocyte formula to the left.
- ESR. It is a non-specific indicator. A normal erythrocyte sedimentation rate indicates the absence of inflammatory processes, an increased rate indicates their presence.
- C-reactive protein. CRP is an acute phase protein and a highly sensitive marker of SSI in people who have undergone arthroplasty. When diagnosing paraprosthetic infections, you need to pay attention to this indicator.
Knee replacement in the Czech Republic: guarantees, prices, rehabilitation, reviews and statistics.
Find out more
Minimally invasive endoprosthetics in the Czech Republic: doctors, rehabilitation, terms and prices.
Find out more
How to avoid getting the seam wet
Preventing the postoperative suture from getting wet is easier than treating a festering wound later. Therefore, patients must take proper care of their sutures. The rules of care are elementary and logical, but for some reason some people still neglect them.
- Change the bandage according to the regimen prescribed by the doctor. Minimum – once a day. If bandages quickly become wet and leak, you should increase the frequency of dressings.
- Changing the dressing should be done with clean hands and without unauthorized persons or animals in the room.
- All dressings (bandages, plasters, cotton wool) must be sterile.
- The seam should not be subjected to mechanical stress: friction against clothing, scratching, picking.
- Do not wet postoperative wounds until they are completely healed.
- If there is any suspicion of pathology (the wound is oozing, the suture has changed color, has festered, become inflamed), you should consult a doctor.
A suture that gets wet after surgery is not only an unpleasant problem that spoils bed linen and clothing, but also a risk of complications in the form of ulcers and necrosis. This also extends the healing time and quality of the suture, which as a result can turn into an unsightly colloidal scar. Therefore, you need to properly care for postoperative wounds and consult a doctor on time.
Once your general condition has stabilized and you have been discharged from the hospital, you can process the stitches yourself. How to independently treat stitches after surgery at home?
The main stage, which requires careful adherence to the rules of asepsis and antiseptics, is processing.
Using a sterile bandage, properly treat the skin in the direction from the wound, at a distance of at least 2.5 cm, and only then apply a sterile bandage.
You can use a bandage to secure it; it will prevent slipping and will hold the bandage securely. Stitches should be disinfected at home every day, at the same time.
Healing and removal of sutures, on what day?
It is almost impossible to make an accurate forecast and clearly formulate the healing time of postoperative sutures. How many days after sutures can be removed depends on many factors.
In different parts of the body, soft tissue regeneration occurs at different rates.
- During a caesarean section, the sutures can be removed on the 10th day.
- For amputation - on the 12th day.
- For operations on the abdomen and abdominal organs - on the 7-8th day.
- For operations on the chest organs - after 14-16 days.
- For facial surgeries – after 7 days.
If the incision site itches, this indicates normal healing by primary tension of the wound.
Normally, after the edges of the wound have fused, the threads are easy to remove, but if you ignore the timing of removal, inflammation and redness of the scar will begin.
Often, when trying to remove stitches yourself, part of the thread remains in the wound. Upon examination, it is easy to see the place where the thread sticks out, going into the soft tissue.
The consequences of such self-medication are a fistula at the suture through which infection occurs. Pathogenic organisms freely enter the body cavity, a significant thickening of the scar is noticeable, and an unpleasant odor appears from the wound.
Prosthetic joint infections
In pathology, inflammation spreads to the cavities and membranes of the operated joint, remnants of the synovial membrane, bones at the site of fixation of the endoprosthesis and adjacent soft tissues. The cause of the complication is the colonization of joint surfaces by pathogenic microflora. Bacteria can come from the external environment or be introduced hematogenously.
This is what an infection looks like on an x-ray.
Prosthetic joint infections are the most serious complication among all SSIs. They do not respond to conservative therapy, so they have to be treated surgically. Doctors replace the endoprosthesis, but sometimes they still manage to save it.
There are three methods for treating infections of a prosthetic joint: wound revision without removing the implant, one-stage revision and two-stage endoprosthetics. The choice of technique depends on the patient’s condition, the time of manifestation of the infection, the stability of the prosthetic components and the nature of the pathogenic microflora.
What to do if the seam comes apart?
Sutures after surgery come apart quite rarely, this is largely due to the severe current illness, but there are other reasons:
- If the reason for the operation was purulent diseases - purulent cholecystitis, peritonitis.
- Incorrect management of the postoperative period - early physical activity, injury to the postoperative suture.
- The stitches are too tight.
