Just the mere mention of the skin disease, popularly known as “ringworm,” will make you shiver involuntarily. It probably wouldn’t even occur to you that a baby stroller left on the staircase could cause infection in a newborn. But this is, indeed, so. It’s just that a homeless sick kitten also wants to relax in a cozy and warm place.
Ringworm is a contagious skin disease caused by dermatophyte fungi (literally, growing on the skin) of two types: trichophytosis or microsporum.
It should be immediately noted that modern doctors practically do not use the term “ringworm”, because This is more of a general concept than a specific diagnosis. It is more correct to call this pathology trichophytosis and microsporia (depending on the type of pathogen). The external manifestations of these diseases are largely similar.
Microsporia and trichophytosis are widespread, and children are especially susceptible to infection.
How does ringworm infection occur?
Ringworm is transmitted through direct contact with a sick person, and you can also become infected through objects that have fungal spores on them - scissors, combs, hats, clothing and bedding. Also, various animals can be carriers of the disease: cattle, rats, mice.
You can become infected through direct contact with a sick animal, as well as through contact with wool, dust and hay infected with the fungus.
According to statistics, with the onset of autumn, the number of cases of ringworm increases, the reason for this phenomenon is the intensive period of agricultural work. Depending on the type of ringworm, the incubation period can range from 7 days to two months.
Treatment methods for lichen on the head of a child
Ringworm on the head of a child, the photo of which is given below, is a serious disease that requires seeking medical help at the first stage of development of the disease. The prognosis will be favorable, and the baby’s rehabilitation will be faster.
Medications
80% of all lichens have a fungal etiology, so treatment measures will include antifungal therapy. Depending on the type of lichen and stage, ointments, gels and shampoos with an antifungal effect are prescribed.
In severe stages (progression stage with complications), in parallel with the use of ointments, intravenous administration of antifungal agents is used (fluconazole - 100.0, 1 r / s for 5 days).
- Clotrimazole. Effectively destroys all types of fungi. Apply to the affected area of skin 2-3 r/s for 10 days. The cost of 1 tube is 30 rubles.
- Mikoseptin - aimed at combating the causative agent of ringworm. Reception up to 4 times a day, during the week. The cost of 1 package is 300 rubles.
- Acyclovir is effective for lichen with viral etiology (lichen planus, herpes zoster, Zhiber's lichen). Reception 4-5 r/s, for 2 weeks.
Shampoo "Dermazol" is used as an antifungal agent 1 r/s, up to 5 days. The cost of shampoo is 300-800 rubles. Before applying to a damaged surface, the area should be thoroughly washed and dried. To adjust the dosage, frequency of use and duration of taking the drug, it is important to consult a dermatologist.
Traditional methods
As maintenance therapy, you can resort to the use of folk remedies. For ringworm, it is advisable to use carefully ground gruel of dried sunflower seeds with sour cream.
It costs 2-3 rubles per second to use this mixture until positive dynamics appear. Treating the lesion with a mixture of iodine and vodka (1:1) will also give good results. Aloe juice has antifungal, antimicrobial and anti-inflammatory effects and will be effective for any type of lichen.
Two methods of using aloe in folk medicine are used:
- A bath filled with warm water, but not higher than 37 degrees. Add 2-3 tablespoons of sea salt (up to 50 g) to the water, with the addition of aloe extract or juice. Take such baths up to 3 times a day.
- Applying aloe juice (from ground leaves or an extract purchased at a pharmacy) to the surface of the lesion. Soak a cotton swab with the extract and apply for 10 minutes. Apply up to 3 r/s.
Other methods
Physical treatments:
- Ultraviolet therapy - improves the protective abilities of the skin, accelerating regeneration processes.
- Laser therapy of the lesion - increases metabolism in the affected area, stimulates the immune system, improving the reactive qualities of the skin.
- Electrophoresis with the use of drugs - reducing skin irritation, itching, discomfort in the area, preventing the possible spread of lichen to other points.
- Acupuncture - improves microcirculation in the damaged area, accelerating regenerative abilities.
In parallel with physiological procedures, you should often go out into the fresh air and engage in an active lifestyle. During adolescence, you should not resort to drinking alcohol and tobacco. A proper, healthy diet is recommended.
