Dermatoses and infectious diseases
A rash during pregnancy may be associated with diseases such as atopic dermatitis, cholestasis (also characteristic of the gestational period), polymorphic dermatosis, pephigoid (a type of herpes).
It happens that before pregnancy a woman was not bothered by allergies or other skin diseases. But more often than not, there was still a predisposition to them (about every fifth patient with atopic dermatosis had signs of this pathology before).
In general, I diagnose dermatoses in pregnant women in approximately 3-5% of women, but it should be noted that with a mild course of the disease, not every expectant mother consults a doctor, so it is quite difficult to establish the true extent.
A rash on the abdomen during pregnancy most often appears in those women who have a hereditary predisposition to such diseases, including autoimmune pathologies and allergic reactions. Fortunately, after giving birth it goes away quite quickly.
It happens that a rash indicates infectious pathologies such as measles or rubella. In this case, additional symptoms characteristic of viral infections arise, from which the nature of the disease can be understood.
Causes and risk factors
All etiological factors that can be triggers of inflammation of the skin are conditionally divided into 2 groups: endogenous (internal) and exogenous (external).
Dermatoses are accompanied by significant subjective sensations, cosmetic defects, limit the patient’s activity and negatively affect the quality of life.
The most common external causes:
- physical factors of influence (mechanical friction, systematic or one-time extreme temperature effects, ultraviolet or ionizing radiation, exposure to electric current, injuries);
- chemicals that can cause disease both through direct contact with the skin and when ingested (aggressive household chemicals, cosmetics, industrial hazards, allergens, medicines, food, etc.);
- biological (bacteria, viruses, protozoa, arthropods, fungi, etc.).
Dermatosis may be caused by skin contact with household chemicals
Usually, for the development of dermatosis, a combination of several factors is necessary: the presence of a provocateur, weakening of local skin protection, failure of the immune response to aggressive influence, etc. However, sometimes even an isolated exposure can provoke a skin disease (for example, a burn or frostbite).
Internal reasons:
- local chronic focus of infection (chronic tonsillitis, pyelonephritis, carious teeth, etc.);
- chronic diseases of internal organs that neutralize and eliminate toxins (for example, erythema of the feet and palms due to liver disease);
- disorders of protein, mineral, carbohydrate metabolism;
- regional blood flow disorders, local microcirculation defects;
- hypovitaminosis;
- lymphatic drainage disorders;
- diseases of the nervous system (both central and peripheral) or functional disorders;
- endocrine pathology;
- metastasis to the skin in malignant neoplasms;
- diseases of the hematopoietic system;
- genetic defect, hereditary predisposition;
- immunosuppression.
Sometimes the cause of dermatosis remains unclear, in which case it is called idiopathic.
Causes of the rash
Although the emergence of such a pathology has not yet been fully studied, the prevailing opinion among doctors is that the problem is associated with hormonal changes during pregnancy, as well as with the natural physiological changes that occur during this period, since certain sweat glands are activated. In addition, stretching the skin leads to itching.
Many people believe that a rash is a sign of pregnancy. In fact, it does not occur in every woman.
The reasons that provoke it are the following:
- Immunity changes that occur during pregnancy are aimed at preventing fetal rejection.
- Genetic predisposition. This is what causes most autoimmune processes. It is interesting that in this case, allergic reactions are caused not so much by external irritants as by the placental antigen.
- Damage to connective tissue. It often happens that a rash during pregnancy itches not because of a classic allergic reaction, but because of an increase in the size of the abdomen and the associated stretching of the skin. The connective tissue fibers are damaged, fragments of elastin and collagen enter the blood, and the body perceives them as allergens, hence the reactions in the form of rashes and itching.
READ ALSO: Acne due to problems with the intestines and stomach - causes of appearance and methods of treating the face
In some cases, the rash and itching are not caused by allergic reactions, but by gestational cholestasis, that is, stagnation of bile, which can occur during pregnancy.