- Low muscle tone, excess weight, tumors.
If internal organs and subcutaneous fatty tissue are visible at the site of the broken suture, then immediate hospitalization is indicated.
If the edges of the wound are partially separated, and when pressure is applied, serous fluid or pus oozes from it, then you can turn to the surgeon who performed the operation for help.
Important! If the edge of the wound has split open, you should never disinfect the damage yourself!
When alcohol, iodine solution or brilliant green gets into the wound cavity, tissue necrosis develops, which complicates treatment and can lead to sepsis.
Further treatment tactics will be based on the results of blood tests, bacteriological culture of the wound contents, and diagnosis using ultrasound or CT will provide information about the condition of the internal organs.
Microbiological studies
Bacterioscopic and bacteriological studies make it possible to identify and identify the causative agent of infection, as well as determine its sensitivity to antibiotics. Quantitative studies make it possible to determine the number of microbial bodies in purulent discharge.
The following materials can be used for research:
- discharge from a wound;
- fabric samples;
- fluid from the joint cavity;
- prosthetic material.
In case of implant-associated infection, it is almost impossible to detect bacteria in biological fluids and tissues. Pathogenic microorganisms are found on the surfaces of endoprostheses themselves. They cover the implants in the form of an adhesive film.
Fact! In addition to bacteriological examination, PCR (polymerase chain reaction) can be used for diagnosis. The method has high sensitivity but low specificity. Because of this, it often gives false positive results.
Home remedies
In the postoperative period, when the patient’s condition is completely stabilized and there are no complications, further care and treatment are carried out at home.
If the area sutured after surgery becomes wet, it is better to carry out the treatment twice a day, noting the condition of the scar.
If there is suppuration under the suture, then under the supervision of a surgeon, blockade of the wound with a 0.25-0.5% novocaine solution with antibiotics is indicated, and in addition, drugs that resolve the pus are prescribed.
If an allergy appears to any of the components of the ointment, treatment is carried out with cleansers for sensitive skin.
Folk remedies that promote healing and smoothing of scars can be used after the approval of a doctor.
A simple ointment to help scars heal faster: 5 g. calendula cream, 1 drop each of orange and rosemary oil.
The ointment gently dissolves the scar, and the oils in the composition are responsible for the gradual lightening of the scar area. After six months, the place where the old scar formed will almost match the color of the skin.
Seam drainage
Drainage is installed in a postoperative wound in order to speed up healing by removing blood clots, lymph, and pus from it.
Typically, wound drainage is indicated for no more than 3-4 days. This term is enough for the wound to cleanse and heal by secondary intention.
Author: doctor Iordanskaya A.V.
Local complications in the area of a postoperative wound are not so rare, but fortunately, for the most part, they occur without serious consequences. Often there is pain and redness in the area of the postoperative suture. Following them, discharges of a varied nature may appear from the sutured wound: purulent, bloody, sanguineous, etc., which indicates the development of complications of an inflammatory nature, such as suppuration of the sutures and their possible divergence.
Why do the seams become inflamed?
There are several main reasons for the development of the inflammatory process: - infection in the wound; — improper drainage of the wound after surgery in obese patients; — injury to subcutaneous fat during surgery, leading to the formation of hematomas and areas of tissue necrosis (necrosis); - use of materials with high tissue reactivity (sensitivity) for a seam made on a layer of subcutaneous fatty tissue; The above reasons may be involved in the development of inflammatory complications individually or in combination with each other.
Symptoms of the development of inflammatory infiltration in the area of the postoperative suture appear 3-6 days after surgery and are as follows: - an increase in suture pain over time; - redness and swelling appear around the wound (looks like swelling); - after some time, discharge appears from the wound (purulent or bloody, and may have an unpleasant odor); — gradually, due to increasing intoxication, the general condition of the body worsens, which is manifested by increased body temperature, muscle aches, general weakness, etc.;
If the above signs appear, you should not self-medicate, since only a doctor, knowing the nature of the operation and the suture applied, what materials were used for this and how the healing process proceeded, as well as taking into account the general condition of the person, will be able to select a treatment appropriate to the severity of the process. If the development of inflammatory infiltration is detected in a timely manner, it can be treated using physiotherapy (UHF, ultraviolet irradiation, etc.). If purulent inflammation is detected in the postoperative area, urgent cleansing of the wound is required, which in some cases may require removal of sutures. This is done in a stationary (hospital) setting, followed by the installation of drainage and antibiotic therapy. You need to understand how to properly treat sutures after surgery. If it is determined that the cause of suppuration of the suture is an anaerobic infection, surgeons excise (cut out) the tissue affected by the inflammation, prescribe antibiotic treatment and drain and clean the wound daily. When the inflammatory process subsides, secondary sutures are applied or limited to ointment dressings.
