Irritation
It appears as an itchy red rash, slightly raised above the skin. Appears when shaving and hair regrowth. A reaction may also occur to detergents and cosmetics, washing powder, and clothing made from synthetic fabrics.
To relieve irritation, use ointments and gels with a soothing or cooling effect. For prevention, you should moisturize, soften and disinfect the skin after shaving. You need to remove hair with a sharp instrument or choose another method of depilation. And you should not use products that cause allergies.
Pseudofolliculitis
Simply put, ingrown hairs. They appear due to hardening of the skin, through which the rods cannot penetrate. It can also be caused by very fine or curly hairs. Girls who prefer to remove vegetation from the roots are more often exposed to the problem. As a result, they develop a small rash on their legs.
The pimples are painful, with the tip of a hair or a small loop visible inside them. The rods are removed manually using tweezers or a needle. Antiseptic treatment of instruments and skin is mandatory.
Types and classification of diseases
According to the international classification of diseases, skin lesions can be divided into the following groups:
- infectious. These include various rashes and neoplasms of infectious origin (boils, abscesses);
- transmitted “inheritedly” (genetic). The most common disease in this category is psoriasis;
- autoimmune;
- neurotic (caused by stress and constant emotional manifestation);
- allergic;
- parasitic.
A separate category includes various tumors - melanomas, moles. Each of these groups of foot skin diseases requires specific treatment.
It is also necessary to understand that some of the lesions are temporary and, with well-chosen treatment, go away within 8-10 days, while others are chronic and it is impossible to get rid of them forever.
Mycosis
Today, foot fungus is the most common skin lesion that occurs on the legs. Experts assure that representatives of the stronger sex most often suffer from this disease, but in women such a disease is diagnosed extremely rarely.
There is a common misconception that foot fungus is a consequence of poor personal hygiene, but doctors say that this assumption is wrong.
Mycosis appears due to the constant wearing of closed and tight shoes, which serves as a favorable environment for the proliferation of pathogenic microorganisms.
Foot fungus progresses quite quickly and in most cases is accompanied by the following symptoms:
- the appearance of peeling (the skin may peel off in entire layers);
- thickening and roughening of the skin on the feet;
- itching and burning;
- formation of microcracks.
Doctors warn that getting rid of the pathology on your own may not be as easy as it seems. To overcome the fungus, the approach must be comprehensive.
The patient will have to not only use external products, but also make various compresses and take medicinal baths. In advanced situations, the doctor may prescribe medications for oral use.
Reference! Mycosis is an infectious disease that can be transmitted from person to person through physical contact and through the use of household items.
Interdigital infection
The lesion is also fungal in nature; in contrast to foot fungus, destruction of the epidermis is observed only in the area of the toes. The disease is infectious and most often spreads in baths, saunas, gyms and swimming pools. Main features:
- peeling of the skin between the fingers;
- skin redness;
- severe burning sensation;
- the formation of small blisters with liquid inside.
In the absence of timely treatment, the disease quickly begins to progress and spread to other areas of the skin.
Psoriasis
This chronic disease occurs in both adults and children. Doctors warn that it is impossible to completely get rid of psoriasis; in any case, the disease will periodically worsen.
The main symptom of this lesion is the uneven appearance of rash and redness in different areas of the skin. Psoriasis can affect not only the feet, but also the lower legs, knee joints and nail beds.
In some patients, such rashes begin to unite, resulting in plaques with white or grayish scales forming on the skin. Externally, psoriasis resembles eczema or mycosis. To make an accurate diagnosis, you need to visit a doctor and undergo a full diagnosis. The following symptoms are typical for psoriasis:
- severe itching;
- swelling of the affected areas;
- splitting and brittleness of nails;
- the appearance of a papular rash during a calm period.
The treatment regimen is selected taking into account the development and degree of the disease, but the patient in any case will have to take both internal and external agents.
Neurodermatitis
An allergic disease that is inherited. Experts assure that the patient’s nervous and emotional state plays a major role in the course of the disease.
If a person constantly worries about problems in his personal life or difficulties at work, the likelihood of an exacerbation of the disease increases, which can last more than several months.
Neurodermatitis has 2 forms:
- limited. It mainly affects the lower extremities, the rashes are often localized under the knees;
- diffuse. This form of the disease is considered more severe, with sores with a scaly surface, blood crusts and multiple cracks appearing on the skin of the legs.
Useful article “The drug Venoruton: instructions for use.”
Athlete's foot
Also refers to fungal diseases that affect the skin of the feet and nails.