Cystic dermatosis
The exact causes of the disease have not been fully established, but usually blistering dermatosis occurs due to autoimmune diseases. Factors in the development of blistering dermatosis can be viruses, infection, etc.
Symptoms of cystic dermatosis
Pemphigus belongs to the group of bullous dermatoses, which are characterized by the appearance of blisters on the skin.
Manifestations of blistering dermatosis depend on its form:
— Seborrheic (blistering formations in the chest, back and head);
— Vulgar (bubbles on the skin or mucous membrane);
— Leaf-shaped (blisters that become crusty over time and hyperpigmentation);
— Vegetating (bubbles form on the folds of the skin).
Treatment of cystic dermatosis
Treatment of blistering dermatosis consists of prolonging the patient’s life and achieving stable remission of the disease. The patient is prescribed corticosteroids and cytotoxic drugs. Medical therapy is also carried out aimed at eliminating concomitant diseases, such as candidiasis, pneumonia and others.
Atopic dermatitis of pregnancy
It accounts for more than 50% of rash cases. It usually causes a rash during early pregnancy. Other types of skin diseases appear later, but atopic dermatitis can occur as early as the first trimester. Caused by changes in immunity during pregnancy.
Practice shows that after childbirth in 80% of cases it goes away and does not bother the woman anymore. Such reactions manifest themselves as prurigo, eczema and itchy folliculitis. They pose no danger.
Pemphigoid of pregnancy
It is a fairly rare autoimmune pathology when the allergen is a placental antigen. Accompanied by itching and a rash in the form of blisters. It usually goes away after birth, but the baby may develop a rash.
Fortunately, this is a rarer disease compared to atopic dermatitis, since it causes complications such as fetoplacental insufficiency, premature birth, and so on. And in the postpartum period, problems can begin - for example, postpartum thyroiditis develops. In addition, during menstruation or while taking hormonal medications, there may be relapses of the disease.
All of these diseases require treatment, so you should definitely consult a doctor.
Symptoms that accompany the rash
It should be noted that rashes can have different localizations. For example, a rash on the hands during pregnancy is mainly a manifestation of atopic dermatitis.
With this disease, red eczematous spots also appear on the face and neck, and on the hands they are localized mainly on the palms and flexor surfaces. It appears especially often in primiparous women. With atopic dermatitis, a rash on the legs during pregnancy is also not uncommon. In particular, it is localized under the knees and on the soles. But there are practically no rashes on the stomach.
READ ALSO: What are the differences between boils and boils, symptoms of the disease and treatment methods
With itchy folliculitis, the rash is similar to acne. It most often occurs on the shoulders and back, stomach, and arms. Pimples are located near the hair follicles. They can be quite large - 2-4 mm in diameter.
With polymorphic dermatosis, the rash consists of itchy red papules. They mainly appear on the abdomen, then spread to the thighs and buttocks. Mostly the rash occurs over stretch marks. It does not occur on mucous membranes. The skin around the navel and on the face also remains clean. Although individual spots have a diameter of 1-3 mm, they tend to merge into large spots.
It happens that a rash occurs on the face during pregnancy. It indicates the presence of allergic reactions, which may be accompanied not only by itching, but also increased tearing, runny nose and other symptoms.
With pemphigoid, the rash most often appears at 4-7 months. It is mainly localized on the skin around the navel, but can also occur on the chest or back. The rashes look like blisters. If they are damaged, erosions appear in their place, and when the crust dries out.
Intrahepatic cholestasis is characterized by yellowing of the skin and itching, which is especially acute on the palms and soles. The rash is usually secondary in nature. Very often a woman scratches it, because the itching is almost unbearable.
Abstract
Dermatoses that occur during pregnancy are very important to know for the clinician, since they affect a large number of pregnant women and pose a danger to the fetus. These diseases include pemphigoid of pregnancy, polymorphous eruptions of pregnancy, intrahepatic cholestasis of pregnancy and atopic rash of pregnancy. This review describes the pathogenesis, clinical features and treatment of these dermatoses.