Wetting seams may not have anything to do with inflammation. In some cases, a so-called seroma develops in the postoperative area, which means a local accumulation of serous fluid. Its formation is due to the fact that during the operation the lymphatic capillaries are crossed, and the lymph flowing from them accumulates under the loose subcutaneous fat. The development of such a postoperative complication is more typical for obese people with excessively developed adipose tissue.
The resulting seroma externally manifests itself as the release of a straw-colored liquid from the postoperative wound. If the development of seroma is suspected, on the second or third day after surgery, serous discharge from the wound is evacuated once (less often twice), after which the formation of seroma ends.
The doctor in your maternity hospital is illiterate, I was forbidden to use it in the housing complex because... it contains Chloramphenicol Use during pregnancy and breastfeeding If taken orally, it passes into the breast milk of nursing women and may cause serious adverse reactions in breastfed children. When applied topically, systemic absorption is possible. In this regard, nursing women should stop either breastfeeding or using the drug.
Side effects of the substance Chloramphenicol Systemic effects From the gastrointestinal tract: dyspepsia, nausea, vomiting, diarrhea, irritation of the mucous membrane of the mouth and pharynx, dysbacteriosis. From the cardiovascular system and blood (hematopoiesis, hemostasis): leukopenia, thrombocytopenia, reticulocytopenia, hypohemoglobinemia, agranulocytosis, aplastic anemia. From the nervous system and sensory organs: psychomotor disorders, depression, impaired consciousness, delirium, optic neuritis, visual and auditory hallucinations, taste disturbance, decreased hearing and visual acuity, headache. Allergic reactions: skin rash, urticaria, angioedema. Other: dermatitis, secondary fungal infection, cardiovascular collapse (in children under 1 year). When applied to the skin and conjunctival use: local allergic reactions.
Well, if you drink this Chloramphenicol, then probably yes)) and diarrhea will attack and the mucous membrane of the mouth will be all irritated) and not only that. Smear yourself with brilliant green, madam. it will be calmer this way
p/s/ these, as you put it, illiterate doctors helped me and my child. none of the horror you cited above followed. everything healed well.
It’s well written here about the treatment of weeping wounds. And most importantly, keep an eye on it, sometimes it makes sense to add syntomycin ointment or levomekol in time, so that later you do not drink AB orally if the wound festers.
To treat a wound at home, you need to prepare in advance:
A clean oilcloth on which everything necessary for dressing will be laid out. Antiseptic for treating hands. Hand soap. Clean towel for hands. Alcohol-containing antiseptic for treating the skin around the wound (alcohol solution of iodine, brilliant green, calendula tincture or salicylic alcohol is quite suitable) Aqueous solution of antiseptic (solution furacillin, 3% hydrogen peroxide solution, miramistin) Tweezers and scissors treated with an alcohol antiseptic (they must be treated before and after each dressing) Medicine for wound treatment Sterile dressing material (bandage, gauze pads) Non-sterile clean dressing material for a fixing bandage.
Rules for dressing and treating wounds
Before starting the dressing, you must thoroughly wash your hands with soap and dry them with a clean towel. After this, lay out everything that is needed for dressing. Next step: remove the previously applied external bandage.
Then we wash our hands again or treat them with a disinfectant solution, or put on sterile gloves.
It's time to remove the tissue directly covering the wound from the wound. If the napkin sticks, moisten it with an aqueous antiseptic solution (in this case it is better to use a 3% hydrogen peroxide solution) and wait until the napkin gets wet. We remind you that you cannot tear off the napkin.
After removing the napkin, treat the skin around the wound with an alcohol-based antiseptic solution and inspect the wound without touching it.
The purpose of the examination is to assess the condition of the wound: is it dry or weeping (wet).
A wound with a wet, pink, easily injured surface and a significant amount of discharge is considered a weeping wound. If the surface of the wound is dry, with crusts and cracks, this wound is dry.