Since high humidity is favorable conditions for the development of the disease, the likelihood of occurrence increases if a person works in a bathhouse, gym, or sauna.
The disease is considered very contagious; when it comes into contact with the skin of a new host, the fungus begins to multiply intensively.
Unlike other fungal infections, signs of epidermophytosis do not appear immediately and are mixed, which is why the patient may not be aware of the development of the disease.
In the first stages, the disease is accompanied by slight itching and mild peeling. But in the absence of timely treatment, the lesion begins to progress, cracks, crusts and ulcers appear on the patient’s skin.
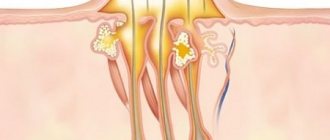
Folliculitis
Inflammation of the hair follicle under the influence of pathogens. Skin damage and excessive sweating may also be a cause. First, red spots appear on the legs, which become denser over time.
Then pus forms inside the growth. Treatment consists of antiseptic treatment of the affected areas. You can carefully squeeze out the purulent contents, not forgetting to disinfect your hands and pimples. Large boils should be addressed to a surgeon.
Fungal infection
The feet are most often affected by fungi. Some types of microorganisms prefer to settle in the groin area. Overweight people may develop a rash on their legs above the knee due to friction and excessive sweating.
The lesions are usually localized on the inner thighs. The affected areas appear as red or pink spots with blisters and bumps along the outer edge. The skin itches and hurts. Antifungal ointments and antimycotics for oral administration are used as therapy.
Rash on legs photo
Acrodermatitis
Inflammation of the skin localized on the lower part of the leg. It occurs under the influence of pathogenic bacteria that enter the body after a tick bite. The disease can also be triggered by metabolic disorders or weakening of nerve impulses.
Specific symptoms depend on the type of disease. Usually, purulent or watery rashes appear first on the toes, which then spread to the ankle. In rare cases, the lesions rise higher in the limb. The skin swells, there is pain, itching and burning. Each type of pathology requires special treatment under the supervision of a doctor.
Why do my feet itch?
If your feet itch day and night, the cause may be a dermatological type of disease. To understand how to treat them, you need to pay attention to the symptoms.
The skin of the feet needs daily care. Dry feet can cause itching. In cold weather, women apply moisturizer to their hands. So the feet also need care. If this is not the problem, you should visit a specialist.
If you want to scratch your leg, you should keep in mind that every scratching is an injury to the upper layers of the skin. No matter how long the itching continues, it is better to find the cause and begin treatment than to introduce infections into the scratched areas.
Itching on the feet, upper legs, and rashes on the palms can be caused by many reasons, the treatment of which should be entrusted to a certified specialist.
Phlebeurysm
Stretching and deformation of the venous walls. The causes of the pathology include blood clotting disorders and vascular damage. The disease may be genetically determined. In the initial stages, patients note swelling and heaviness in the legs.
There is pain, discomfort and burning. The legs become covered with red spots due to dilated capillaries. Spider veins gradually form. In severe cases, venous tubercles bulge, and the entire skin becomes covered with bluish spots.
Venotonics are used for treatment. Wearing compression stockings and lymphatic drainage are helpful. In advanced cases, surgery is indicated.
What is itchy feet
Itchy feet is a symptom that can occur in all age groups and affects both men and women equally. Often associated with non-pathological conditions and tends to resolve quickly.
In other cases, it is combined with other disorders and lasts for 2-3 days, in this case it may be a manifestation of a pathological condition of the skin or the whole body, in such cases it is always useful to consult a doctor.
Varicose dermatitis
Complication of varicose veins. The pathology begins with redness and itching just above the ankle. The skin becomes smooth and shiny. Then bubbles with liquid appear on it, which disappear without a trace on their own.
Gradually the epidermis darkens, the itching spreads throughout the leg. Watery pimples do not go away. After opening, erosions remain in their place, which over time degenerate into ulcers.
Treatment involves restoration of the veins and external treatment of the affected areas with ointments containing corticosteroids. When an infection occurs, antibiotics or antifungals are needed.
Methods of therapy
Since dry eczema on the legs is a chronic disease, its treatment requires a long period of medical manipulation and complex effects. The patient will require drug therapy, lifestyle and nutritional adjustments, as well as proper skin care, paying special attention to the affected areas.
Drug treatment
Drug therapy for eczema on the legs involves taking drugs orally and local treatment.
For oral administration the following are used:
- Antihistamines. They help eliminate discomfort - itching, as well as allergic manifestations of pathology. The most commonly used: Fenistil, Zodak, Loratadine, Fexadine, etc.