Introduction
During pregnancy, there are three groups of skin diseases. The first group includes benign diseases that arise as a result of hormonal changes that occur during pregnancy; the second group includes pre-existing diseases that worsened during gestation; The third group includes dermatoses specific to pregnancy [1].
Dermatoses of pregnant women are a specific group of itchy pathologies that occur only in pregnant women. Due to the unclear etiopathogenesis, rare occurrence and similarities in the clinical picture, there is ongoing debate about how to classify these diseases. The latest classification was proposed by Ambrus-Rudolph [2] in 2006, and includes pemphigoid of pregnancy, polymorphic dermatosis of pregnancy, intrahepatic cholestasis and atopic rash of pregnancy (Table 1).
Table 1
| Dermatosis | Pathogenesis | Clinical picture | Localization | Paraclinical diagnostics | Treatment | Risks to the fetus |
| Pemphigoid of pregnancy | Circulating IgG, complement activation, antibody reaction with the amniotic epithelium, placenta, skin basement membrane, leading to an autoimmune reaction and tissue damage with the formation of a blister. | Pruritic papules and plaques, ring-shaped vesicles, tense blisters on an erythematous background | Periumbilical region, extending to thighs, palms and soles | Histology: identification of superficial and deep lymphocytohistiocytic eosinophilic infiltrates; PIF: deposits of IgG and C3 on the basement membrane | Systemic corticosteroids at a dose of 0.5 mg/kg, with a gradual reduction to a maintenance dosage depending on the activity of the disease; topical GCS classes III and IV; Cyclosporine a, dapsone, azathioprine, or methotrexate (after childbirth) | Urticaria or vesicular rash in newborns (due to the transfer of antibodies from mother to fetus); premature birth, fetal malnutrition; toxicity when using cyclosporine A. |
| Polymorphic rashes of pregnant women | Overstretching of the anterior abdominal cavity due to an increase in body weight, leading to inflammation of the connective tissue; changes in cortisol levels; atopy. | Severely itchy urticarial rashes, edematous papules and plaques, papulovesicles, erythema, blisters, blisters. | Abdomen, without involving the umbilical area, buttocks, thighs, back | Histology: Dermal edema, with a perivascular lymphocytic infiltrate consisting of eosinophils, T cells and macrophages | Topical and systemic corticosteroids, antihistamines | There are no side effects associated with the disease and the use of systemic corticosteroids; use only antihistamines approved during pregnancy |
| Intrahepatic cholestasis of pregnancy | Hormonal changes, genetic predisposition, exogenous factors (seasonal fluctuations), diet. | Severe pruritus, without primary skin lesion, with or without jaundice | First on the palms and soles, followed by spreading to the entire skin; excoriation, prurigo, nodules | Increase in serum bile acids and aminotransferases | Ursodeoxycholic acid, phototherapy | Preterm birth, intrapartum fetal distress, stillbirth, vitamin K deficiency, coagulopathies |
| Atopic rash of pregnancy | Decreased production of cytokines by T-helpers of the 1st order, increased production of cytokines by T-helpers of the 2nd order | Skin itching, excoriation, secondary infection | 66% - eczematous skin lesions in areas typical of atopic dermatitis; 33% - slight itching, papules on the trunk and limbs | There are no pathognomonic symptoms specific to the disease, elevated serum IgE levels in 20-70% | Topical corticosteroids class II–IV. Topical GCS. Antihistamines. phototherapy Antibiotics in cases of secondary infection. | There are no risks, other than a high risk of the child developing atopic dermatitis in the future. |
The purpose of this review is to examine four specific dermatoses of pregnancy. Some dermatoses pose a risk to fetal development and are therefore an important topic for clinicians.