Symptoms of the disease
Superficial lichen
Ringworm of the superficial type is manifested primarily by the appearance of spots in the area of the mustache, beard and head. They do not merge with each other and have a diameter of 1-2 centimeters. Usually there are 1-2 large lesions, near which small spots are observed. Inside the spot, the skin becomes more swollen, it may peel, and in some cases itching occurs.
Bubbles or crusts with pus are observed along the outer part of the spot. In the place where the fungus has touched the scalp, hair breakage is observed. In appearance, such hairs are very reminiscent of stumps in height from 2 mm to 2 cm, on which there is a gray coating (fungal spores). If there are bubbles with liquid, then if you press on them, pus flows out. With this form of the disease, abscesses are often observed - the appearance of inflamed areas with large cavities of pus.
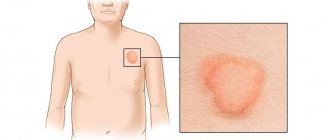
Infection with skin fungi can develop independently or occur against the background of hair damage. Ringworm is observed on an open area of the body. There are several or one spot on the skin, the diameter of which is no more than 3 cm; it has a rounded, clear shape, from which a ring gradually begins to form. The spot itself rises slightly above the surface of healthy skin. The color of the formation is pink-red. If you carefully examine the spot, there are tiny scales inside it, on which a crust quickly appears. Usually the number of spots does not exceed 1-3 pieces, and they can be on the neck, face or shoulders. In some cases, the patient complains of a slight feeling of itching.
In rare cases, lichen may be localized on the nail plate. White isolated spots are observed on the outer side of the nail plate, in this place the nail begins to crumble and soften.
Infiltrative-suppurative lichen
This type of disease differs from the superficial form in that it causes more noticeable symptoms. Often the inflammatory process is purulent and can last several months. In most cases, infection occurs from animals; it is believed that this disease is often found in livestock farmers. The spots in this case are red-blue in color and are observed in the area of the mustache, beard and on the head.
Erosion is observed inside the spots, hair follicles begin to become inflamed, and hair in the affected area begins to weaken, break and fall out. Inside each hair follicle there is pus. On the skin, such spots look like festering plaques; the pus causes the death of fungi, which can only be seen on the outer part of the round spot.
The mechanism of development and varieties, photos, how to recognize the disease
The basis of the pathology is parasitism of the fungus in vegetative forms. This is mycelium, which is thin threads. Organisms live and develop in the intercellular space of hair, skin, and nails.
Based on the localization of the infectious process, the following types of disease are distinguished:
- hair microsporia. Hair is affected: the fungus is located directly in the hair structure under its cuticle. Due to this, the hair is destroyed and breaks off, hence the name “cutting”;
- skin microsporia. The fungus is found in the top layer of the skin;
- microsporia of nails. The mycelium is located in the horny substance of the nail plate. This form is very rare;
- pustular form. It is quite severe, and the mycelium penetrates into the deeper layers of the skin and provokes inflammation along with the appearance of pus.
Ringworm in children most often manifests itself as a fungal infection of the hair with characteristic symptoms.
Ringworm is more common among children. It mainly affects the part of the head covered with hair or smooth skin.
Spots appear on the head , covered with white scales of different sizes. The hair loses its shine, breaks off at the level of 4-8 mm, leaving characteristic stumps.
Nails are rarely affected. As the pathology develops, they begin to exfoliate, crumble, and their color becomes gray.
If the lesions are located on the skin, nodules appear, which over time transform into large or oval spots covered with crusts or scales.
Photo of the initial stage of ringworm on the head:
Photo of ringworm on a child’s body:
Symptoms include mild itching. There is no inflammation, except in cases where a child gets an infection through scratching.
If the immune system is weakened, the disease can be severe. Then symptoms such as high fever and swollen lymph nodes are possible.
If the skin is severely affected, the disease enters an advanced stage. Complete hair loss and the appearance of severe scars are possible.
The following symptoms are alarming. If you notice them in your child, you need to go to the doctor :
- the appearance of pinkish-red spots on the head with clear or smeared edges;
- peeling spots, severe dandruff;
- deterioration of hair condition, dryness, fragility;
- itching that causes the baby to constantly scratch.