- Sedatives. These drugs are prescribed for the neurological form of the pathology, that is, when the cause of the rash is frequent stress, anxiety, depressive and psychological disorders. Most often, herbal-based medications are used (Novopassit, Persen, Notta, etc.). For more severe forms of the disease, tranquilizers and antidepressants are prescribed, which are sold in pharmacies only with a doctor's prescription (Pyrazidol, Amitriptyline, Diazepam, Trimipramine, etc.).
- Antibacterial agents. They are prescribed quite rarely for this form of the disease. Most often this occurs when a secondary infection occurs, that is, pathogenic microflora enters the damaged plaque. These include: Amoxicillin, Moxifloxacin, Tetracycline and other broad-spectrum antibiotics.
- Antifungal agents. It is used when fungal microflora is attached. For this, Binafin, Irunin, Candide and others are used, which are selected from the damaging microflora.
- Sorbents and enzymes. To normalize the functioning of the gastrointestinal tract, various drugs are prescribed. Sorbents: Polysorb, Polyphepan, Chitosan, Enterosgel, etc. Enzymes: Festal, Enzistal, Creon, Ermital, etc.
- Corticosteroids. They are prescribed for fast and effective pain relief. The most commonly prescribed: Prednisolone, Triamcinolone, Florinef and others.
- Vitamin complexes. Multivitamins and immunomodulators are used to strengthen the immune system. The most popular immunoboosting drugs: Viferon, Reaferon-EC, Genferon, etc. Vitamin complexes can be used from both domestic and foreign production: Alphabet, Complivit, iHerb, Velmen, etc.
In addition to taking various medications internally to promote speedy recovery and recovery, external agents are used.
- In the initial stage of pathology development, it is necessary to use moisturizers, which include lactic acid, petroleum jelly, and glycolic acid.
- With further spread of the pathology and its transition to the next stage, the use of creams, ointments and pastes for hormonal or corticosteroid purposes is necessary. The most commonly used ointments are prednisolone or pydrocortisone, Soderm, Advantan, Elokom, Lokoid. At the same time, the patient should know that corticosteroid ointments thin the skin and reduce their immune status. These products can only be used as prescribed by a dermatologist and strictly in the prescribed dosage, since the drugs have a number of side effects, despite their high effectiveness.
- Non-hormonal external agents are also used. These are mainly Skin-Cap, Dermasan, Aurobin. Aurobin can be used at the initial stage of pathology development. Dermasan is effective in more advanced cases, but it is contraindicated in breastfeeding and pregnancy, or in the presence of open wounds and ulcers. Skin-Cap has a wider spectrum of action; it can be used at any stage of pathology development and for all categories of persons.
Fenistil is a remedy for the treatment of dry eczema on the legs.
For healing and drying (if cracks and weeping wounds appear), it is recommended to use zinc ointment. This remedy has a limitation: it cannot be used for acute purulent processes, as well as for increased allergic reactions.
Diet therapy
Proper dietary nutrition plays an important role in eczema, which includes avoiding certain foods. Patients need to reconsider their lifestyle, giving up bad habits such as smoking and drinking alcoholic beverages, which only aggravate the patient’s condition. The following products are prohibited:
- red vegetables and fruits;
- citrus fruit;
- chicken eggs;
- sweets;
- fresh baked goods;
- chocolate;
- caffeinated products;
- smoked meats;
- pickles;
- spices;
- spicy foods;
- fatty food.
It is better to prepare food just before eating, and the cooking method should be gentle - boiling, steaming, stewing, baking. If you follow the right diet, it is easier to get rid of itching and other uncomfortable sensations.
Folk remedies
In addition to the above treatment methods, you can turn to alternative medicine. However, this can only be done after consultation with a specialist who will not object to such an addition.
There are several recipes that help well with dry eczema of the extremities:
- Celandine ointment. Fresh celandine leaves are thoroughly washed and dried, after which they need to be crushed and mixed with petroleum jelly and lanolin in a ratio of 2:1:1. This ointment should be used at least three times a day, applied to the affected areas of the skin.
- Compresses with coltsfoot. Coltsfoot is ground in a blender or meat grinder, and then mixed with fresh milk. The resulting mixture is applied to the affected areas, wrapped in film on top and secured with a bandage or clean cloth. Use until stable remission.
- Infusion of yarrow and calendula. Take plant flowers in equal quantities (40-55 g each) and pour a glass of boiling water. Leave to infuse for 2-3 hours. Afterwards, the infusion is filtered and consumed 3-5 times during the day.