Also, with each dressing change, it is necessary to evaluate how the healing process is progressing. The following criteria will help assess the healing process: wound size (a healing wound, albeit slowly, but decreases in size), a dry or weeping wound (the transition from a weeping wound to a dry one indicates successful treatment of the wound), depth of the wound (with successful treatment, the wound becomes more and more and more superficial).
If upon examination you see that the amount of discharge from the wound has increased, or it has acquired a different smell (no matter whether it is unpleasant or even pleasant, for example, sweetish) and color (primarily yellow, greenish, gray). If the wound does not decrease in size, but, on the contrary, increases, especially if it deepens. If the pain in the wound increases every day or has sharply intensified. If there is a tugging and (or) throbbing pain in the wound area. If treatment of the wound does not produce any positive results. If there is swelling and redness of the skin around the wound. If the body temperature has increased, chills have appeared, and there are no other reasons for this condition. In all of the above cases, you should urgently show the wound to a surgeon!
After examination, the wound is washed with an aqueous antiseptic solution using sterile wipes. They are moistened with an antiseptic solution and the wound is carefully treated. Then the wound is dried with a dry sterile cloth.
The next step is to apply a wound healing agent. A very important point: ointments are used to treat dry wounds, and jelly or gels for weeping wounds. The difference is explained by the fact that a dry wound requires protection in the form of a film, under which it will soften. Ointment is not suitable for a weeping wound, as it will create an environment that will prevent the release of fluid and the entry of oxygen, which will slow down the healing of the wound. Therefore, jelly (gel) is applied to the weeping wound. Jelly (gel) will protect the wound from drying out and possible infection, and will not allow the wound to suffer from lack of oxygen.
So, we have decided on the form - we apply the required amount of medicine directly to the wound or to a napkin, but you cannot touch the wound or napkin with the tube. It is time to replace the gel wound treatment with ointment only when the wound begins to dry out.
Choosing the right drug to treat a wound
It's time to figure out which medicine can effectively treat wounds at different stages of healing. It is optimal when the active substance is universal and the same at all stages of wound treatment. The drug Solcoseryl has all these qualities. The drug was developed by Swiss scientists and is available in both jelly (gel) and ointment form, which is very convenient. Solcoseryl has a powerful wound-healing effect and is a universal wound-healing agent.
Important! When the wound is large, it may have both wet and dry areas, then Solcoseryl gel and ointment are used simultaneously for these areas, respectively. In such a situation, Solcoseryl is applied directly to the wound surface (not on a napkin) in order to accurately reach the desired area.
After applying Solcoseryl, the wound is covered with a sterile napkin, after which a fixing bandage is applied.
When the wound has healed so much that it is covered with thin young skin, a small amount of Solcoseryl ointment is applied to it and the protective bandage is no longer applied. If areas of young skin alternate with areas of a dry wound, the bandage is applied 20-30 minutes after dressing, giving the wound the opportunity to remain open. As the wound continues to heal, it is advisable to leave the wound open for a longer period of time.
© 2007-2013, Pharmpreparat LLC All rights to materials on the site are protected in accordance with the legislation of the Russian Federation. When using any resource materials, a direct link is required.
A drug for the treatment of difficult-to-heal sutures and postoperative wounds
Despite advances in surgical technology, the use of modern sterile materials and the skill of surgeons, there are frequent cases of complications from a postoperative wound, when the healing time is noticeably prolonged.
Why is this happening?
On the one hand, the reason for the difficult healing of a postoperative wound directly depends on the degree of its microbial contamination
. Thus, with “clean” wounds the number of complications reaches 1.5-7.0%, with conditionally “clean” wounds - 7.8-11.7%, with contaminated wounds (wounds that come into contact with organs contaminated with microbes) - 12.9 -17%, for “dirty” (purulent) wounds – more than 20%.
On the other hand, this is due to the general condition of the human body
who underwent surgery. Unfavorable factors include: age over 70 years; nutritional status (hypotrophy, malabsorption syndrome, obesity); concomitant infectious diseases; violation of anti-infective defense systems, including immune status (oncological process, radiation therapy, treatment with corticosteroids and immunosuppressants, parenteral nutrition); concomitant chronic diseases (diabetes, chronic inflammatory processes, circulatory failure, renal and liver dysfunction).
At the same time, natural (physiological) healing mechanisms are significantly reduced, reparative (restorative) processes are sharply inhibited
, a manifestation of which is
difficult healing of postoperative wounds and sutures
.
How to effectively help healing?