Disease detection
Ringworm can be determined through diagnostics, which consists of taking an anamnesis, visual examination, instrumental and laboratory testing. Laboratory research involves cultural and microscopic methods. When examining scales affected by a fungal infection under a microscope, you can see mycelium - twisted threads of mycelium.
When conducting a microscopic examination of hairs affected by the fungus, you can see their clear boundaries; inside the hair there are large fungal spores, which are parallel to longitudinal chains. The presence of a fungal infection can be determined using the cultural method 5-6 days after sowing.
Treatment of ringworm
In any case, prevention of ringworm is better than its treatment, but if infection occurs, then you need to know how to cope with the infection. It is prohibited to treat ringworm on your own. In this case, it is better not to joke with mushrooms, since improper treatment can be very expensive. Only correct treatment prescribed by a doctor can achieve truly good results, especially since in modern conditions it is quite simple to cope with a fungal infection. In the treatment of ringworm of smooth skin, without the disease affecting vellus hair, antifungal external preparations are used: iodized tincture, sulfur-tar, sulfur-salicylic or sulfur ointments.
Modern antifungal drugs are also very popular in the treatment of ringworm. If there are numerous lesions on the skin, especially if the disease has affected the hair, it is recommended to use antifungal drugs for several weeks. In this case, the hair must be completely shaved. If there is an inflammatory process, the patient is prescribed combination drugs.
If a fungal infection has affected vellus hair, then it is necessary to do hair removal with detachment of the stratum corneum. It is recommended to carry out such detachment 2-3 times.
If the disease is in infiltrative-suppurative form, it is recommended to remove the crusts using a scalpel.
Features of treatment for children
Treatment of versicolor in children is aimed at destroying pathogenic flora and accelerating the exfoliation of affected epidermal cells. When diagnosing keratomycosis in the initial stages, they are limited to treating the skin with antimycotic and keratolytic agents. Medicines of the first group destroy the infection, and the second stimulate the exfoliation of epidermal cells.
Oral preparations are used for the rapid spread of pityriasis-like spots on the body and severe cases of lichen. Also, systemic therapy is carried out for persistent exacerbation of infection against the background of secondary immunodeficiencies. To prevent exacerbations of tinea versicolor, immunostimulants are prescribed.
Medications
Pityriasis versicolor in children is treated with local antimycotic agents. They do not have a toxic effect on the liver and rarely provoke adverse reactions. The basis of local antifungal therapy for lichen is:
- Bifosin is a fungicidal agent in the form of a spray, ointment and solution that has antifungal activity. Apply to problem areas no more than 1-2 times a day. The course of therapy is no more than 14-20 days.
- Terbix is an antimycotic spray (cream) that quickly destroys fungal infections in the skin. Children over 12 years of age are recommended to use the drug no more than 2 times a day for 2 weeks.
- Ketoconazole is an antifungal cream that has an antipruritic effect. Apply to flaky spots and 2 cm of healthy skin around them up to 2 times a day.
- Exoderil is a naftifine-based cream that has antifungal activity against dermatophytes, yeast and mold fungi. Apply to pre-cleaned fabrics once a day.
When spots appear on the head, use Nizoral, Perhotal, Keto-plus or Mycozoral shampoo. The following are used as keratolytic (exfoliating) agents for pityriasis versicolor: Betasalik, Retasol, Skinoren.
This lichen is caused by a fungus, so an antifungal therapeutic course is prescribed.
In case of severe pityriasis versicolor, systemic antimycotics are included in the treatment regimen:
- Rumicosis - broad-spectrum antifungal tablets. Children under 12 years of age are prescribed 100 mg of medication per day for 7 days. If there is no positive effect, treatment is extended for another 3-4 days.
- Itrazole is an antimycotic drug that destroys mold and yeast-like fungi. For lichen, 200 mg is prescribed once a day for a week.
- Mycozoral is an antifungal tablet that destroys the cellular structures of dermatophytes, dimorphic and yeast-like fungi. Children weighing over 30 kg are prescribed 1 tablet per day for 3 days. If there is no positive dynamics, the dosage is increased by 2 times.
For severe itching, take antihistamines - Suprastin, Claritin, Parlazin. In case of decreased immune defense due to hypovitaminosis, children are prescribed vitamin and mineral complexes with retinol - Pikovit, Alphavit, Complivit.