Hemorrhagic vasculitis
If the rash on your legs does not itch, it may be due to inflammation of the subcutaneous vessels. Pathology occurs due to infection by pathogenic microorganisms. The clinical picture consists of the appearance of dark red spots on the buttocks and lower extremities.
When pressed, the pigmentation does not change shade and does not disappear. For treatment, ointments with anticoagulants are used. It is also necessary to eliminate the source of infection using antibiotics and antivirals. In some cases, cytostatics are prescribed.
A rash on the legs spoils the appearance and sometimes causes serious physical discomfort. It can be a sign of not only skin diseases, but also pathologies of the circulatory system and the musculoskeletal system.
Some problems are easy to deal with on your own. In some cases, medical attention is required. Fortunately, the most dangerous rashes look specific and are difficult to miss.
Trophic ulcers on the legs: treatment and photos
Trophic ulcer is a disease caused by the rejection of dying tissue, resulting in an open wound of the skin. Such an ulcer develops in parallel with other diseases, such as varicose veins, eczema, and venous insufficiency. This disease usually affects the lower extremities. You can see what trophic ulcers on the legs look like in the photo; the initial stage has pronounced symptoms.
Quick and effective treatment of trophic ulcers on the leg What foods thin the blood and prevent thrombosis? Treatment of trophic ulcers of the lower extremities Quick and effective treatment of trophic ulcers on the leg What foods thin the blood and prevent thrombosis?
Signs and symptoms
Fungal infection of the big toe is accompanied by more striking manifestations. For example, the nail has an uneven structure and yellow-gray spots.
Moreover, a person may feel pain due to the formation of microcracks that do not heal for a very long time. If you notice a fungus on your feet, you should immediately contact a dermatologist.
Since it is necessary to determine the cause of this formation in order to prevent recurrence. Only a specialist can prescribe high-quality and effective treatment.
- From the side of the hair: hair fragility, dandruff, hair loss, etc.
- From the sides of the nails: changes in the color of the nails, their thickening and fragility, etc.
- From the side of the skin itself: itching of the skin begins, the skin will peel off, red spots, age spots, acne, pimples will begin to appear, the skin will become oily, etc.
There are different types of human skin diseases. We list the main ones:
- Dermatoses, dermatitis - manifest themselves as inflammatory processes of the skin, manifested by swelling and redness of the skin, the appearance of blisters on it;
- Neurodermatitis (or atopic dermatitis) is a neuroallergic skin disease that causes rashes and itching of various parts of the body;
- Eczema is one of the most common skin lesions of the human skin, characterized by vesicular rashes and peeling;
- Psoriasis - manifests itself as scaly lichen, is a non-contagious disease of the human skin. Rashes and small scales appear on the skin;
- Onychia (candidal paronychia) - nail fungus - is one of the types of skin lesions. Mainly found in the female half of the population, this type of disease manifests itself as a result of local trauma, as well as moisture in the skin. These factors especially often affect the hands of cooks, laundresses, housewives, and confectioners.
Yeast nail fungus
When the interdigital folds on the feet are affected, the following is observed:
- slight peeling of the skin of the legs;
- small cracks between the toes;
- burning sensation, pain and itching;
- feet sweat excessively;
- the feet become hard and compacted;
- toenails change appearance: they peel, become covered with yellow and gray spots, which grow over time.
At the initial stage of the disease, the feeling of discomfort and itching is mild, so many do not pay attention to these first warning signs. However, ignoring the symptoms of mycosis leads to the fact that after some time the disease progresses and affects the nails, which begin to peel, change their natural color and thicken.
The risk of fungal diseases especially increases during the use of antibiotics and with diabetes mellitus. If skin lesions on the legs are detected in a timely manner, it will be easy to cure the fungus.
However, you need to be prepared for the fact that the treatment takes a long period, so it will be possible to get rid of the fungus only in a month or much later, when the fungal infection is completely cleared from the body and the blood is cleared of microorganisms.
If the disease has spread to the nail plates, it will be possible to completely recover from the fungus between the toes only after twelve months.
Therefore, when identifying the first signs of the appearance of a fungus, it is important to seek the help of a doctor who will examine the lesion, examine skin particles in the laboratory, identify an accurate diagnosis and draw up a treatment regimen.
The main thing in this case is not to neglect it, otherwise the damage may spread to other parts of the body and treating the fungal infection will be much more difficult and longer. You can learn more about what nail onychomycosis is: treatment, symptoms and photos of this disease from the information on our portal.