Of course, you can diligently engage in general strengthening and systemic therapy, thus affecting the entire body “as a whole.” And wait for months for normal physiology to be restored. But when it comes to chronically non-closing wounds, more effective means are needed.
Stellanin ® ointment
– a new generation drug for the treatment of wounds and sutures in patients who have undergone surgery:
- Eliminates infection, swelling and pain, prevents the synthesis of inflammatory mediators - prostaglandins, biologically active substances that initiate and maintain the inflammatory process. As a result, even extensive inflammation stops very quickly
. - Activates vascular growth factors vegf-A and vegf-B. Newly arriving cells are specialized into tissue cells, which leads to restoration of the structure
of the lowest basal (germ) layer of the skin, damaged during surgery.
To solve the whole complex of accumulated problems, together with scientists from the Russian Academy of Sciences and the Institute of Surgery named after. Vishnevsky (Moscow) developed an innovative approach
to the treatment of long-term non-healing wounds, which is implemented in original preparations:
Stellanin ointment
and
Stellanin-PEG ointment
. To create them, some of the best specialists in the country were involved and the latest achievements of molecular biology were used.
The active ingredient of Stellanin-containing ointments is the substance Stellanin (1,3-diethylbenzimidazolium triiodide). Stellanin is a complex chemical compound - organic
part of the molecule affects the activity of the cell’s gene apparatus, powerfully activating regeneration processes in it.
At the same time the inorganic
part of the molecule has a pronounced effect on the entire spectrum of pathogenic microorganisms.
Stellanine is the only one
from wound healing agents that directly activate previously
SUPPRESSED
regeneration processes.
It
increases the number of fibroblasts in the wound - the main cells involved in the restoration of damaged skin - 7.5 times
It is especially important that all pathogens
wound infections
have neither
natural nor acquired resistance to Stellanin.
In the presence of pus, thanks to the excipient (polyethylene glycol) included in the Stellanin-PEG ointment, the wound is quickly cleared of purulent
content. At the same time, inflammation is blocked, pain and swelling are eliminated.
«Already on the first day
Treatment of wounds with Stellanin-PEG ointment shows positive dynamics in the healing process, and inflammation decreases.
Young cells with a high level of metabolic processes appear in the wound.” ( From the Report approved by the Director of the A.V. Vishnevsky Institute of Surgery, Academician of the Russian Academy of Medical Sciences V.D. Fedorov).
How to treat a wet seam after surgery – Health Savior
Wounds
Each surgical intervention ends with suturing the surgical incision with special threads. Wound care after removal of sutures should be carried out under aseptic conditions with antibacterial ointments and antiseptic agents.
On what day are the stitches removed from the wound?
During surgery, the integrity of healthy tissue is damaged. At the end of the operation, the edges of the abrasion are connected with surgical sutures and staples, the care of which must be careful.
There are three types of defect closure:
- The primary one is applied after the operation is completed.
- Secondary - closed after cleansing the granulating wound.
- Provisional - applied temporarily during surgery, removed at the end of the operation.
The day the sutures are removed depends on the following factors:
- on the type of complexity of the operation;
- postoperative wound length;
- development of complications;
- on the rate of soft tissue regeneration;
- from leaving.
Sutures are removed on a certain day:
- After a cesarean section, the staples and threads are removed on the 10th day.
- After amputation of limbs, they wait 12-14 days.
- During surgical interventions on the abdominal organs (stomach), the sutures are opened a week after the operation.
- On the chest they are removed after 2 weeks.
- On the face, regenerative processes occur faster. The procedure is carried out after 5-7 days.
Stages and factors of healing of postoperative sutures
Healing of the wound area is determined by the following factors:
- The patient's age affects the speed of reparative processes.
- The patient's weight affects the reparative capabilities of soft tissues. The presence of excess fatty tissue prolongs the process of healing of the skin defect. Normally, with proper care, adipose tissue receives a poor blood supply, which reduces the rate of healing. Obese people have a high risk of infection in the postoperative area due to the increased susceptibility of lipocytes to pathogenic microorganisms.
- Hypovitaminosis and poor nutrition reduce metabolism within damaged tissues. The flow of energy and plastic material into the tissues is disrupted, which negatively affects the reparative functions of the skin.
- After surgery, you must follow the established drinking regime. Dehydration leads to insufficient fluid flow into the cells.
- The postoperative area, enriched with blood vessels, heals faster due to the constant supply of nutrients.