Pemphigoid (herpes) of pregnant women
Pemphigoid of pregnancy is a rare autoimmune skin disease that causes intense itching and occurs only during pregnancy. In terms of clinical and immunological characteristics, pemphigoid of pregnant women is similar to other cystic dermatoses.
Due to the similarity of the morphological picture - blisters - the former name of this disease is herpes of pregnant women. The name was changed due to the lack of connection with herpes virus infection. The disease occurs in the second and third trimester of pregnancy [2,3], but cases have been reported in the first trimester and postpartum period [2,4,5]. The prevalence of the disease is the same throughout the world and is 1:60,000 [6,7]. The pathogenesis is not fully understood, but in 61–80% of cases there is an association with HLA–DR3 and 52–53% with HLA–DR4 [8].
Pathogenesis
The primary immune response occurs within the placenta. Circulating IgG reacts with the amniotic epithelium of placental tissue and the basement membrane of the skin. Autoimmune reactions occurring in the skin are associated with the accumulation of immune complexes, complement activation, chemotaxis and degranulation of eosinophils, resulting in tissue damage and blistering [9]. The main initiating factor remains unclear, but it is assumed that the allogeneic or autoimmune reaction is associated with deviation from normal expression of the TI product by the major histocompatibility complex [10].
There are reports of cases of pemphigoid in pregnant women during menstruation and after taking oral contraceptives. These observations suggest a role for sex hormones in the pathogenesis of the disease [6,11,12], although there are also studies suggesting the opposite [13].
Clinical features
Pemphigoid of pregnancy begins with the appearance of intensely itchy urticarial ring-shaped rashes, then vesicles and large tense blisters appear on an erythematous background. The favorite location is the periumbilical region (Fig. 1). In 90% of cases, the rash subsequently spreads throughout the abdomen, and in some cases, to the thighs, palms and soles [11]. Often, the disease subsides in the last month and worsens immediately after childbirth. The activity of the process decreases and disappears during the first months after birth, and reappears during subsequent pregnancies. In most patients, the disease resolves into spontaneous remission, without treatment, several weeks or months after delivery.
Diagnostics
The diagnosis of pemphigoid in pregnant women is based on the characteristic clinical picture, histological examination and direct immunofluorescence. The classic histological picture is characterized by the presence of superficial and deep perivascular lymphohistiocytic eosinophilic infiltrates. Direct immunofluorescence reveals deposition of IgG and C3 complement on the basement membrane [4, 11]. Deposition of C3 complement is detected in 100% of cases, while IgG deposition is found only in 25–50% [11].
Treatment
Treatment of pemphigoid in pregnant women begins with oral corticosteroids at a dose of 0.5 mg/kg, then the dose is gradually reduced to maintenance, depending on the activity of the disease. For mild cases, it is possible to use topical corticosteroids of class III and IV. If topical and systemic corticosteroids are ineffective, treatment is supplemented with the use of systemic immunosuppressants, such as Cyclosporine, Dapsone, Azathioprine, Methotrexate (after childbirth).
The effect of pemphigoid in pregnant women on the fetus
As a result of transplacental transfer of IgG1 antibodies from mother to fetus, 10% of newborns develop a mild clinical picture consisting of urticaria or vesicular skin rashes [9] (Fig. 2). Pemphigoid in pregnancy is associated with premature birth and fetal malnutrition. Some researchers have suggested that abnormalities in newborns are associated with the use of systemic corticosteroids, but most likely this is due to the activity of the dermatosis, and not to the use of corticosteroids. A high risk of developing pathology in the fetus is often associated with the development of pemphigoid of pregnancy in the first and second trimester. Systemic use of GCS does not affect the outcome of pregnancy [14]. However, it is necessary to monitor the condition of the pregnant woman while taking systemic corticosteroids. Also, due to toxicity to the mother and malnutrition on the part of the fetus, careful monitoring of patients when taking Azathioprine is necessary. Azathioprine can be taken during pregnancy, but its use must be supervised. Methotrexate is contraindicated during pregnancy.