Fungal infections often affect the toes, which results in constant itching and significant cracks in the skin of the feet. The fungus can be cured using ointments, tablets and folk remedies. There are also preventive measures to protect against the disease and relapse.
Eczema in the legs, which occurs in the acute stage, is accompanied by redness of the skin and the formation of small reddish nodules on the toes. These formations increase in size and then fill with liquid.
Symptoms of the disease
The following signs of the initial stage of a trophic ulcer on the leg occur:
the appearance of swelling in the legs;
What does the disease look like in the initial stage (see photo)? The appearance of seizures begins to be accompanied by visual changes. The skin on your legs begins to change color, turning blue or purple. Increased moisture appears in the legs as a result of the passage of lymphatic fluid through the skin. Over time, the resulting wound begins to fester.
It is important to know! If a regular wound on the leg does not disappear within 1 month, it is a trophic ulcer! You need to immediately contact a specialist who will find out the cause of the disease and prescribe the correct treatment.
Some useful tips
Leg pain that doesn't go away? The damaged area of the body will heal much faster if it is carefully treated immediately after the injury has been sustained. Particularly severe cases require qualified assistance from medical professionals who will apply stitches if necessary and help the victim with valuable advice and useful recommendations.
If there is no qualified specialist nearby, then to treat the damaged area of the body it is recommended to use any antiseptic agents that are at hand: brilliant green, iodine, hydrogen peroxide, etc. After treatment, the wound should be covered with a temporary sterile bandage. You need to bandage damaged areas at least 2 times a day and remember that you need to use different products to treat wet and dry wounds.
Causes of the disease
The following factors can serve as prerequisites for the disease:
- disorders in arterial and venous circulation;
- diabetes;
- mechanical effects on the skin, trophic ulcers of the lower extremities can cause burns or frostbite;
- poisoning with highly toxic substances;
- dermatitis, eczema;
- deterioration of local blood circulation as a result of prolonged immobility.
Important! When establishing a diagnosis, the disease that caused the ulcers plays a very important role! This way, the specialist will be able to prescribe the correct treatment.
Types of pathology
Various diseases occur in the lower extremity area. They can be infectious-inflammatory, allergic, toxic, neurotrophic or other in nature. The most common pathology on the legs is:
- Dermatitis and dermatoses (eczema, neurodermatitis).
- Mycoses (athlete's foot, onychomycosis).
- Plantar warts.
- Trophic ulcers.
- Psoriasis.
- Erysipelas.
Of course, the skin of the lower extremities can be affected by other diseases, for example, pyoderma, scabies, secondary syphilis, and tumors. The range of possible disorders seems to be very wide, but a pathology that has become widespread requires careful consideration.
Types of trophic ulcers on the legs
Depending on the cause of the disease, there are the following types:
Arterial
This type of lesion occurs due to atherosclerosis, which disrupts the functioning of the main arteries. The cause of development is usually severe hypothermia, even frostbite. The location of the ulcer is most often the foot area, big toe, heel. A person is constantly cold, quickly overtired, and the affected leg begins to hurt at night. If this type of disease is not treated at the initial stage, the resulting wounds begin to spread throughout the foot and fester.
Venous
Usually appear on the inside of the lower leg. The occurrence is associated with a complication of varicose veins. What does a trophic ulcer look like in the initial stage? The initial stage is accompanied by swelling of the calf, the appearance of cramps at night, a venous network is formed, and the color of the skin changes. If treatment is not started, the disease will progress and affect not only the skin, but also tendons and muscles. Pus with a pungent odor begins to ooze out. Incorrectly chosen treatment can lead to more severe illnesses.
Diabetic
Diabetes mellitus causes many concomitant diseases, including diabetic ulcers. The initial stage is characterized by the death of nerve cells, as a result of which the sensitivity of the legs is lost. Mostly the big toes are affected. The danger of this type of disease lies in susceptibility to various types of infections, as a result of which gangrene can develop, followed by amputation.
Neurotrophic
The appearance is caused by severe injuries to the head or spine. The lateral surface of the foot is most often affected. The size of the formation is small in appearance, but very deep. The wound begins to fester rapidly.
Symptoms of manifestation
Dry eczema has the following symptomatic manifestations:
- increased dryness of the skin;
- feeling of skin tightness;
- the appearance of hyperemic areas that indicate inflammatory processes;
- coarsening and roughness of the skin;
- severe itching that bothers the patient, especially at night, which can result in insomnia;
- characteristic rashes appear on the skin, which gradually grow and form eczema plaques;
- In the absence of treatment or its ineffectiveness, cracks appear on the plaques, which cause pain;
- The last stage of the pathology is characterized by weeping wounds, from which blood and ichor can ooze, drying out and forming easily traumatic crusts.