- Normal functioning of the immune system contributes to the healing of a postoperative wound without the development of negative consequences. Immunodeficiencies suppress reparative processes within epithelial cells.
- Chemotherapy, X-ray irradiation, and long-term use of hormonal drugs have a negative effect on the condition of the sutures.
- Diabetes mellitus disrupts metabolism and care can be painful. To increase reparative processes, you need to keep sugar under control and smear the pathological area with special products.
- The addition of a bacterial infection reduces the protective function of the skin.
- The condition of the scratch is negatively affected by hypoxemia, low blood pressure, ischemic damage to injured tissue, and cardiovascular diseases.
- The use of anti-inflammatory drugs in the early stages helps to suppress the reparative functions of the skin and mucous membranes. Application 12-14 days after removal of the suture has the opposite effect.
- Insufficient oxygen supply into tissues slows down the synthesis of collagen, which is involved in wound healing.
They heal in several stages:
- Microphages immediately react when the integrity of the skin is violated. Fibroblasts migrate to the injured area, which is formed by cut, sutured tissue.
- Fibroblasts connect to fibrillar structures using fibronectin. The reaction provokes active synthesis of collagen, the fibers of which cover the resulting defect.
- A scar forms at the site of the wound. Its strength depends on the amount of collagen. Young patients heal faster than older people.
- Epithelial cells begin to migrate from the periphery to the central part. The new epithelium acts as a barrier to the penetration of pathogenic microorganisms. Fresh, large scars have poor resistance to infectious agents. Epithelial cells cannot cover the entire postoperative area; careful care is required. A skin graft is required. The last stage of healing of wound surfaces is tightening of the edges. The skin is restored.
Seam treatment products
Treatment of sutures after removal should be carried out under aseptic conditions with selected preparations. Medicines must be selected according to the type and condition of the wound, its length, the presence of complications, and the type of care for it. Postoperative patients are advised to consult a doctor about choosing a drug in order to get the most effective results from treatment in a short time.
The drug must have a regenerative, antiseptic, antimicrobial, reparative effect.
It is better to choose drugs from the group of drying ointments to prevent the development of a weeping wound.
For processing, solutions, creams, gels, and powders are used. The therapy combines several types of care and medications to achieve the fastest results.
Solutions
- Hydrogen peroxide has an antiseptic effect on the damaged area after removal.
Upon contact with the skin, active oxygen is released. The solution has a short-term antimicrobial effect. The product is used 2-3 times a day. - When leaving, treatment is carried out with boric acid. The medicine is used twice a day.
- The seams can be wetted. After the water procedure, it is advisable to smear the wound defect daily with brilliant green to reduce the risk of infection.
Ointments, creams, gels
- Levomekol is a drug that has an anti-inflammatory and antibacterial effect. Helps restore the integrity of the skin after removal and discharge. Levomekol is recommended to be applied twice a day.
- Povidone-iodine promotes healing, prevents the development of inflammation and suppuration. The medicine is applied for half an hour, then washed off with warm water. Careful care with this medication is not required.
- Bepanten cream normalizes metabolism within tissues. Suppresses the formation and release of pathogenic fluid. The cream is applied 2-3 times a day.
- Eplan promotes healing of postoperative wounds in a short time.
The cream anesthetizes the pathological area and prevents the growth of bacteria inside the postoperative area.
Daily wound care after stitches
After the scar is removed, it is necessary to continue to care for the postoperative area. Proper care and following the doctor’s recommendations will help avoid unpleasant complications. Treatment of the wound after removal of the sutures should be carried out according to the following algorithm:
- Buy the necessary materials for dressing at the pharmacy: bandage, potassium permanganate, brilliant green, hydrogen peroxide, plaster.
- Before treatment, carefully inspect the postoperative area. Pathological contents in the form of pus, ichor, and blood should not be released.
- Before carrying out the manipulation, wash your hands with soap. You need to wash up to the elbow.
- Treat your hands with disinfectants.
- Remove the bandage.
- The skin around the postoperative scar can be periodically lubricated with brilliant green and iodine.
- Ointments are applied to the surface of the damaged area, which accelerate the reparative processes.
- Doctors allow you to wet the wound after removing the stitches. It is important to lubricate the pathological area with hydrogen peroxide after water procedures. The solution should be applied with a cotton pad or swab.
- After care, the abrasion can be left open or an aseptic bandage applied to it. Secure the top with adhesive tape.