Comorbid diseases
Pemphigoid pregnancy is often associated with other autoimmune diseases, such as Graves' disease, thyroiditis, and pernicious anemia [5,11]. This is due to the presence of HLA antigens – DR3 and DR4 [15] in these autoimmune diseases.
Polymorphic dermatosis of pregnancy
Polymorphic dermatosis of pregnancy is a benign, self-limiting inflammatory disease, more often found in primigravidas in the third trimester or postpartum period [9,16,17]. Rarely occurs in subsequent pregnancies [17]. This is the most common dermatosis in pregnant women, its incidence is 1 in 160 pregnancies [9,18]. Although the incidence of the disease is high, the etiology is still unclear. There is a relationship with a large increase in body weight, immuno-hormonal changes, but not a single theory has yet been substantiated [3,9,18].
Pathogenesis
The pathogenesis of the disease has not yet been studied. It is assumed that overstretching of the abdominal wall leads to damage to the connective tissue, causing an inflammatory reaction [9,18]. In a study involving 200 patients with polymorphic dermatosis, a decrease in serum cortisol was found compared to the control group. Another theory is the presence of atopy in pregnancy. A study of 181 patients found that 55% had atopy [18]. There is still no evidence regarding the contribution of circulating immune complexes and the presence of HLA class to the pathogenesis.
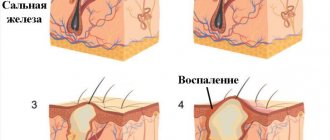
Clinical features
The favorite localization of rashes is the abdomen, usually on striae, without affecting the navel area; the disease begins with the appearance of itchy erythematous urticarial papules and plaques (Fig. 3). Characterized by rapid spread to the thighs, buttocks, chest and back. Involvement of the hands and feet is rare [9]. The rashes are characterized by polymorphism: papulovesicles, purpura, vesicles.
Diagnostics
There are currently no diagnostic methods. Histopathology varies depending on the stage of the disease. Diagnosis is based on clinical picture and biopsy. A biopsy reveals superficial dermal edema, a perivascular lymphocytohistiocytic infiltrate consisting of eosinophils, T helper cells and macrophages. At later stages, epidermal changes are detected: hyper- and parakeratosis [9,16].
Treatment
Treatment is symptomatic. Corticosteroids with or without antihistamines are usually sufficient to relieve itching and rashes. In severe cases, the use of systemic corticosteroids may be necessary. More often, the disease resolves itself within a few weeks after birth without pigmented post-inflammatory scars.
Risks to the fetus
Polymorphic dermatosis of pregnant women is not dangerous for the fetus and newborns. The outcome of the disease in the mother is usually favorable. When taking topical and systemic corticosteroids, monitoring the condition of the pregnant woman’s body is necessary. When prescribing antihistamines, preference should be given to Cetirizine, Loratadine and Fexofenadine.
Intrahepatic cholestasis of pregnancy
Intrahepatic cholestasis of pregnancy is characterized by severe itching and secondary skin lesions in the third trimester of pregnancy. Cholestasis of pregnancy is a reversible form of cholestasis that develops in genetically predisposed individuals. Cholestasis of pregnancy does not belong to primary dermatosis, but due to the correlation of the manifestations of skin symptoms during gestation and the presence of risks to the fetus, it was classified as a specific dermatoses of pregnant women. The prevalence of dermatosis is highest in Scandinavia and South Africa, with a frequency of about 1%.
Pathogenesis
The pathogenesis is based on the interaction of hormonal, genetic and environmental factors [9]. Exogenous factors include seasonal environmental fluctuations [21], as well as dietary patterns and selenium deficiency [22]. The role of exogenous factors in the development of the disease is still being studied.