Dietary recommendations
Opportunistic fungi reproduce only when the body’s protective properties decrease. Often it is vitamin deficiencies and hypovitaminoses that negatively affect tissue reactivity and the body’s ability to resist infections. Therefore, to increase immunity in a child with lichen versicolor, it is recommended to consume foods with vitamins:
- lean meat;
- honey (in the absence of allergies);
- barley;
- fresh vegetables;
- red fruits;
- homemade yoghurts;
- berries;
- celery.
To create conditions unfavorable for fungal flora, the following are excluded from the menu during treatment:
- confectionery;
- rich meat broths;
- fatty fish;
- fast food;
- smoked meat;
- conservation.
Among drinks, preference is given to dried fruit compotes, natural fruit and vegetable juices, milk, and green tea. To normalize the functioning of the gastrointestinal tract, it is advisable to refrain from drinking soda and strong coffee.
ethnoscience
Before treating pityriasis versicolor in a child with alternative medicine, you should consult a pediatrician or dermatologist. Ointments, decoctions and compresses based on honey, medicinal herbs and other highly allergenic ingredients can cause inflammation and other adverse reactions. To prevent them, the prepared product is first applied to healthy tissue and left for 1-2 hours. Only if there is no redness, rash or itching, use it to treat multi-colored spots.
Tinea versicolor is a recurrent disease, so it is important to eliminate the factors that provoked its occurrence, carry out thorough cleaning with disinfectants, and thermally treat clothes and bedding.
In the fight against lichen, herbs and products are used that have pronounced antifungal, keratolytic and regenerating properties. To speed up the healing process, use:
- St. John's wort ointment. In 1 tbsp. l. baby cream or Vaseline add ½ tbsp. l. St. John's wort herbs. Apply a thin layer of ointment to multi-colored spots 3-4 times a day. Treatment is continued until the external symptoms of pityriasis versicolor disappear.
- Sorrel ointment. Crushed sorrel is mixed with heavy cream and 3-5 drops of essential oil. Apply to stains and wrap in polyethylene. After 1.5 hours, wash off the remaining product. In case of exacerbation of deprivation, the procedure is performed 2-3 times a day for 2 weeks.
- Herbal ointment. Mix 2 tbsp. l. calendula, hop cones and crushed burdock root. Pour the herbal mixture into 300 ml of water and boil for 3-5 minutes. Add 100 g of Vaseline and licorice powder to the decoction. The ointment is used to treat colored spots no more than 3 times a day for 2 weeks.
During periods of exacerbation of tinea versicolor, folk remedies are combined with antifungal ointments or creams. If there is no effect or allergic reactions, you should stop using herbal ointments.
Prevention of ringworm
If one of the family members has become infected with ringworm, it is recommended to disinfect objects that have previously been in contact with the sick person. The patient should not have contact with other relatives until he has fully recovered.
It is imperative that all people in contact with the patient undergo examinations, as well as pets, if they have them, since they are often the source of infection.
To exclude primary infection with ringworm, it is recommended to undergo periodic medical examinations in kindergartens and schools, and to handle animals with extreme caution.
Ringworm in children
Most often, a child becomes infected with ringworm as a result of contact with a sick animal. In most cases, pets - rabbits, guinea pigs, dogs and cats - act as the source of infection. Any of these animals may be infected with one or even several types of fungus. It is also interesting that in order to become infected with lichen, it is not at all necessary to touch a sick animal; it is enough to come into contact with objects or fur.
Most often, transmission of trichophytes occurs from a sick person to a healthy person. Animals are the second most important source of fungal infection transmission, but children often become infected from animals in rural areas. In this case, the causative agent of lichen is often microsporum.
Symptoms of lichen in children
The manifestation of the disease in children directly depends on its form and the fungus that caused the lichen. Almost always, children experience superficial trichophytosis in the scalp area. It is because of this shape that ringworm was able to get its name. The reason is that the disease often affects the hair on the head, which begins to break at a height of 1-2 mm. In appearance, the manifestation of the disease resembles simply hair cut bald. It is for this reason that this type of lichen is called “ringworm”.
In addition to hair, the disease damages the skin under the hair. There are lesions that have a round shape and unclear boundaries. Lichen scales are also observed on such spots. In most cases, the patient has several foci of the disease, although in rare cases the formation may be single. In some cases, crusts, blisters and pustules are observed at the border of the formation.