Most often, the process begins with dryness and flaking of the skin. Gradually, the feeling of itching increases, the inflammatory process on the skin begins and wounds appear. The development of dry eczema on the legs is very slow and the feet are always affected.
Treatment of the disease
How to treat the resulting wounds? The fight against the disease is divided into 3 stages:
- Conservative treatment. Treatment of an initial stage trophic ulcer consists of eliminating the symptoms of the disease. For this, the following drugs are used: Actovegil, Tocopherol, Solcoseryl and their analogues.
- Local treatment. First, you should act on the disease that was the cause of the damage to the lower extremities. Treatment should then be directed towards eliminating the infection, getting rid of dead tissue and addressing the wound. For such measures, antibacterial drugs (Furacilin, Chlorhexidine), broad-spectrum antibiotics, anti-allergenic medications (Suprastin, Tavegil), compresses with medicinal ointments (Levomikol, Dioxikol) are used.
- Surgical intervention. The indication for this type of treatment is the widespread spread of ulcers along the lower extremities with a high degree of severity. The operation involves the elimination of the ulcer and surrounding necrotic tissue. The second stage involves surgery on the veins.
Important to remember! Surgery can be avoided thanks to a quick response at the initial stage of the disease!
Treatment
Today there are many methods and methods for treating interdigital fungus. In addition to drug treatment of the disease, special ointments and creams against fungus are used, which can be found in any pharmacy.
But there are proven folk recipes that you can use at home without danger to your health. Any treatment option must be discussed with the treating doctor, as contraindications are likely.
Interdigital fungus is quite easy to cure, but it will take a lot of time. The approximate course of treatment for interdigital fungus is about one year. This can be explained by the fact that the interdigital folds are an excellent environment for the reproduction and development of pathogens. High humidity is constantly maintained in the skin folds.
Drug treatment
It is better to find out how to cure fungus between the toes from your doctor, since he is the one who can examine the infection and scrape it. It is strictly forbidden to ignore painful symptoms, as the disease is likely to spread to other skin areas, for example, the abdomen, buttocks or arms.
Thanks to the huge variety of special medications, the patient can choose the most optimal remedy against fungus on the fingers. In addition, they have different courses of treatment.
Certain ointments require two weeks of use, while some can be used once. When the skin humidity is high, it is necessary to use ointments and gels with a drying effect.
The cream is best used for dry skin. If the patient suffers from itching, the doctor prescribes medications that contain hydrocortisone.
This is an antimicrobial component that perfectly removes itching and burning. Rapid acting antifungal medications are:
- Kanesten;
- Clotrimazole;
- Lamisil;
- Miconazole;
- Candide B and so on.
The combined drug Lotriderm effectively removes the symptoms of the disease and fights its causes. Broad-spectrum medications can be used without a doctor’s prescription, but they must be used in the specified dosage, because medications can create an allergic reaction that significantly aggravates the disease.
Doctors also advise changing ointments and creams every 14 days, as the body is likely to become addicted. The drug must be used until signs of the fungus are completely removed. It is necessary to smear the infected skin areas for 2 weeks after the symptoms have disappeared. This must be done to prevent re-occurrence of pathological bacteria.
Treatment with traditional methods
You can use traditional methods to treat interdigital fungus after consulting a doctor. Since sometimes infusions and compresses from medicinal herbs can cause an allergic reaction, and the factor of intolerance to the drug on an individual basis cannot be excluded.
Thumb fungus, which is treated with topical medications, can very quickly spread to other fingers, so timely help is a good opportunity to prevent the regressive process of the disease.
At home, you can use various compresses that are made on the basis of Burov's ointment. Why do you need to soak tampons in the solution and apply them to the infected areas? The application time of the compress should be no more than 25 minutes. For better effectiveness, you can wrap your feet in plastic bags to create a kind of vacuum.
In addition, the following are considered effective drugs in the fight against interdigital fungus:
- chamomile decoction;
- baby talc, it helps get rid of excessive sweating;
- soda solution;
- foot baths in a salt solution;
- compress of nettle and coltsfoot.
You can also use antifungal drugs at home, for example, Lamisil, Nizoral, and so on. But they can only help if the cream is chosen correctly. Only the attending doctor can choose the right drug.
In addition, after completion of treatment, it is necessary to disinfect all shoes that the patient wore during infection with the fungus. But if such a possibility exists, then it is better to buy new shoes to prevent re-infection with the fungus. Because it is quite difficult to remove pathogenic bacteria from shoes.
