For women, caring for the skin of the hands is of particular importance, because this part of the body, in fact, is a kind of calling card. Pimples on the fingers, for example, around or near the nails, often become a real tragedy for the fairer sex. Therefore, protecting the skin around the nails, as well as on the entire surface of the hands, is of particular importance.
Causes of an abscess
They are associated with external influences. When a wound forms on the skin, dirt and infection get into it, leading to suppuration. Why does the inflammatory process develop and the wound does not heal, as often happens?
- People who have metabolic disorders or blood diseases are susceptible to the development of complications.
- The skin breaks out near the big nail if it grows in.
- Fungus can lead to inflammation.
- A manicure done with poorly processed, non-sterile instruments is the cause of panaritium.
- A sore finger on the hand near the nail in people with a bad habit of biting nails, as a hangnail forms.
- Increased stress on the hands due to professional activities (agricultural work, carpentry, carpentry).
If you follow certain rules of prevention: work with gloves, have your nails done only by a professional in compliance with sanitary standards, do not injure your hands, you can avoid unpleasant consequences.
Symptoms of the disease
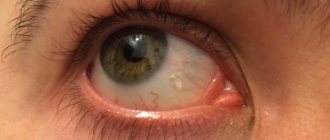
Severe throbbing pain appears in the area of inflammation, and the skin turns red.
The finger swells and becomes difficult to bend. If the inflammation increases and covers a large area on the arm, a temperature appears. Under these conditions, purulent inflammation is caused by Staphylococcus aureus, which appears on the injured area. Chronic inflammation under the nail develops more slowly, manifested by swelling, redness around the injury, and painful sensations. Other microbacteria (Gram-negative cocci) are involved in the inflammatory process. People with diabetes or people who frequently expose their hands to chemicals and water are at risk of getting this form: bar workers, cleaners, cooks, nurses.
It is important to note that the diagnosis is determined visually: redness, swelling, suppuration. The patient experiences severe throbbing pain. If the symptoms spread beyond the damaged area, to the fingertip, a serious infection has begun - panaritium. Then an abscess will begin, and you will have to do drainage to release the pus.
! You cannot open an abscess yourself in order to drain the pus! It may spread higher up the arm.
If you have suppuration, you need to contact a surgeon, he will carry out the drainage himself. This should be done if the condition is accompanied by chills and fever. This means that the acute form has taken on the character of a severe infection.
How long it will last depends on the severity of the disease and the timely measures taken. Typically, healing occurs within a week or more. The chronic form takes weeks, even months to heal; local treatment is not enough.
Antifungal and anti-inflammatory drugs are prescribed. The disease rarely develops and leads to serious consequences. In most cases, there is no trace left after treatment. However, felon may return.
Fungus on the hands: causes, symptoms, how and how to treat
Fungus on the hands is a very dangerous disease that affects the dermis of the hands and nail plates. It is very easy to catch fungus on the palms, since fungal spores can be found anywhere. Fungal spores flake off along with the scales of the dermis and settle on household items. Through abrasions and cuts they are transferred to the epithelial layer and begin to infect the dermis.
Pathogens
Fungus on the palms and fingers is caused by two pathogens:
- Dermatophytes. The disease is common among the male population. Initially, lesions appear between the fingers, after which the infection spreads further. Most often it is Trichophyton mentcigrophytes or Trichophyton rubrum.
- Yeast-like fungi. The female half often suffers from such a pathogen. Albicans are usually the causative agents.
How do we get infected?
There are several ways to get a fungal infection. They may be:
- from oneself if a person is infected with foot fungus;
- intra-family infection if someone is already sick at home;
- by shaking hands;
- the use of other people's unprocessed manicure accessories;
- going to baths, saunas or swimming pools;
- touching the handrails.
Factors predisposing to infection are:
- presence of cuts and abrasions;
- poor blood circulation;
- decreased immunity;
- excessive sweating of the palms;
- stressful situations;
- use of toxic drugs;
- changes in hormonal levels;
- the appearance of endocrine disorders;
- poor nutrition;
- failure to comply with personal hygiene rules.
It is very important to maintain your personal hygiene in order to avoid infection.
Clinical manifestations of the disease
Symptoms of fungus on the hands manifest differently in different patients. They differ in the type of stimulus. General signs of hand fungus are noticed in various areas:
- nail plates;
- the outer and inner sides of the palms;
- interdigital parts.
Symptoms
Many symptoms can tell you what skin fungus looks like on your hands. At the very beginning of infection, the dermis begins to itch, itch, swell and peel. In later stages, an inflammatory process and severe pain occur, which cause terrible discomfort.