It is also interesting that children often do not experience the symptoms characteristic of lichen - discomfort, pain and itching. As a result, the fungal infection begins to quickly spread to healthy areas of the skin. Subsequently, with the onset of puberty, women experience a transition of the disease into a chronic form, and men experience self-healing. In all likelihood, this feature lies in the hormonal balance, which is radically different in women and men.
What medications are used to treat ringworm?
The following drugs have a therapeutic effect on ringworm:
ointments
- sulfuric - has a drying and healing effect;
- sulfur-tar - has an antifungal and disinfectant effect;
- salicylic - has antifungal and anti-inflammatory effects;
- Lamisil - stops the growth of fungi; applied for 5-6 weeks;
- mycosporus - destroys fungal cells; applied for 4-6 weeks;
gels
- exifin - applied 1-2 times a day, rubbed until completely disappears from the surface of the skin; applied within 3-4 weeks;
- mycogel - applied 2 times a day in a thin layer; applied within 3-4 weeks;
solutions (convenient for use on the scalp)
- Vokadin is an antifungal and bactericidal drug;
- iodicirin - promotes rapid healing and detachment of scales;
- nitrofungin is an antifungal drug used until the symptoms of the disease completely disappear;
tablets - have a systemic effect, are highly effective, however, they also have a number of side effects; used in case of presence of several foci of ringworm
- griseofulvin - take 8 tablets per day with meals with a teaspoon of vegetable oil until the first negative test, then the dose is reduced and the drug is gradually discontinued;
- Lamisil - taken 1-2 times a day for 6 weeks;
- orungal - taken 100 mg once a day for 15 days.
Before applying medications to the skin, it is recommended to clean the damaged areas; for this, use:
- furatsilin,
- rivanol,
- potassium permanganate.
Treatment of lichen in children
Any type of fungus is characterized by a long period of therapy, so ringworm is no exception. Thanks to the availability of modern medications, it becomes quite simple to cope with any fungal infection. But as a result of the specific location of the fungus on the skin, which has extremely low permeability, the duration of therapy may take several weeks or more.
The main treatment for microsporia and trichophytosis is griseofulvin. This drug is used orally in the amount indicated by the treating doctor.
It is necessary to take the remedy until complete recovery. Also, against the background of tablets, it is recommended to use local agents - ointments and creams, including bifonazole, isoconazole, ketoconazole.
Recently, antifungal antibiotics with a powerful effect have been very effective - fluconazole (Flucostat), terbinafine (Lamisil, Terbizil) and itraconazole (Itrazol and Orungal). Medicines are highly effective in treating children. The main advantage of such medications is that they can be taken orally without the need for local permanent treatment of areas of skin or hair affected by ringworm. The only drawback of such drugs is that the cost of treatment will be very high, but the result will not be long in coming.
Speaking about the effectiveness of drugs, first of all you need to look at the speed of disappearance of the manifestations of ringworm. For this purpose, a special Wood lama is used, with the help of which the patient is examined. In addition to treating a sick child, all people in contact with him should be examined for the presence of the disease. If the disease is found in other people, treatment should be started without delay. You can also take pets for examination by a veterinarian if there is a suspicion that the child became infected from him.
Local treatment of dermatomycosis
As mentioned above, complex therapy includes the parallel use of tablets and local agents. Ointments, gels and solutions act differently, depending on the active substance and dosage. The ointment has a thick consistency, is deeply absorbed into the skin and remains on it longer. This remedy is most effective in severe forms of the disease. Ointments are combined with iodine, which can disinfect the skin, dry and kill bacteria. In the morning, foci of lichen are lubricated with iodine, in the evening - with antifungal ointments.
Conclusion
Despite the fact that ringworm does not cause tragic outcomes, it can create many problems, especially for children.
A child suffering from lichen may turn out to be a real outcast in society, so treatment should be carried out carefully, without self-medication. An error in the selection of a medicine, the timing of its administration or the dosage can cause an even greater spread of the disease, which will certainly affect the moral and physical condition of the patient.
Only compliance with all the rules given by a qualified dermatologist will allow you to quickly get rid of the disease, returning the child to society completely healthy.