Disinfection occurs in this way: it is necessary to treat the surface inside the shoes with a 25% formaldehyde solution or 30% vinegar. Afterwards, the shoes are placed in a plastic bag for several hours. After this time, the shoes need to be aired to remove the smell of vinegar. It is not recommended to wash shoes.
If you have an interdigital fungus, then visits to the bathhouse or swimming pool should be cancelled. Otherwise, there is a chance of infecting other people with the disease.
In this case, it is necessary to protect family members from the shoes of an infected person. If there are small children in the house, then put it away in such a way that children cannot reach it.
There are statistics that indicate that if one family member becomes infected with a fungal disease on the feet, then in 80% of cases the rest of the family members are affected.
In order not to become infected with interdigital fungus, you need to follow simple rules that even small children can follow. In this case, the best preventive measure is to increase a person’s healthy immunity.
With the right approach, getting rid of dermatitis will not be difficult. Conventionally, all treatment of dermatitis can be divided into several parts.
As a rule, all traditional medicine methods based on getting rid of dermatosis involve creating lotions on areas affected by dermatitis.
If a fungus is detected on the surface of the skin, it is necessary to immediately disinfect all things with which the foot surface of the feet came into contact. It is better to throw away washcloths and old slippers immediately; treat the rest of the shoes from the inside with lemon juice, after removing the insoles. A similar procedure for prevention should be carried out weekly.
If the disease is not advanced, you can get rid of the fungus between your toes in a month. There are effective and proven ways to do this.
Medicinal ointments containing tolnaftate and miconazole are good for getting rid of fungi on the feet. These drugs include Clotrimazole ointment, which is used for two weeks, after which the ointment must be changed to avoid addiction. The drugs are used until the symptoms of fungus between the toes completely disappear, after which the ointment is used for prevention for two weeks.
To get rid of fungus on the big toe, use compresses from Burov's solution. To do this, a cotton swab is soaked in the solution, placed between the toes and held for twenty minutes.
An effective way to get rid of fungal infections is baking soda dissolved in water. Wipe the areas affected by fungal infection with a soda solution.
In addition to ointments and other medications, it is necessary to use special tablets that, when released into the blood, kill fungi. These drugs include Grisiovulfin, Nizoral and Lamisil.
Additionally, to restore the immune system, it is worth using vitamins and immunostimulating drugs - Thymogen, Taktivin and Levamisole.
To prevent the fungal infection from spreading, it is necessary to follow the rules of personal hygiene and take special care of the skin of your feet. It is important to wash your feet twice a day with tar soap, after which the skin between the toes should dry thoroughly - for this, use cotton swabs, disposable towels or a hairdryer.
After drying the skin of the legs, a medicinal antifungal ointment is applied to the affected areas - Desenex, Exoderil or Clotrimazole.
When wearing shoes, you should pay attention to open shoes that allow air to pass through well. For prevention, the inner surface of shoes is treated with formaldehyde or vinegar.
Shoes also require daily airing, preferably outdoors. We also recommend a special device for disinfecting shoes, which uses ultraviolet light to kill fungi and make shoes safe for frequent wear.
The special liquid “Samarovka”, which is sold in any pharmacies, is also popular. With its help, shoes should be thoroughly treated, placed in a sealed bag and kept for three hours.
Additionally, you should not allow your feet to get wet or sweat frequently. You need to wear socks made of natural fabric and change them regularly. If your feet sweat frequently, you can use foot powder. Only through careful monitoring of the condition of your feet and skin care will you be able to completely get rid of a fungal infection.
Folk remedies that have been proven over the years are effective and safe. These treatments for fungus between toes are inexpensive, accessible, and very simple. You can find out more in our article - toenail fungus - treatment.
Folk remedy No. 1
Strong tea with a volume of 50 milliliters is mixed with a tablespoon of 9% vinegar. Cotton swabs are dipped into the resulting solution and treated with them on the affected areas on the skin of the legs. The procedure is carried out several times during the day for several weeks until the fungus completely disappears.
Folk remedy No. 2
Glycerin from the bottle is poured into a half-liter jar, 70% vinegar is added to it in a ratio of 1 to 1. The jar is carefully closed and shaken so that the mixture is completely mixed. The fungus-infected surface is treated with this mixture.
Folk remedy No. 3
Sea salt baths are an effective remedy. After softening the skin in a saline solution, the skin between the toes is lubricated with celandine or aloe juice. Apple cider vinegar is also used instead of sea salt. The feet are immersed in the bath for fifteen minutes, after which they are treated with tea tree oil. Similar procedures should be done until the skin of the feet is completely cleared of fungus.