Clinical picture
Intrahepatic cholestasis of pregnancy is characterized by the presence of itching without primary skin lesions with or without jaundice. Incidence of jaundice: 0.02 – 2.4% [23]. Itching usually begins on the palms and soles and then spreads throughout the entire skin. Intense itching is often combined with secondary excoriations (Fig. 4). They are usually localized on the lower extremities, often in the lower legs. Symptoms usually resolve within 1–2 days after delivery, but may persist for 1–2 weeks [9]. There is a high risk of recurrence of the disease with repeated pregnancies (50–70%), as well as with the use of oral contraceptives.
Diagnostics
The diagnosis is based on the presence of skin itching, increased levels of bile acids and aminotransferases.
Treatment
The goal of treatment is to reduce the level of bile acids in the blood serum and eliminate skin itching. To relieve skin itching, ursodeoxycholic acid can be used; no side effects or effects on pregnancy outcome are observed with their use [24]. The use of cholestyramine, antihistamines, topical and systemic corticosteroids does not have an evidence base and may have an adverse effect on pregnancy outcome [1,24]. In exceptional cases, phototherapy may be used.
Risks to the fetus
Cholestasis in pregnancy is associated with preterm birth (20–60%), followed by the development of intrapartum fetal distress (20–30%), as well as stillbirth (1–2%) [9]. Severe cholestasis can lead to vitamin K deficiency and coagulopathies in pregnant women and children [1]. This needs to be monitored closely during and after pregnancy.
Atopic rash of pregnancy
Atopic rash of pregnancy is a benign condition characterized by pruritic eczematous or papular lesions, most often in those predisposed to atopic dermatitis or with a history of atopic dermatitis. The term "Atopic rash of pregnancy" refers to a heterogeneous group of pruritic disorders during pregnancy, such as prurigo gravidarum, pruritic folliculitis of pregnancy, and eczema gravidarum. Atopic rash is the most common cause of pruritus during pregnancy [2,16]. The disease has two groups of patients: the first group of patients who have a history of atopic dermatitis, and the second group of patients includes pregnant women whose atopic rash appeared for the first time during pregnancy. In 80% of pregnant women, the rash appeared for the first time [2]. The disease develops early in the first or second trimester and usually recurs in subsequent pregnancies. Most pregnant women with atopic rash have elevated levels of IgE in the blood. Such pregnant women have positive tests for allergens, as well as a family history of atopic dermatitis.
Pathogenesis
It is believed that the pathogenesis of atopic rash is based on immunological changes. Pregnancy is associated with a shift in the immune response towards the production of Th 2nd order cytokines (IL - 4 and IL - 10). The production of anti-inflammatory cytokines is responsible for skin changes during pregnancy [25].
Clinical picture
The main clinical features are pruritus, prurigo, excoriation, and eczematous skin lesions (Fig. 5). In two thirds of pregnant women, the rash is localized in places typical for atopic dermatitis, on the face, neck, flexor surfaces of the limbs; in the remaining pregnant women, the rash is localized on the torso and limbs and is accompanied by slight itching. Scratching leads to excoriation and secondary skin infections. Eczema usually disappears after delivery.
Diagnostics
The diagnosis is based mainly on the clinical picture. There are no pathognomonic symptoms for atopic rash in pregnant women. An increased level of IgE (20–70%) can be detected in blood serum [2].
Treatment
Treatment depends on the severity of the disease. Usually, the use of topical corticosteroids of class III and IV is sufficient, but in severe conditions, systemic corticosteroids and antihistamines may be necessary. If treatment is ineffective, phototherapy may be used. When a bacterial infection occurs, the use of antibiotics is necessary.
Risk to the fetus
Atopic rash in pregnancy does not affect the development and condition of the fetus and newborns, but indicates that the child has a high risk of developing atopic dermatitis in the future.
conclusions
Skin itching and rashes are common during pregnancy and are usually benign and self-limiting. They constitute a small group of inflammatory diseases associated with pregnancy and/or the early postpartum period, which can lead to severe fetal pathologies, stillbirth and premature birth [23].