At first, the symptoms are not pronounced. Single symptoms can easily be confused with simple irritation and dry hands. As the fungus on both hands progresses, it infects larger and larger parts of the skin. The most obvious signs are:
- the appearance of redness;
- peeling;
- inflammation of the cuticle;
- the appearance of interdigital folds;
- severe itching of the palms;
- swelling of the epidermis;
- the appearance of calluses;
- the appearance of cracks in the dermis;
- the appearance of a rash.
If there is no proper treatment for a dangerous fungus on the hands, the infection begins to spread to the nail plates. Symptoms of nail fungus include:
- modification of the nail and its color;
- severe brittleness of the nail;
- dulling of nail growth;
- separation of the plate.
Important! When the first symptoms appear, you must consult a doctor and begin treatment at the first stage.
Diagnostics
Before starting treatment, it is necessary to correctly diagnose the disease. Its symptoms are very similar to those of other dermatological diseases. Self-diagnosis is prohibited. To prescribe competent treatment, the following manipulations are carried out:
- at the first visit to a specialist, it becomes clear what kind of fungus has affected the epidermis;
- To make a diagnosis, scraping from the infected part of the epidermis is required;
- the diagnosis is made after examining the patient and PCR diagnostics of scrapings for types of infectious agents;
- sometimes changes in the nail are not associated with a fungus at all (in this case a blood test is taken).
Affected nails may also indicate the following pathologies:
- plate fragility – calcium deficiency;
- softness – insufficient amount of iron;
- yellowish tint – poor functioning of the liver and gastrointestinal tract;
- tuberosity – the presence of inflammatory processes in the body;
- whitish stripes – deficiency of zinc, iodine.
Treatment
Fungus on the palms of the hands can be cured using an integrated approach to treatment. The cure may be:
- systemic: use of tablets and capsules;
- local: use of ointments, creams, peel-off patches, medicinal varnishes;
- folk remedies: baths, homemade creams and ointments, compresses, decoctions, tinctures.
Before using this or that method, you must consult your doctor.
Systemic treatment
It is clear how to cure the disease. But which drugs are the most effective? In order to kill the infection, the following is prescribed:
- Fluconazole. These are capsules that completely destroy mushrooms. The drug is taken once a day, 50 mg for 2-4 weeks, depending on the manifestations. It should not be taken by children under 6 years of age, pregnant women or during breastfeeding. Dizziness and nausea may occur.
- Itraconazole Highly effective against many pathogens. Do not take during pregnancy and breastfeeding, heart pathologies, hypersensitivity to the components in the composition. Side effects include allergies, nausea, and dizziness.
- Ketoconazole. The tablets fight all types of irritants. Take 1-2 tablets per day. The duration of therapy is determined by the doctor. Prohibited for renal failure, pregnancy and breastfeeding. Side effects include vomiting, dizziness and allergic reactions.
Local treatment
The most effective medications for local therapy are:
- Candide. This is an ointment whose action is aimed at destroying many pathogens. Apply 2 times a day. The minimum course of therapy is 4 months.
- Nizoral. Actively fights almost all types of irritants that affect the dermis of the limbs. Use once daily for at least 2 months.
- Zalain. This is an ointment that fights all types of fungi. Apply 2 times a day. The duration of therapy is 2-4 weeks.
- Exoderil. With this ointment, therapy lasts up to 4 weeks. Apply twice a day.
Absolutely all drugs have contraindications. These include hypersensitivity to components, gestation period, and kidney disease. After use, side effects may occur, which manifest themselves in the form of itching, redness, and irritation.
Treatment
At home, treatment comes down to the following procedures:
- treating the torn finger with a light pink solution of manganese or other antiseptics (iodine, hydrogen peroxide, brilliant green, alcohol solution);
- applying ointment (Vishnevsky, Ichthyolova, Levomikol) so that the abscess ripens and the pus flows out;
- applying a bandage to the inflamed area, which must be changed periodically.
! If the fungus or herpes has penetrated the skin under the nail, it cannot be cured on its own. It is better to consult a dermatologist or surgeon.
Treatment is carried out traditionally. You should avoid putting pressure on your arm for a long time until the abscess disappears. If the inflammation is moderate, you can try to cure your finger using folk remedies:
- soak your feet or hands in hot water and antibacterial soap;
- for fungus, after removing moisture - dry with powder, a bath of warm water with apple cider vinegar;
- a self-prepared lotion from oregano oil with another vegetable oil (12).
Other Treatment Options
Folk remedies help at the very beginning of the disease or at the end, when there is no longer inflammation. When traveling or hiking, it is recommended to make baths from laundry soap, water, and alcohol. If you don’t have antibacterial ointment on hand, you can apply a baked onion in the form of a paste.
To drain the pus, use a cake made from honey and flour. You can pick a leaf from a coltsfoot or plantain plant and wrap it around your sore finger. Prepare vegetable mush from carrots, beets, and onions.