Salt effectively gets rid of fungal infections, so before going to bed, it is recommended to put on socks with salt poured inside. Additionally, the legs are steamed in the solution. Add one kilogram of salt and a teaspoon of soda to the water.
Mycosis of the foot (foot fungus) is an infectious disease caused by parasitic fungi and transmitted from person to person.
It should be noted that in the past, fungal skin infections were so common that only a small number of people managed to avoid infection. The situation changed dramatically in the 60-70s of the last century, when many effective medications became available, which not only brought relief to the patient, but also allowed recovery.
Today, the disease remains the most common skin disease, followed by ringworm.
With mycosis of the feet, the surface of the foot and the skin between the toes are often affected; in rare cases, the hands are involved in the pathological process. The latter is caused not so much by the spread of the fungus itself, but by the circulation of fungal toxins in the bloodstream.
In addition, additional infection of the hands is caused by scratching the skin of the legs, after which the parasitic agent can be transferred from the hands even to the scalp. This route of spread should be taken into account by patients with mycosis of the foot in order to protect not only themselves, but also those around them.
This is what skin affected by a fungus looks like
Mycosis of the feet is infection of the nails and skin of the foot by a parasitic fungus of various nature. Among all fungal diseases, this is the most common.
Below we will talk not only about the causes of the disease, but also about its treatment. Traditional methods of treatment are also used very widely.
Main causes of infection
External preparations designed to get rid of toenail fungus are represented by the following ointments:
- Kanizon is a product for topical use, available in the form of ointment, solution and cream. The active ingredient here is clotrimazole, which quickly destroys the cell membrane of the fungus. The ointment is applied to the entire surface of the finger, including the nail plate. This prevents the spread of infection over large areas.
- Mycospor is a cream and ointment with an antifungal effect. Perfectly neutralizes dermatophytes, yeast-like and mold fungi.
- Exoderil - most effectively copes with thumb fungus and eliminates rashes in other areas. The ointment is not absorbed into the blood, does not cause addiction, and there is no overdose of the active substance.
- Mycosan - a fungus on the toes when treated with this remedy disappears quite quickly. Positive changes are observed within 15 days after the start of therapy. The active substance here is ketoconazole, the action of which contributes to the destruction of the fungal structure and the destruction of enzymes. In addition, the drug has a certain peculiarity: it creates a film on the nail plate that performs protective functions even after the end of therapy.
Typically, skin diseases are treated in the following ways:
- Following a diet and proper nutrition, taking the necessary vitamins.
- Treatment with medications to boost the immune system.
- Use of antibiotics if the skin disease has become severe.
- External treatment with ointments and creams.
It is important to note that any treatment should begin only after the disease itself and its causes have been established by a specialist. So do not neglect visiting a doctor at the first symptoms of a skin disease.
Here you can read in detail how to treat foot fungus.
The choice of treatment methods is influenced by the cause that provoked the dermatitis. First of all, the root cause of the disease is eliminated.
But there are also generally accepted therapeutic methods for treating pathology, regardless of its characteristics.
Traditional medicine
A dermatologist must make the correct diagnosis and prescribe treatment. Most often, treatment is used with external preparations, i.e. various ointments, gels or nail polishes (they are used to treat fungus).
To alleviate unpleasant symptoms, you can resort to treatment with folk remedies, for example, make a foot bath with cool water with the addition of soda and salt, or wipe the affected areas of the skin with lemon juice.
An important factor is the disinfection of things that your feet come into contact with: slippers, shoes, stockings, socks, tights. To avoid relapse of the disease, it is important to treat the bathroom in a timely manner.
How to treat eczema on legs? This question remains relevant today, since each type of this disease has its own effective methods of therapy.
Dry eczema
Preventive actions
The main preventive measure is timely treatment of diseases that cause the appearance of trophic ulcers. You should also adhere to the following rules:
- abstaining from heavy physical work, especially for women;
- lead an active lifestyle;
- wear an elastic bandage during exacerbation of varicose veins;
- proper nutrition;
- giving up cigarettes and drinking alcohol;
- avoid injury;
- choose only comfortable shoes for everyday wear.
It should also be remembered that after complete recovery from the disease, reappearance is not uncommon. Therefore, it is important to follow your doctor's recommendations during the recovery period. Be sure to do therapeutic exercises to maintain blood vessels in a state of elasticity. And also treat the affected areas with moisturizers and bactericidal agents.