Itching is a common symptom for this group of diseases. The diseases differ in the morphology of the rash, localization, and time of occurrence, but at the same time they have much in common. For inexperienced clinicians, it can sometimes be difficult to make a diagnosis based on clinical presentation alone. Ancillary diagnostic methods include histopathology, blood tests, and direct immunofluorescence. For pemphigoid of pregnancy and cholestasis of pregnancy, laboratory tests are fundamental. Therefore, it is necessary to take into account the history, clinical picture and histopathology to make a diagnosis.
There is a risk to the fetus only with pemphigoid and cholestasis of pregnancy. For a successful pregnancy outcome, multidisciplinary monitoring is required with the participation of a dermatologist, pediatrician, obstetrician, and gastroenterologist.
Diagnostics
In order to make a correct diagnosis, the doctor will prescribe additional research. After all, it must exclude infections, microbial damage, and other pathologies.
One of the most informative studies from this point of view is a biochemical blood test. It allows you to identify the presence of obstetric cholestasis, since with this disease the level of bile acids in the blood increases significantly; in approximately 20% of expectant mothers who are faced with the problem of a rash, the level of bilirubin also increases.
And in the vast majority of cases, the analysis shows a significant increase in the activity of liver enzymes. For other diseases that manifest as a rash, the parameters in the biochemical analysis remain within normal limits.
To exclude microbial or fungal infection, the scraping or the contents of the rash bubbles are analyzed for microflora, and luminescent diagnostics are also performed. When diagnosing, it is very important to exclude scabies, seborrhea, bacterial folliculitis, hepatitis and a number of other diseases, since they require other methods of therapy.
For atopic dermatitis and herpes, an analysis is carried out to determine the content of IgG4 antibodies (with herpes, the indicator increases) and IgE (this indicator reflects the course of the allergic reaction).
Finally, if pemphigoid and polymorphic dermatosis are suspected, a histological examination of a skin biopsy is performed.
Introduction
Lichenoid dermatoses of the vulva are a heterogeneous group of diseases with a number of similar clinical and/or morphological features [1].
The clinical picture of lichenoid dermatoses is characterized by the appearance of papules with superficial, tightly adjacent scales (from the Latin Lichen
- lichen, a symbiotic association of fungi and microscopic green algae) [2]. Their prototype is lichen planus (LP); in addition, lichenoid dermatoses include lichenoid rashes and lichenoid contact dermatitis, graft-versus-host disease, lichen sclerosus and atrophic dermatoses, and focal neurodermatitis [1].
Histologically, the lichenoid model of inflammation is characterized by damage to the cells of the basal layer of the epidermis and the formation of a strip-like infiltrate in the upper dermis [3]. The International Society for the Study of Vulvovaginal Disease (ISSVD) includes LP and the early stages of lichen sclerosus and atrophic lichen of the vulva to the group of dermatoses with such a histological pattern [4]. Some authors recommend including Zoon plasma cell vulvitis in this group [2], which also has similar clinical features to the erosive form of vulvar LP.
The similarity of the clinical and histological picture of lichenoid dermatoses makes their differential diagnosis difficult. In the last decade, the dermatoscopy method has been widely used in the diagnosis of inflammatory dermatoses [5, 6]. Despite the small number of publications concerning the dermoscopic signs of vulvar dermatoses, the distinctive features of each of them can be identified and used as an additional method for diagnosing this group of diseases [7–9].
The purpose of this review is to systematize the most characteristic clinical, morphological and dermoscopic signs of lichenoid dermatoses of the vulva, the consideration of which is necessary for the correct diagnosis (Table 1).
Treatment of rashes: basic methods
Itching and rashes during pregnancy must be treated comprehensively, including eliminating the cause of their appearance, depending on what causes such phenomena.