If it comes to visiting a doctor, since all the methods have not helped, antibiotic treatment will be prescribed: Mitronidazole, Clindamycin; fungal inflammation is treated with Lamisil, Mycosalon, Triderm. Plus treatment with ointment, changing the bandage daily until the abscess disappears. We must try to destroy the bacteria so that the infection does not affect the deeper layers: tendons, bone.
If there is no result after such treatment methods, the surgeon will open the abscess. He will cut the abscess, remove dead cells, and clear the cavity of pus. If necessary, the nail plate is removed. Then the wound is treated and a bandage is applied. An antibiotic is administered intramuscularly. Within a week, the patient visits a doctor to treat the wound.
If a child's finger breaks, the same measures are taken. This phenomenon is very common if the splinter is not pulled out in time or the cut on the fingertip is not treated immediately. On a child's dirty hands, the infection enters the wound and spreads under the nail.
What to do: wash the injured area with a solution of St. John's wort, calendula, chamomile or antiseptic; make a bath of potassium permanganate; treat with iodine and brilliant green.
Prevention
The most important thing is good hand and foot hygiene. In order to prevent the appearance of an abscess you need to:
- Keep your feet and hands clean and dry.
- If necessary, wear rubber and other protective gloves, the lining of which is made of cotton fabric that absorbs moisture well.
- Do not bite your nails or the skin around them. Don't let children do this!
- Manicure and nail care should be very careful, without cutting the cuticle or injuring it. Toenails should be properly trimmed into a rectangular shape to prevent ingrown toes.
- If you have diabetes, do not neglect your diet, take medications, and maintain normal blood sugar levels to avoid prolonged wound healing.
- When leaving the countryside or going to the country, put antiseptic ointments, bandages, gauze pads, and adhesive plaster in your first aid kit. Treat any wounds that appear immediately, preventing the spread of microbes under the skin and the occurrence of inflammation.
Non-dermatophytic onychomycosis. Symptoms and treatment
Have you been trying to cure FUNGUS for many years?
Head of the Institute: “You will be amazed at how easy it is to cure fungus by taking the product every day for 147 rubles ...
Read more "
The causative agents of fungal nail diseases are various types of fungi: yeast, mold and dermatophyte. Non-dermatophytic onychomycosis can be caused by yeast or mold representatives of the infection.
Infection with yeast fungus leads to thinning of the nail and a change in its color to a yellowish tint. In this case, the diseased nail plate moves away from the bed.
The action of mold fungus extends not only to the nail tissue, but also to the skin located around it, on which quite dangerous ulcers develop. This type of onychomycosis affects nail plates already infected with a fungal infection, and can also develop against the background of existing diseases. In this case, the nail becomes yellow, blue, brown, green and even black. The peculiarity of mold fungus is its superficial action without penetration deep into the nail tissue.
How does mold manifest itself?
The first sign of onychomycosis is clouding (sometimes darkening) of the nail, loss of a healthy appearance.
Further development of the disease leads to thickening and deformation of the nail plate, which becomes brittle and can peel off on its own.
Fungus of mold origin can appear not only on the nail.
Dryness and flaking appear in the spaces between the fingers, accompanied by intense itching.
Fluid-filled blisters may appear on the skin around the nail. In place of the burst bubbles, microcracks remain, which cause pain.
Untimely initiation of treatment can result in the appearance of ulcers, deformation of the plate and irreversibility of the process.
Pensioners! Don't cut fungal nails! They are derived simply: take 9 grams...
Military doctor: So that the soldiers do not have fungus, they 2 times a day...
How is mold fungus treated?
Like all fungal infections, the disease requires long-term treatment, which can take about six months.
Treatment can be carried out with special varnishes, ointments, tablets in combination with traditional medicine recipes only after an accurate diagnosis has been made.
If the use of external agents does not give the desired effect, the patient is prescribed internal antifungal drugs. Since such drugs may have side effects, they should not be taken without a doctor's prescription.
As practice shows, there are cases of mold fungus when it does not respond to any treatment. Then the affected nail is removed through surgery.
Prevention of fungal diseases
To avoid onychomycosis, you must follow some rules:
● After each bath, it must be subjected to mandatory treatment with special means.
● Avoid wearing tight, uncomfortable shoes.
● Treat shoes with antifungal agents.
● Do not walk barefoot in the pool, bathhouse, sauna.
● Do not wear someone else's house shoes.
● Only personal tools should be used to care for your feet.
Don't treat yourself!
If the first changes appear on the skin of the feet or nails, there is no need to start dealing with the problem on your own. For treatment to be successful, “you need to know the enemy by sight.” Since there are different types of fungi, tests should be done, and only after an accurate diagnosis has been made, the doctor will prescribe treatment.
The most important condition for successful treatment of onychomycosis is a timely visit to the doctor and strict adherence to all the doctor’s prescriptions and recommendations.
The course of therapy must be completed to the end. Interrupted treatment can cause a relapse of the disease with further development of severe complications.