READ ALSO: Apple cider vinegar use in folk medicine ✦ 33 secrets ✦
For example, antihistamines are used for atopic dermatitis and other types of allergies. They can affect the fetus, so they are prescribed with caution in the first trimester if the benefit to the mother outweighs the risk to the baby. In such cases, 2-3 generation antihistamines are used - Histafen, Claritin, Zyrtec, Cetirizine.
If the rash is accompanied by severe inflammation, then for all types of diseases, except for itching of pregnancy (that is, atopic dermatitis, polymorphic dermatosis, pymphegoid), corticosteroids can be prescribed. For example, this could be an ointment based on hydrocortisone or prednisolone.
There is no specific treatment for pemphigoid, so most often the hormonal agents described above are also used.
For obstetric cholestasis, ursodeoxycholic acid drugs are prescribed. It improves the composition of bile, reduces the concentration of toxic types of bile acids in it, and promotes the outflow of bile. For this disease, hepatoprotective drugs are additionally prescribed to protect the liver, for example, Karsil, as well as cytostatics (Methotrexate). It is recommended to take the antihistamines and vitamins described above.
Finally, it is important to observe certain dietary restrictions, avoid spicy, fatty, salty foods in order to support the liver. Sometimes therapeutic massage or special physical exercise are prescribed.
Emollients
These are creams and lotions that are used for such diseases for skin care to restore damaged epidermis, moisturize and soften the skin, and promote the regeneration of intercellular lipid structures.
Most emollients have no contraindications for expectant mothers, but you need to carefully study their composition so that it does not contain components that could cause allergic reactions.
The composition may include peach or olive oil, panthenol, and other natural and synthetic ingredients to moisturize the skin.
Popular emollients include, for example, Bepanten cream, which is even recommended for use in the treatment of atopic dermatitis in infants.
During pregnancy, it is important to take proper care of your skin to prevent rashes caused by poor hygiene.
As such, there are no preventive measures against dermatoses. But doctors recommend abandoning synthetic underwear and clothing in favor of products made from natural fabrics, and also eliminating contact with various allergens: house dust, animal hair, plant pollen. To do this, it is recommended to regularly do wet cleaning and wash the window screens, and during the flowering period to stay away from potential sources of problems.
It is very important to choose the right washing powder so that it does not cause either atopic or contact dermatitis.
How is dermatitis treated during pregnancy?
Both forms of dermatoses, which most often affect pregnant women, are treated with almost the same groups of drugs. Many women resort to treatment with folk remedies in order to avoid taking medications, which are undesirable during pregnancy. But this type of treatment should also be carried out only after consulting a doctor.
After a visual examination and establishing the degree of development of the disease, the doctor prescribes one or a set of methods for conservative treatment of such a lesion:
1. When there is a risk to the health of the fetus, one of the antihistamines is prescribed: Suprastin, Loratadine, Claritin or their analogues.
2. For external treatment of affected areas of the skin, antipruritic ointments, mash and creams are prescribed: Bepanten, Desitin, Losterin, etc.
3. When treatment is carried out in a hospital, corcosteroid creams and ointments are prescribed, as well as antiallergic and sorbent drugs (Enterosgel, Filtrum).
Folk remedies against dermatitis in pregnant women
If a woman has a negative attitude towards taking medications, then folk recipes can be used in the fight against dermatosis (not a severe stage).
Among them, the most effective are:
- compresses with rosehip oil extract;
- lotions with Kalanchoe juice;
- mix water and birch sap in equal parts and treat the affected areas of the skin with this mixture;
- oak bark decoction compress;
- applying cabbage leaf;
- elderberry or nettle decoction – 1 tbsp. before bedtime.
During the period of treatment for dermatitis, a pregnant woman should avoid any stressful situations, overwork, and lack of sleep.
It is against the background of frequent experiences that dermatitis worsens, and the effectiveness of its treatment is reduced to nothing.